
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
Program Selection Criteria:
2023 Maternity Care
Released July 2023

2013 Benefit Design Capabilities Survey
®
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 1
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Document Overview
The Program Selection Criteria outlines the Quality, Business, and Cost of Care Selection Criteria and evaluation
processes used to determine eligibility for the Blue Distinction
®
Centers (BDC) for Maternity Care program (this
Program).
Sections of this document include:
1. Blue Distinction Centers for Maternity Care
2. Evaluation Process
3. Quality Evaluation
4. Quality Selection Criteria
5. Rationale For Required Selection Criteria
6. Quality Informational Measures
7. Business Selection Criteria
8. Cost of Care Selection Criteria
9. Cost of Care Evaluation
10. Appendix A: Obstetric Hemorrhage Patient Safety Bundle Elements
11. Appendix B: Severe Hypertension Patient Safety Bundle Elements
12. Appendix C: Safe Reduction of Primary Cesarean Births Patient Safety Bundle Elements
Blue Distinction Centers for Maternity Care
The BDC for Maternity Care program (Program) evaluates facilities (acute care hospitals, as well as children’s
hospitals) that offer maternity services for adult patients 18 years or older. This Program evaluates patient
outcomes and additional measures collected in the 2023 Maternity Care Provider Survey. Designation as a BDC for
Maternity Care differentiates facilities locally, as well as nationally, and includes two levels of designation:
• Blue Distinction Centers (BDC): Facilities recognized for their expertise in delivering specialty care.
• Blue Distinction Centers+ (BDC+): Facilities recognized for their expertise and cost-efficiency in
delivering specialty care.
Quality is key: only those facilities that first meet nationally established quality measures for BDC will be
considered for designation as a BDC+.
Designations are awarded to individual facilities (i.e., unique bricks-and-mortar facilities with unique addresses).
Any facility with multiple locations (different addresses) was evaluated separately for each location. Health
systems and other groups of multiple facilities/clinics are not designated collectively.
Evaluation Process
Blue Distinction Specialty Care programs establish nationally consistent and continually evolving approaches to
evaluating quality and value of care. The evaluation process include:

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 2
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Quality
A nationally consistent approach to evaluating quality and safety by incorporating quality measures with meaningful
impact, including care delivery system features and specific quality outcomes to which all can aspire.
Cost
A nationally consistent and objective approach for selecting BDC+ was used to address market and consumer
demand for cost savings and affordable healthcare.
Access
Blue members’ access to Blue Distinction Centers was considered to achieve the Program’s overall goal of
providing differentiated performance on Quality and, for the BDC+ designation, Cost of Care.
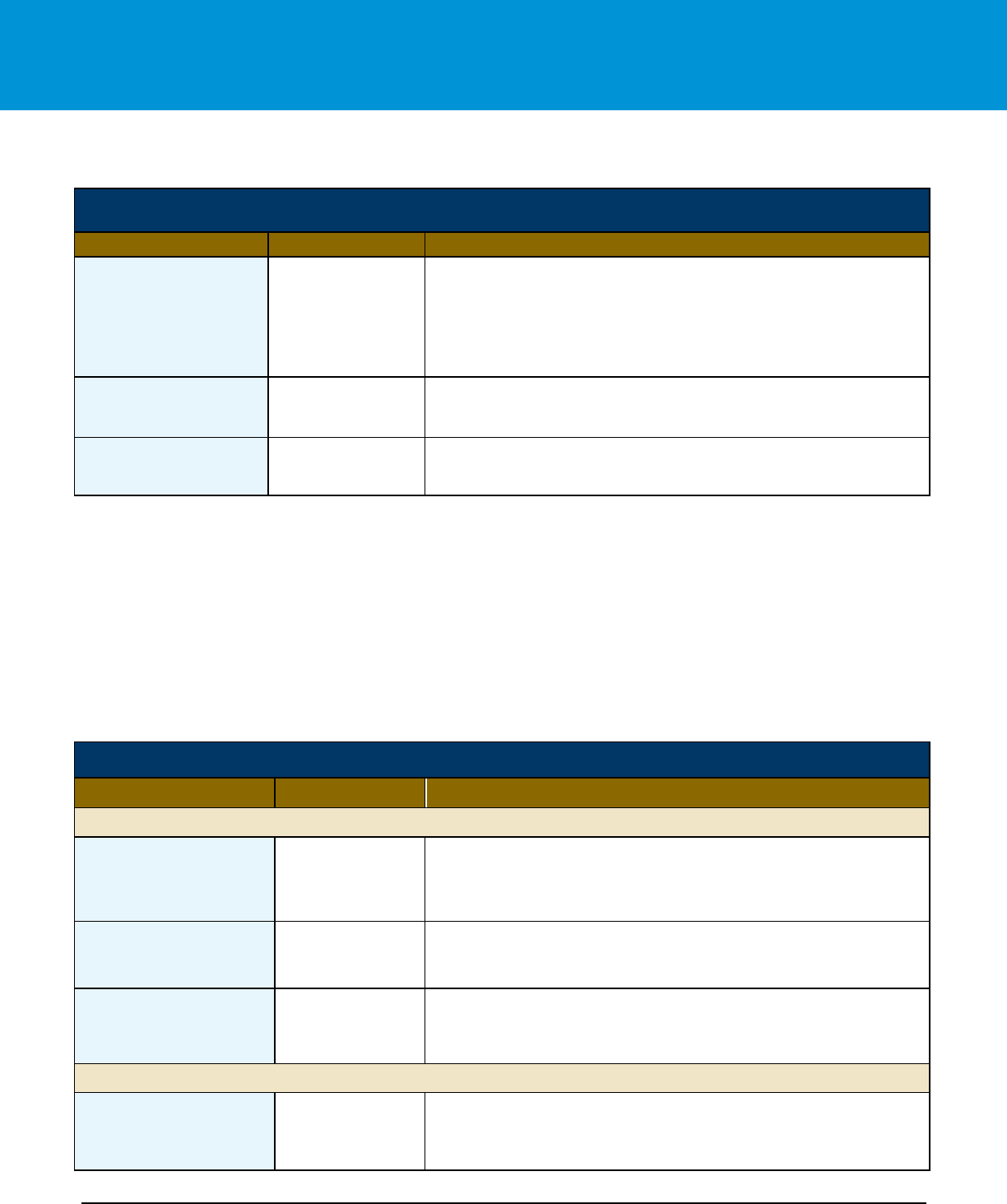
Data Sources
Objective data from the Provider Survey, Plan Survey, and National Blue Claims Dataset (Claims Data) information
were used to evaluate and identify facilities that meet the Program’s Selection Criteria. Table 1 below outlines the
data sources used for evaluation of this Program.
Table 1: Data Sources
Selection
Criteria
Components
Data Source
Blue
Distinction
Centers
(BDC)
Blue
Distinction
Centers+
(BDC+)
Quality
•
Quality data supplied by applicant facility in the Provider Survey
•
Local Blue Plan Quality Criteria (if applicable)
✓
✓
Business
•
Data supplied by Blue Plan in the Plan Survey
•
Review of Blue Brands Criteria
•
Local Blue Plan Business Criteria (if applicable)
✓
✓
Cost of Care
•
Blue Health Plan Claims Data
•
Local Blue Plan Cost Criteria (if applicable)
✓
Quality Evaluation
Blue Distinction Specialty Care programs establish a nationally consistent approach to evaluating quality and safety
by incorporating quality measures with meaningful impact. Selection Criteria continues to evolve through each
evaluation cycle, consistent with medical advances and measurement in this specialty area. The measurement
framework for this and other Blue Distinction programs were developed using the following guiding principles:
• Align with credible, transparent, nationally established measures with an emphasis on improved outcomes.
• Implement a nationally consistent evaluation approach.

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 3
Blue Distinction Centers for Maternity Care| Program Selection Criteria
• Include metrics that close clinical care gaps recognized as affecting longevity and quality of life and/or
contributing to higher spend.
• Evolve the selection criteria, consistent with medical advances and objective measures demonstrating
improved outcomes. by including elements of behavioral/mental health, virtual care, equity, and social
determinants of health (where applicable).
• Apply a fair and equitable evaluation approach that identifies facilities that meaningfully differentiate the
delivery of care.
Quality Measure Selection
Facilities were evaluated on quality measures developed through a process that included input from the medical
community and quality measurement experts, and review of medical literature. This process also included an
analysis of national quality and safety initiatives, and a thorough analysis of meaningful quality measures. Quality
Selection Criteria includes general facility structure and process measures, and patient outcome measures specific
to maternity care. The evaluation was based on facility responses to the Provider Survey for cases performed
during the most recent 12 months prior to submitting the Provider Survey.
The selected measures are joined into the final aggregate scoring model for evaluating facilities. The goal of the
program is to create a final aggregate model that provides differentiated performance on quality, while still providing
Blue Member access to designated facilities in each of the top 100 MSAs for Maternity Care.
Furthermore, Quality Selection Criteria scoring was based on a 90% lower confidence limit (LCL) of the outcome
measures, not on the actual point estimate (or rate) of the quality outcome measures. This benefits each facility by
taking potential measurement error into account, based upon statistical confidence predictions. If a facility’s LCL is
equal to or below the threshold, then that facility’s performance is the same or better than that threshold and that
facility would meet the quality scoring threshold for that measure; but if a facility’s LCL is above the threshold, that
indicates that the facility performance is worse than that threshold and that facility will not meet the quality scoring
threshold for that measure.
For accuracy, patient outcome measures were evaluated only if the analytic measure volume (measure
denominator) reported was greater than or equal to 11. If the reported analytic measure volume was less than 11,
then that patient outcome measure was not evaluated due to insufficient data.
Quality Selection Criteria
Quality Selection Criteria are outlined in Tables 2-4, below. Scoring of quality measures is based on both required
and flexible measures.
• Table 2 outlines required quality measures. The facility must meet ALL required measures.
• Table 3 outlines required patient outcome measures. The facility must meet ALL required measures.
• Table 4 outlines flexible measures. The facility must meet a specific number of measures within each of
three flexible measure categories:

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 4
Blue Distinction Centers for Maternity Care| Program Selection Criteria
1) Patient Outcome measures: Must meet 1 of 3 measures.
2) Patient Safety Bundles measures: Must meet 2 of 3 measures, and
3) Structure and Process measures: Must meet 2 of 4 measures.
Required Quality Measures
Table 2: Quality Measures (Required)
Table 2: Quality Selection Criteria: Required Measures
Facility must meet ALL measures
Measure Name
Data Source
Selection Criteria Description
National Accreditation
Provider Survey
Question #4
The facility is fully accredited by at least one of the following national
accreditation organizations:
• The Joint Commission (TJC) (without provision or condition) in the
Hospital Accreditation Program.
• Healthcare Facilities Accreditation Program (HFAP) of the
Accreditation Association for Hospital and Health Systems (AAHHS)
and is an acute care hospital. www.hfap.org.
• National Integrated Accreditation Program (NIAHO
SM
)—Acute Care of
DNV GL Healthcare.
• Center for Improvement in Healthcare Quality (CIHQ) in the Hospital
Accreditation Program.
Quality Improvement
Program
Provider Survey
Question #19
Facility has an internal quality improvement program to assess maternity
care.
Obstetric Hemorrhage
Provider Survey
Question #21
Facility uses a standardized, facility-wide, stage-based obstetric
hemorrhage emergency management plan, with checklists and an
escalation policy.
Provider Survey
Question #22
Facility has implemented ALL the following
elements of the Obstetric Hemorrhage Patient
Safety Bundle:
• Facility uses an evidence-based risk
assessment tool for hemorrhage risk at
defined stages of labor (prenatal, on
admission, pre-birth, and on transition to
postpartum care) for all patients.
• Facility measures cumulative quantitative
blood loss on all patients.
• Facility performs active management of the
3rd stage of labor (department-wide
protocol).
• Facility completes multidisciplinary reviews
for monitoring of outcomes and process
metrics (at least) for OBH cases resulting in
4 or more units of blood products and/or
SMM Indicator (as defined by CDC) by the
facility’s perinatal quality improvement (QI)
committee.
OR
Facility has
implemented at least
4 of the 6 bundle
elements.
(Refer to Appendix A
for a list of bundle
elements)

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 5
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Table 2: Quality Selection Criteria: Required Measures
Facility must meet ALL measures
Measure Name
Data Source
Selection Criteria Description
Severe Hypertension in
Pregnancy
Provider Survey
Question #23
Facility uses standardized protocols (with checklists and escalation
policies), which include a standardized response to maternal early
warning signs, listening and investigating patient-reported and observed
symptoms, and assessment of standard labs for the management of
patients with severe hypertension or related symptoms, as well as
obtaining appropriate consultation and maternal transport.
Provider Survey
Question #24
Facility uses standardized protocols (with checklists and escalation
policies) for management and treatment of severe hypertension,
eclampsia, seizure prophylaxis, and magnesium overdosage, as well as
postpartum presentation of severe hypertension/preeclampsia.
Provider Survey
Question #25
Facility has implemented ALL the following
elements of the Severe Hypertension in
Pregnancy Patient Safety Bundle:
• Facility has rapid access to standardized
medications used for severe
hypertension/eclampsia.
• Facility ensures accurate measurement and
assessment of blood pressure and initiates
treatment with antihypertensive.
medication(s) that are recommended to be
administered ASAP (preferably within 60
minutes of verification).
• Provides educational information, which
includes specific to warning signs/
symptoms of severe hypertension/
preeclampsia.
OR
Facility has
implemented 4 or
more of the 6
bundle elements.
(Refer to Appendix B
for a list of bundle
elements)
Safe Reduction of
Primary Cesarean Birth
Provider Survey
Question #26
Facility has implemented ALL the following
elements of the Safe Reduction of Primary
Cesarean Birth Patient Safety Bundle:
• Facility uses standardized methods in the
assessment of the fetal heart rate status,
including interpretation and documentation
based on National Institute of Child Health
and Human Development (NICHD)
terminology, and encourages methods that
promote freedom of movement.
• Facility upholds standardized induction
scheduling, to ensure proper selection and
preparation of women undergoing induction
of labor.
• Facility utilizes standardized evidence-
based labor algorithms, policies, and
techniques, which allow for prompt
recognition and treatment of labor dystocia.
• Facility adopts policies that outline
standardized management of Category II
fetal heart rate patterns and uterine
tachysystole.
OR
Facility has
implemented 5 or
more of the 8
bundle elements.
(Refer to Appendix C
for a list of bundle
elements)

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 6
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Table 2: Quality Selection Criteria: Required Measures
Facility must meet ALL measures
Measure Name
Data Source
Selection Criteria Description
Demographic Data
Collected
Provider Survey
Question #34
Facility collects the demographic data of race, ethnicity and spoken
language (REL) data preferred for healthcare during patient registration or
during a hospital visit.
System for Documenting
REL Data
Provider Survey
Question #35
Facility has an established system to document obtain self-reported race,
ethnicity, and primary language (REL) data directly from patients.
Drills for Serious
Adverse Maternal
Events
Provider Survey
Question #43
Facility holds drills or simulations for adverse maternal events.
Frequency of Drills for
Severe Adverse
Maternal Events
Provider Survey
Question #44
Facility holds drills or simulations AT LEAST every 12 months, or more
frequently.
PQC Involvement
Provider Survey
Question #47
Facility engages with its state Perinatal Quality Collaborative.
Prevention of Deep Vein
Thrombosis (DVT)
Provider Survey
Question #51
Facility routinely uses sequential compression devices (SCDs) for deep
vein thrombosis (DVT) prevention on patients at high risk for DVT.
Doulas
Provider Survey
Questions #53 and
#54
Facility employs doulas and/ or is supportive of participation by doulas in
labor support.
Local Blue Plan Quality
Criteria (if applicable)
Plan Survey
An individual Blue Plan, at its own independent discretion, may establish
and apply local quality requirements as additional Selection Criteria for
eligibility in a Blue Distinction Centers Program, for facilities located within
its Service Area.
Patient Outcome Measures (Required)
Facilities also must meet patient outcome measures for Maternity Care procedures, as reported in the Provider
Survey. Patient outcome measure evaluation requirements are outlined below in Table 3. For accuracy, a facility
must present sufficient data to meet the minimum analytic measure volume (measure’s denominator):
1) If the analytic measure volume is greater than or equal to 11, then then the patient outcome measure has
‘Sufficient Data’ for evaluation and the patient outcome measure will be evaluated.
2) If the analytic measure volume is less than 11, then the patient outcome measure has ‘Insufficient Data’
for evaluation, will not be evaluated, and the facility will not meet that measure.
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 7
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Table 3. Patient Outcome Measures (Required)
Quality Selection Criteria: Patient Outcome Measures (Required)
Facility must meet ALL measures
Measure Name
Data Source
Selection Criteria Description
Analytic Measure
Volume
Provider Survey
Questions #12, #13
and #16
Facility’s analytic measure volume is greater than or equal to 11 for the
following measures:
• PC-01 Elective Delivery Denominator
• PC-02 Cesarean Section Denominator
• Episiotomy Denominator (Measure is evaluated in the Patient
Outcome Measures Flexible criteria, outlined below in Table 4)
PC-01
Elective Delivery
Provider Survey
Question #12
Rate of patients delivering newborns with >=37 and <39 weeks gestation
completed lower confidence level (LCL) must be less than or equal to
4.00%.
PC-02
Cesarean Section
Provider Survey
Question #13
Rate of Nulliparous Patients who delivered a live term singleton newborn
in vertex presentation via cesarean section lower confidence level (LCL)
must be less than or equal to 24.00%
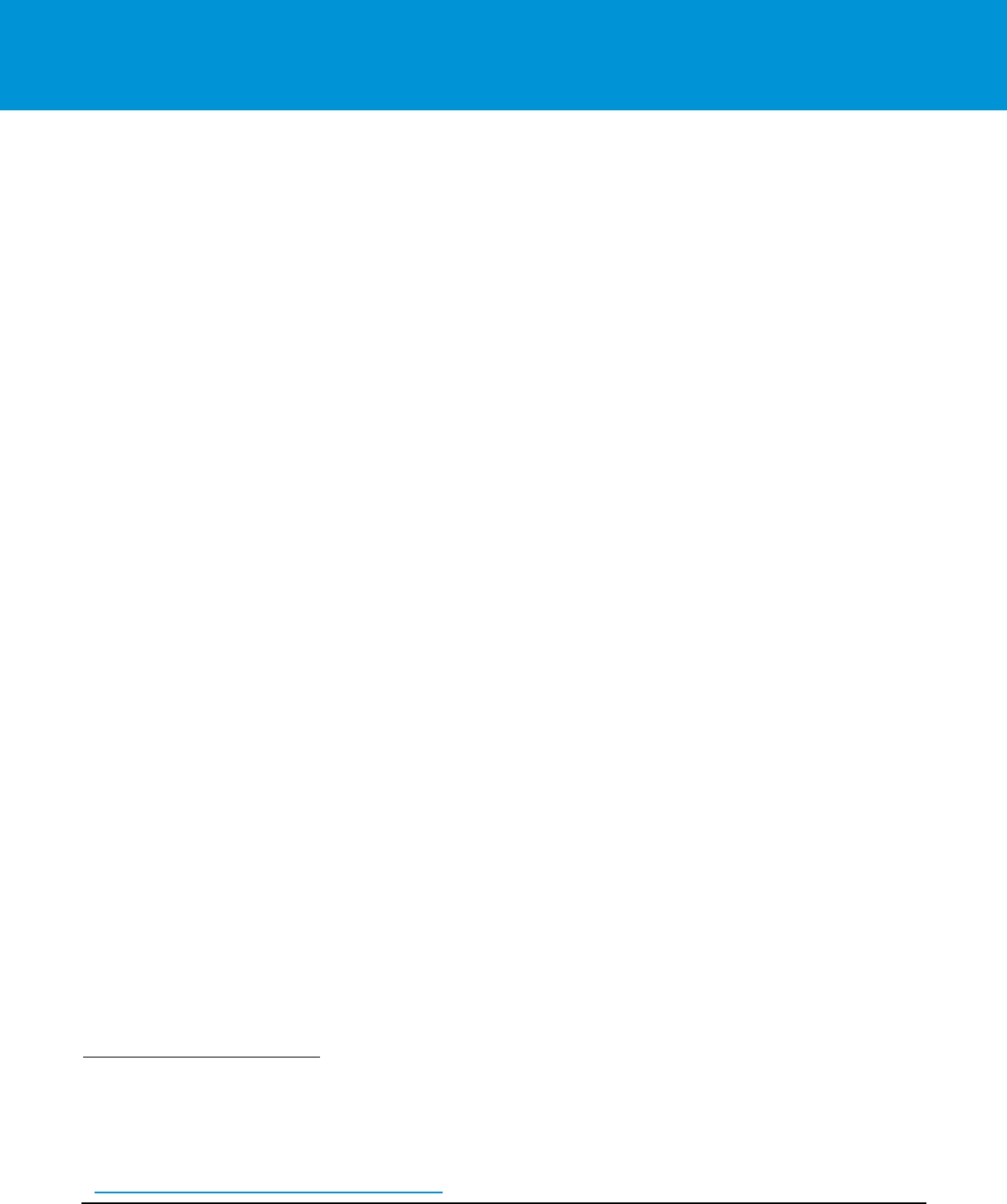
Flexible Measures – Structure/ Process and Patient Outcome Measures
Required flexible measures are grouped into 3 categories, shown in Table 4:
• Patient Outcomes Measures Facility must meet 1 of 3 measures
• Patient Safety Bundles Measures Facility must meet 2 of 3 measures
• Structure and Process Measures Facility must meet 2 of 4 measures
Table 4: Flexible Measures
Quality Selection Criteria: Flexible Measures
Measure Name
Data Source
Selection Criteria Description
Patient Outcome Measures Flexible Category: Must Meet 1 out of 3 Measures
Episiotomy Rate
Provider Survey
Question #16
Percent of women who received an episiotomy during a vaginal birth
lower confidence limit (LCL) must be less than or equal to 5.00%
Measure denominator must be at least 11 procedures for the measure to
be evaluated, explained above in Table 2.
PSI 18 (Obstetrical
Trauma with Instrument)
Provider Survey
Question #17
Hospital discharges with third- and fourth-degree obstetric traumas with
instrument-assisted vaginal deliveries lower confidence level (LCL) must
be less than or equal to 11.72% (AHRQ).
PSI 19 (Obstetrical
Trauma without
Instrument)
Provider Survey
Question #18
Hospital discharges with third- and fourth-degree obstetric traumas
without instrument-assisted vaginal deliveries lower confidence level
(LCL) must be less than or equal to 1.75% (AHRQ).
Patient Safety Bundles Measures Flexible Category: Must Meet 2 out of 3 Measures
Care for Pregnant and
Postpartum People with
Substance Use Disorder
Provider Survey
Question #27
Facility assesses all pregnant women for substance use disorders
(SUDs), using validated screening tool(s) to identify drug and alcohol use;
and incorporates a screening, brief intervention, and referral to treatment
(SBIRT) approach, in the maternity care setting.

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 8
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Quality Selection Criteria: Flexible Measures
Measure Name
Data Source
Selection Criteria Description
Postpartum Discharge
Transition
Provider Survey
Question #29C
Facility screens all patients for Post-Partum Depression prior to discharge
(using the Edinburgh Postnatal Depression Screen or another
standardized tool) and establishes a system of support and follow-up
within 30 days for those who screen positive.
Sepsis in Obstetrical
Care
Provider Survey
Question #30
Facility uses standardized protocols with checklists and escalation
policies (including a standard response to maternal early warning signs,
listening, investigating patient-reported and observed symptoms, and
assessment of standard labs for the management of patients with
symptoms of sepsis) and obtain critical care consult and transfers patients
when necessary.
Structure and Process Measures Flexible Category: Must Meet 2 out of 4 Measures
Frequency of Data
Sharing
Provider Survey
Question #20
Facility shares personal rates of maternal quality measures with OB
providers at least annually.
Unconscious Bias
Training
Provider Survey
Question #42
Facility has implemented trauma-informed protocols and anti-racist
training (unconscious bias/ respectful and equitable care) to address
healthcare team member biases and stigmas.
Physicians at Drills/
Simulations
Provider Survey
Question #45
Facility requires physicians (both privileged and hospital-based) who
provide obstetric care at your facility to participate in serious maternal
adverse event drills and/or simulations.
Ongoing Education and
Training
Provider Survey
Question #46
Facility requires ongoing (at least every 2 years) physician and nursing
education/ training of fetal heart rate monitoring, obstetric hemorrhage
management and severe hypertension in pregnancy management.
Rationale for Required Selection Criteria
The selection criteria chosen for the 2023 BDC Maternity Care Program places a renewed focus on the need for
improved maternity services, in alignment with the BCBS National Health Equity Strategy and the goal of reducing
racial disparities in maternal health by 50% in 5 years. Nationwide efforts have been put into place to address the
maternal health crisis in the United States. Severe maternal morbidity, which includes unexpected complications in
labor and delivery that result in significant short-term or long-term consequences to a women’s
1
health, has been
increasing and affects thousands of women in the United States each year. The selection criteria for the Maternity
Care Program aligns with actionable approaches recommended by organizations such as the Department of Health
and Human Services (HHS), American College of Obstetricians and Gynecologists (ACOG), Alliance for Innovation
on Maternal Health (AIM), and the California Maternal Quality Care Collaborative (CMQCC), to enhance outcomes
and reduce adverse events in maternal health care. The following categories offer background information and
suggestions for improvement on each of the required selection criteria, where applicable.
1
Throughout this document, the terms “mother,”” maternal,”” she” or “her” refer to a person who is pregnant, has given birth or is in the postpartum stage of
pregnancy. We recognize that not all people who have been pregnant or given birth identify with these terms, and that all people deserve to receive safe, equitable
healthcare.

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 9
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Quality Improvement Program
Having a robust quality improvement (QI) program is instrumental to making positive changes at the facility and
must be an organizational priority. Administrative support, staff involvement, and a multidisciplinary team are the
backbone of effective quality improvement programs. Facility and provider engagement should include data
collection, analysis, and data sharing to identify issues; focus on improvements when things go wrong; incorporate
evidence-based practices and standardized protocols to close gaps in care for all mothers; and have a commitment
to high reliability performance for ongoing quality improvement.
2
Patient Safety Bundles
Patient safety bundles have been developed by maternal health experts, to provide guidance on the
implementation and quality improvement efforts related to PREVENTABLE obstetric conditions that have a direct
correlation to severe maternal morbidity and mortality. AIM Patient Safety Bundles are based on five (5) major
components: Readiness; Recognition and Prevention; Response; Reporting and Systems Learning; and
Respectful, Equitable, and Supportive Care. Following these evidence-based actions, with defined rationales,
allows facilities to be prepared for adverse maternal complications and to improve maternal outcomes. Similarly,
CMQCC has developed toolkits for several obstetric emergencies and disorders, which outline research and
evidence-based practices that facilities can use to improve outcomes. Standardization of protocols and checklists,
using evidence-based practices, are vital in reducing patient harm, thanks to consistency and reliability of a process
that will apply to most patients.
3
,
4
Both AIM and CMQCC also provide suggestions and guidance for quality
improvement projects specific to each topic.
Recently, AIM Patient Safety Bundles and CMQCC toolkits have begun to include actionable steps that facilities
can take to provide more equitable maternal healthcare, as well as to address maternal mental health with the
incorporation of trauma informed care. Traumatic birth experiences can come from any unexpected outcome –
ranging from an unintended cesarean birth to obstetric complications, such as obstetric hemorrhage leading to
hysterectomy. As self-harm resulting from mental health conditions has been determined to be one of the top
causes of maternal mortality
5
, maternity care providers should be educated on how to identify trauma and
implement strategies to reduce the risk of re-traumatization, while providing care that offers patients a sense of
safety
6
. AIM also released a new maternal mental health tool kit recently, which facilities should review and
implement to prevent potential gaps in care, Perinatal Mental Health Conditions | AIM (saferbirth.org).
Although not part of the required selection criteria for the 2023 BDC Maternity Care Program, AIM Cardiac
Conditions in Pregnancy Bundle may become required in future Maternity Care evaluation cycles. Facilities should
take time to review the bundle and initiate implementation of a Cardiac Conditions screen and a standardized
protocol for managing maternal cardiac conditions when they are identified. CMQCC has developed an algorithm
2
BCBS National Health Equity Strategy: Maternal Health Compendium and Workbook, Blue Cross Blue Shield Association, April 2021
3
Clinical guidelines and standardization of practice to improve outcomes. ACOG Committee Opinion No. 792. American College of Obstetricians
and Gynecologists. Obstet Gynecol 2019;134: e122–5.
4
The use and development of checklists in obstetrics and gynecology. Committee Opinion No. 680. American College of Obstetricians and
Gynecologists. Obstet Gynecol 2016;128: e237–40
5
Pregnancy-Related Deaths: Data from Maternal Mortality Review Committees in 36 US States, 2017–2019 | CDC
6
Caring for patients who have experienced trauma. ACOG Committee Opinion No. 825. American College of Obstetricians and Gynecologists.
Obstet Gynecol 2021;137: e94–9

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 10
Blue Distinction Centers for Maternity Care| Program Selection Criteria
for cardiovascular disease assessment in pregnant and postpartum women with recommendations for interventions
and referrals, when necessary.
7
Each of the required Patient Safety Bundles For Safer Birth | AIM are outlined below, with actionable items
highlighted that facilities should consider implementing on a priority basis, if they are not in place already .
Obstetric Hemorrhage
In the event of obstetric hemorrhage, early recognition is essential to successfully manage the hemorrhage. This
starts with using an evidence-based risk assessment tool upon admission to labor and delivery and upon admission
to postpartum, at minimum. Quantifying blood loss is a simple process facilities can have in place to measure a
mother’s blood loss, before, during, and for up to 24 hours after birth, or when clinically indicated. Pregnancy
doubles a woman’s blood volume, allowing her to lose almost 1 liter of blood before she starts to show clinical signs
and symptoms of hypovolemia. If obstetric hemorrhage is not recognized before that point, it is even more difficult
to manage. Utilizing standardized protocols and emergency checklists with the actio n items identified in the
Obstetric Hemorrhage patient safety bundle and toolkit will allow for effective management of the hemorrhage. A
facility should consider reviewing any case of hemorrhage in which the patient receives 4 or more liters of blood
products as part of their Quality Improvement program to determine opportunities for improvement and celebrate
the successes noted.
8
,
9
,
10
Severe Hypertension in Pregnancy
To recognize severe hypertension in pregnancy, facilities must first ensure that maternal care providers
understand how to measure blood pressure correctly, being sure to consider the patient’s physical position, recent
drug or medication use, and psychosocial status. Not identifying these factors (or identifying them incorrectly) can
lead inaccurate blood pressure assessment. Using standardized protocols and checklists with the action items in
the Severe Hypertension in Pregnancy patient safety bundle and toolkit, the facility should treat any sustained
blood pressure (≥160/≥110) quickly, regardless of the perceived reason for the severe range blood pressure.
Timely treatment from the second severe range blood pressure to the administration of antihypertensive
medication is data that would be beneficial for a facility to collect and then use to develop an appropriate
performance improvement plan for, if necessary.
11
,
12
,
13
7
Afshan B. Hameed, Christine H. Morton, and Allana Moore. Improving Health Care Response to Cardiovascular Disease in Pregnancy and Postpartum Developed
under contract #11-10006 with the California Department of Public Health, Maternal, Child and Adolescent Health Division. Published by the California Department of
Public Health, 2017, Cardiac Conditions in Obstetric Care | AIM (saferbirth.org)
8
Lagrew D, McNulty J, Sakowski C, Cape V, McCormick E, Morton CH. Improving Health Care Response to Obstetric Hemorrhage, a California Maternal Quality
Care Collaborative Toolkit, 2022
9
Quantitative blood loss in obstetric hemorrhage. ACOG Committee Opinion No. 794. American College of Obstetricians and Gynecologists. Obstet Gynecol
2019;134: e150–6
10
Obstetric Hemorrhage | AIM (saferbirth.org)
11
Druzin M, Shields L, Peterson N, Sakowski C, Cape V, Morton C. Improving Health Care Response to Hypertensive Disorders of Pregnancy,
a California Maternal Quality Care Collaborative Quality Improvement Toolkit, 2021
12
Severe Hypertension | ACOG
13
Severe Hypertension in Pregnancy | AIM (saferbirth.org)
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 11
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Safe Reduction of Primary Cesarean Birth
Cesarean birth is necessary at times, for the mother and/or baby’s safety. Unfortunately, cesarean births also occur
frequently when they are not necessary, needlessly increasing a woman’s risk of complications (such as
hemorrhage and infection) and putting her at risk for complications (such as uterine abruption and placenta accreta
spectrum in future pregnancies). Standardized induction protocols and labor admission processes/rules should be
in place to decrease mothers’ need for medical intervention to progress labor. As ACOG recommends, supporting
natural labor progress, with actions such as intermittent fetal heart rate monitoring, ambulation, and frequent
position changes, can improve a mother’s chance at a successful vaginal birth.
14
When slow labor progress or fetal
intolerance to labor is a concern, utilizing evidence-based algorithms from CMQCC can guide maternal care
providers to accurately diagnose labor dystocia and manage category II fetal heart rate tracings.
Although not a requirement of the 2023 BDC Maternity Care Program, it is of interest to consider employment
models for certain maternity care providers and their effect on maternal outcomes. Research has shown that
facilities whose care model includes Obstetric Hospitalists, Certified Nurse Midwives and/or doulas have better
outcomes, including lower cesarean birth rates, than those who use traditional employment models. These care
models offer an alternative to on-call requirements, which may surpass 24 hours at a time, leading to exhaustion
and a greater risk of medical error.
15
Utilizing obstetric hospitalists, CNMs, and/or doulas allows patients to receive
care from provider(s) who are more available and can offer greater labor support and patience than one who needs
to multitask office responsibilities, operative cases, and other laboring patients.
Facilities should review cases regularly for primary cesarean births and the causes attributed to them, comparing
the care documented to evidence based practices outlined by AIM and CMQCC, while looking fo r trends and
opportunities that may need to be addressed. Cesarean birth rates should be shared with the facility’s providers to
create awareness of the need for cesarean reduction and the leading contributors for potentially avoidable
cesarean births.
16
,
17
,
18
Care for Pregnant and Postpartum People with Substance Use Disorder Abuse
Screening every pregnant patient for substance abuse is the first step a facility can take to addressing substance
use disorder (SUD). Screening (with a validated verbal assessment tool), then providing Brief Intervention and a
Referral to Treatment (together, SBIRT) is an evidence-based tool that facilities can implement to identify patients
with SUD and then provide the resources and interventions necessary to improve outcomes for both mother and
infant. Management of SUD in pregnancy and postpartum can be challenging and requires collaboration with a
multidisciplinary team of SUD specialists to care for the mother properly and to keep her safe, both during
14
Approaches to limit intervention during labor and birth. ACOG Committee Opinion No. 766. American College of Obstetricians and Gynecologists. Obstet Gynecol
2019;133: e164–73
15
The obstetric and gynecologic hospitalist. Committee Opinion No. 657. American College of Obstetricians and Gynecologists. Obstet Gynecol 2016;127: e81–5.
16
Smith H, Peterson N, Lagrew D, Main E. 2016. Toolkit to Support Vaginal Birth and Reduce Primary Cesareans: A Quality Improvement Toolkit. Stanford, CA:
California Maternal Quality Care Collaborative
17
Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1. American College of Obstetricians and Gynecologists. Obstet Gynecol 2014;
123:693–711.
18
Safe Reduction of Primary Cesarean Birth | AIM (saferbirth.org)

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 12
Blue Distinction Centers for Maternity Care| Program Selection Criteria
hospitalization and after discharge. Quality improvement topics may include ensuring that screening is completed
on all mothers, with follow through using evidence-based guidelines when a positive screen is identified.
19
,
20
,
21
Postpartum Discharge Transition
Discharge home after childbirth can be incredibly challenging for many families. Signs and symptoms of obstetric
complications can often be dismissed while caring for a new human and coping with fatigue and postpartum mood
changes. Facilities should develop guidelines for discharge teaching, with criteria for discharge to home and
coordinated care for follow up visits. Screening for comorbidities and social determinant of health concerns, such as
food insecurity and unstable housing, will allow maternity care providers to identify concerns and coordinate
appropriate follow up care and resources for the patient. Discharge teaching of post birth warning signs for the most
common obstetric complications, using tools such as a those developed by the Association of Women’s Health,
Obstetric and Neonatal Nurses (AWHONN)
22
, should be available in multiple languages and written with health
literacy in mind. Health education is essential in empowering mothers to speak up for themselves when they feel
something is not right and these tools can have a direct impact on maternal mortality and morbidity in the
postpartum period. Quality improvement plans might include assessing readmission rates for mothers who present
to the Emergency Department and are readmitted to the facility within 30 days of discharge, to provide insight into
trends of postpartum complications at your facility and to put a plan in place to reduce readmissions.
23
,
24
,
25
Sepsis in Obstetrical Care
Facilities should have a maternity specific sepsis protocol in place. Maternity care providers must have a clear
understanding of the difference in clinical features of sepsis between the pregnant and non-pregnant patient. Using
evidence-based guidelines provided by organizations such as AIM and CMQCC will direct maternity care providers
how to identify sepsis properly, based on laboratory values and risk factors specific to the pregnant or postpartum
patient, and how to manage the patient’s care if sepsis is diagnosed. CMQCC’s toolkit offers algorithms that
clinicians can use in their management of sepsis. Prompt recognition and initiation of treatment is necessary for
improving outcomes. Any case of confirmed sepsis also should be reviewed by the facility to determine
opportunities for improvement and to reduce the incidence of sepsis in the future.
26
Demographic Data Collection
Collecting self-reported demographic data (race, ethnicity, spoken language) is the first step facilities can take to
reduce racial disparities in healthcare. Facilities can use the data collected to stratify quality measures and make
changes to policies, procedures, patient safety goals and quality improvement goals to address equity. An
19
Opioid use and opioid use disorder in pregnancy. Committee Opinion No. 711. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;130:
e81–94
20
Crew E, Chowfla A, DuPlessis H, Lee H, Main E, McCormick E, Oldini C, Smith H, Robinson R, Waller C, Wong J. Mother and Baby Substance Exposure Toolkit.
Stanford, CA: California Maternal Quality Care Collaborative and California Perinatal Quality Care Collaborative. 2020. Acces sed from https://nastoolkit.org/.
21
Care for Pregnant and Postpartum People with Substance Use Disorder | AIM (saferbirth.org)
22
POST-BIRTH Warning Signs Education Program – AWHONN
23
Optimizing postpartum care. ACOG Committee Opinion No. 736. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131: e140–50
24
Stuebe, Alison M. MD, MSc; Kendig, Susan JD, WHNP-BC; Suplee, Patricia D. PhD, RNC-OB; D'Oria, Robyn MA, RNC. Consensus Bundle on Postpartum Care
Basics: From Birth to the Comprehensive Postpartum Visit. Obstetrics & Gynecology 137(1): p 33-40, January 2021. | DOI: 10.1097/AOG.0000000000004206
25
Importance of social determinants of health and cultural awareness in the delivery of reproductive health care. ACOG Committee Opinion No. 729. American
College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131: e43–8
26
Gibbs R, Bauer M, Olvera L, Sakowski C, Cape V, Main E. Improving Diagnosis and Treatment of Maternal Sepsis: A Quality Improvement Toolkit. Stanford, CA:
California Maternal Quality Care Collaborative

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 13
Blue Distinction Centers for Maternity Care| Program Selection Criteria
intervention as simple as communicating in a patient’s preferred language can increase trust, satisfaction and
improve outcomes.
27
Drills and Simulations for Adverse Maternal Events
Obstetric emergencies happen, and periodic drills and simulations improve the facility’s response and outcomes
when they do. Drills and simulations should follow established protocols and standardized interventions, using a
strategy that emphasizes effective communication, such as TeamSTEPPS, and include a multidisciplinary team,
requiring physicians, nurses, nursing assistants, and other care providers from all potentially involved departments
(anesthesiology, blood bank, pharmacy etc.) to attend. Resources for drills and simulations can be found with the
AIM Patient Safety Bundles and the CMQCC toolkits. Readiness is a core principle of patient safety bundles and
preparing for obstetrical emergencies allows faster and improved response along, with improved patient outcomes
by team members’ knowledge of designated roles, access to emergency supplies, effective communication, and
ongoing education and training.
28
Perinatal Quality Collaborative Involvement
Perinatal Quality Collaboratives (PQC) consist of maternal and neonatal health experts that develop initiatives
aimed at improving the quality of care for mothers and babies. PQCs assist facilities in implementing performance
improvement plans consisting of evidence-based practices and data collection targeted at an identified gap in
maternity care practices. Involvement with the applicable state’s PQC provides each facility with not only the
resources and expertise to be successful in improving outcomes, but also a community of support and
encouragement to maintain a path to continuous improvement.
29
Doulas
While hospital employed doulas may not be feasible everywhere, supporting their involvement during labor and
delivery is. Doulas do not have formal obstetric training; they are trained, however, to provide emotional, physical,
informational and resource support through pregnancy and into the postpartum period. Collaboration between all
maternity care providers and doulas within a facility not only enhances the patient experience, but also has been
shown to reduce cesarean birth rates and to lower incidences of maternal complications – which is why ACOG
reports that continuous labor support by a doula is “one of the most effective tools to improve labor and delivery
outcomes.”
30
Doulas also reduce racial disparities in maternal care, by serving as patient advocates for minority
groups – especially in the hospital setting, where mistrust of maternity care providers can exist. Doulas empower
patients to make the best personal decision for themselves and their babies by helping them to understand and
interpret what is happening to them in the hospital environment. Facilities are encouraged to assess their
relationships with doulas and determine an action plan to incorporate doulas as valuable members of their
maternity care team.
31
27
Makoul G, Donohue R, England W, Gorley T. 2023 Experience Perspective. NRC Health. https://nrchealth.com/resources (Accessed 05/31/2023)
28
Preparing for clinical emergencies in obstetrics and gynecology. Committee Opinion No. 590. American College of Obstetricians and Gynecologists. Obstet
Gynecol 2014; 123:722–5
29
Perinatal Quality Collaboratives | Perinatal | Reproductive Health | CDC
30
Safe prevention of the primary cesarean delivery. Obstetric Care Consensus No. 1. American College of Obstetricians and Gynecologists. Obstet Gynecol 2014;
123:693–711
31
Smith H, Peterson N, Lagrew D, Main E. 2016. Toolkit to Support Vaginal Birth and Reduce Primary Cesareans: A Quality Improvement Toolkit. Stanford, CA:
California Maternal Quality Care Collaborative. pp 102-105
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 14
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Unconscious Bias Training
Unconscious bias refers to attitudes and stereotypes held towards others that affect our understanding, actions,
and decisions in an unconscious manner.
32
Reducing racial disparities is another way that facilities can improve
maternal health outcomes. Research has proven that Black and Hispanic women experience higher rates of
childbirth complications, regardless of age or geographic location.
33
Unconscious bias and lack of cultural humility
and awareness can lead to unintended, but unequal treatment of patients from racial and ethnic minorities or from
marginalized social groups.
34
Unconscious bias training helps maternity care providers to recognize their own
biases and to understand how and why to deliver safe, equitable care to all patients. Standardization of protocols
and processes also ensures that the same care is provided to every patient, every time.
Regardless of their designation eligibility status, all applicant facilities should use the 2023 Maternity Care Provider
Survey results as a guide to improve care and to identify gaps in their Maternity Programs for which performance
improvement plans may be necessary. The structure and process measures highlighted in the survey have all been
correlated to improvements in maternal health outcomes and racial disparities. In the future, these elements and
more will be required for designation. Our Program recommends that facilities look closely at their own maternity
programs and develop a strategy for addressing the opportunities for improvement that they identify. As a next
step, BCBSA will begin working closely with Blue Plans, as they encourage facilities to implement performance
improvement activities that will enhance their maternity care programs and patient outcomes.
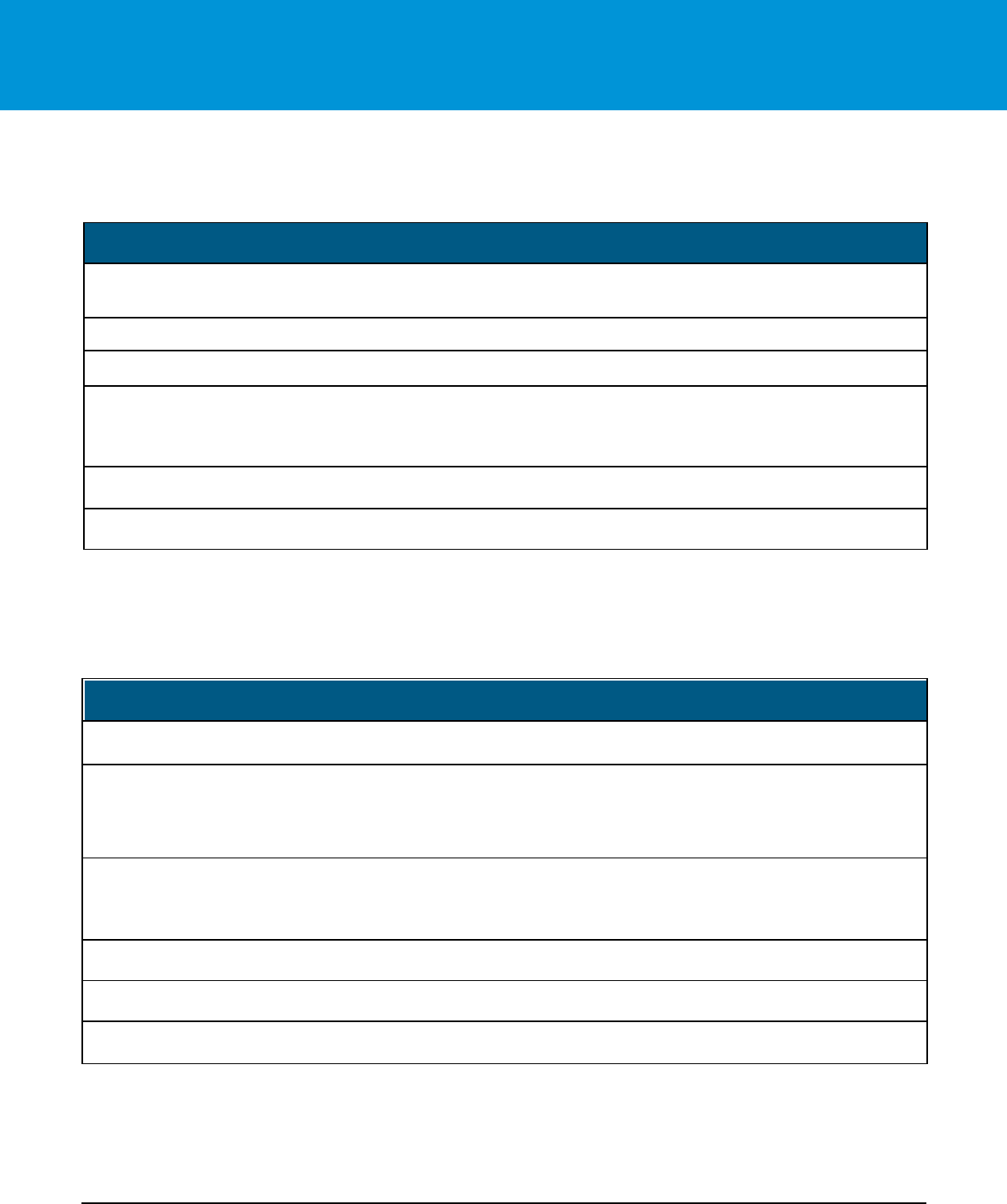
Quality Informational Measures
The informational measures outlined in Table 5 were included in the Provider Survey. These measures were not
scored but used as an educational tool for quality improvement. These informational measures may become
required Quality selection criteria, in future Program evaluation cycles.
Table 5: Informational Measures
Informational Measures
Not Scored
Measure Name
Source
Selection Criteria Description
The Joint Commission’s
(TJC) Perinatal Care
Certification or Advanced
Perinatal Care Certification
Provider Survey
Question #5
Facility has either attained, not attained, is in process of attaining or is not
in the process of attaining, TJC Perinatal Care Certification or Advanced
Perinatal Care Certification.
Centers for Medicare and
Medicaid Services’
Birthing-Friendly Hospital
Designation
Provider Survey
Question #6
Facility participates in a structured state or national Perinatal Quality
Improvement (QI) Collaborative and/or has implemented patient safety
practices or bundles as part of these CMS Birthing Friendly Designation QI
initiatives.
TJC/ American College of
Obstetricians and
Gynecologists (ACOG)
Provider Survey
Question #7
Facility has attained, is in process of attaining, or is not in the process of
attaining, a TJC/ACOG Levels of Care verification between I and IV.
32
Quick Safety Issue 23: Implicit bias in health care, the Joint Commission.
33
Racial Disparities in Maternal Health, Blue Cross Blue Shield Association Health of America Report, May 2021.
34
Implicit bias in health care professionals: a systematic review, Chloë FitzGerald, Samia Hurst, BMC Med Ethics. 2017.

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 15
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Informational Measures
Not Scored
Measure Name
Source
Selection Criteria Description
Levels of Care Verification
Program
Centers for Disease Control
and Prevention’s Levels of
Care Assessment Tool
(CDC LOCATe
SM
)
Provider Survey
Question #8
Facility has attained, has not attained, or is not in the process of attaining a
CDC LOCATe
SM
) Level of Care determination between Level I and Level
IV.
PC-02 Cesarean Section for
the past 24 months
Provider Survey
Question #14
Facility reports PC-02 Cesarean Delivery rates for the most recent 24
months, if available.
PC-07 Severe Obstetric
Complications
Provider Survey
Question #15
Facility reports PC-07 Severe Obstetric Complications rate, if available.
Cardiac Conditions in
Obstetric Care
Provider Survey
Question #32
and #33
Facility has implemented a standard protocol (with checklists and
escalation policies) for management of cardiac symptoms and conditions,
which includes multidisciplinary consultation and maternal transport when
necessary and has trained obstetric care providers to perform a basic
Cardiac Conditions Screen.
Patient Perception of Care
Provider Survey
Question #41
Facility collects information regarding patient perception of care (including,
but not limited to the patient’s perception of receiving unbiased, respectful
healthcare).
Postpartum Contraception
Provider Survey
Question #48
Facility provides postpartum women with access to placement of Long -
Acting Reversible Contraceptives (LARCs) with-in 3 days of birth.
Post-Birth Warning Signs
Provider Survey
Question #49
Facility has implemented the Association of Women’s Health , Obstetric and
Neonatal Nurses (AWHONN’s) Post-Birth Warning Signs for patient
discharge education.
Enhanced Recovery after
Cesarean Surgery
Provider Survey
Question #50
Facility has implemented Enhanced Recovery After Surgery (ERAS)
protocols for cesarean birth patients.
Navigator/ Support
Program
Provider Survey
Question #52
Facility offers an Obstetric Nurse Navigator program (or similar program),
which facilitates the mother’s access to pregnancy education, self-care,
and support systems (such as doulas).
Birthing Center
Provider Survey
Question #55
Facility is affiliated with a birthing center, either attached to or detached
from the facility.
Obstetric Hospitalists/
Laborists
Provider Survey
Question #56
Facility employs obstetric hospitalists/ laborists.
Business Selection Criteria
The Business Selection Criteria consists of the following components:
• Facility Performs Services
• Facility Preferred Provider Organization (PPO) Participation;
• Blue Brands Criteria; and
• Local Blue Plan Business Criteria (if applicable)

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 16
Blue Distinction Centers for Maternity Care| Program Selection Criteria
A facility must meet ALL components listed below in Table 6 to meet the Business Selection Criteria for the Blue
Distinction Centers for Maternity Care designation.
Table 6. Business Selection Criteria
Business Selection Criteria
Facility Performs Services
Facility must perform maternity care services.
Facility PPO Participation
Facility must participate in the local Blue Plan’s BlueCard
®
Preferred Provider
Organization (PPO) network.
Blue Brands Criteria
Facility and its corporate family meet BCBSA criteria for avoiding conflicts with BCBSA
logos and trademarks.
Local Blue Plan Business
Criteria (if applicable)
An individual Blue Plan, at its own independent discretion, may establish and apply
local business requirements as additional Selection Criteria for eligibility in a Blue
Distinction Centers program, for providers located within its Service Area.
Note: Physician participation in the local Blue Plan’s PPO Network is not part of the Selection Criteria and evaluation for the
Program at this time but will become a requirement in the next evaluation cycle. Blue Cross Blue Shield and Local Blue
Plans believe that all patients should be protected from surprise medical bills. We are strongly committed to working with policy
makers, hospitals, and physicians on solutions to better protect consumers while preventing unintended costs an d disruptions to
the healthcare system.
Cost of Care Selection Criteria
In addition to meeting the Program’s nationally established, objective Quality and Business Selection Criteria for
BDC, facilities must meet ALL requirements of the following Cost of Care Selection Criteria in Table 7 to be
considered eligible for the BDC+ designation.
Table 7. Cost of Care Selection Criteria
Cost of Care Selection Criteria
Facility must meet ALL measures to be designated as BDC+
Measure Name
Selection Criteria Description
Episode Volume
The facility has greater than or equal to 5 matched episodes of cost data in both clinical
categories:
• Vaginal Delivery
• Cesarean Delivery
Composite Cost Index
Composite Cost Index must be less than or equal to the established threshold of 1.00.

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 17
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Cost of Care Selection Criteria
Facility must meet ALL measures to be designated as BDC+
Measure Name
Selection Criteria Description
Local Blue Plan Cost
Criteria
(If Applicable)
An individual Blue Plan, at its own independent discretion, may establish and apply local cost
requirements as additional Selection Criteria for eligibility in a Blue Distinction Centers program,
for facilities located within its Service Area.
Quality is key: Only those facilities that first meet nationally established quality and business measures for Blue
Distinction Centers will be considered for designation as a Blue Distinction Center+.
Cost of Care Evaluation
Cost of care measures were designed to address market and consumer demand for cost savings and affordable
healthcare. The Cost of Care Selection Criteria were used to provide a consistent and objective approach to identify
BDC+ facilities. The inputs and methodology used in the cost of care evaluation are explained below.
Cost of Care Methodology Framework
The cost of care evaluation uses a consistent framework to define and adjust episodes, and to establish and
compare the resulting cost measures.
Figure 1. Cost of Care Methodology Framework Illustration
Defining the Episodes
Cost of care evaluation was based on a nationally consistent analysis of Claims Data. To provide validity for
comparisons, cost analytics for the BDC Maternity Care program focus on vaginal and cesarean deliveries.

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 18
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Cost Data Sources
Each facility’s cost of care is calculated using adjusted allowed amounts for specific maternity care episodes of care
for actively enrolled Blue Members, derived from Blue Plans’ PPO Claims data from National Data Warehouse from
January 1, 2019, through August 31, 2022, paid through November 30, 2022, with episodes of care occurring between
June 1, 2020, through May 31, 2022.
Clinical Category Identification Criteria
To provide validity for comparisons, cost analytics for the BDC Maternity Care program fo cus on vaginal and
cesarean births. This section explains how Maternity Care episodes are characterized and identifies the subset of
episodes included in the comparison analysis.
Maternity episodes are triggered by inpatient deliveries – either vaginal or cesarean, using the Blue Claims data.
and by MS-DRGs (DRGs are assigned by Blue Health Intelligence
®
(BHI) to ensure consistency of approach) and
are listed in Table 8.
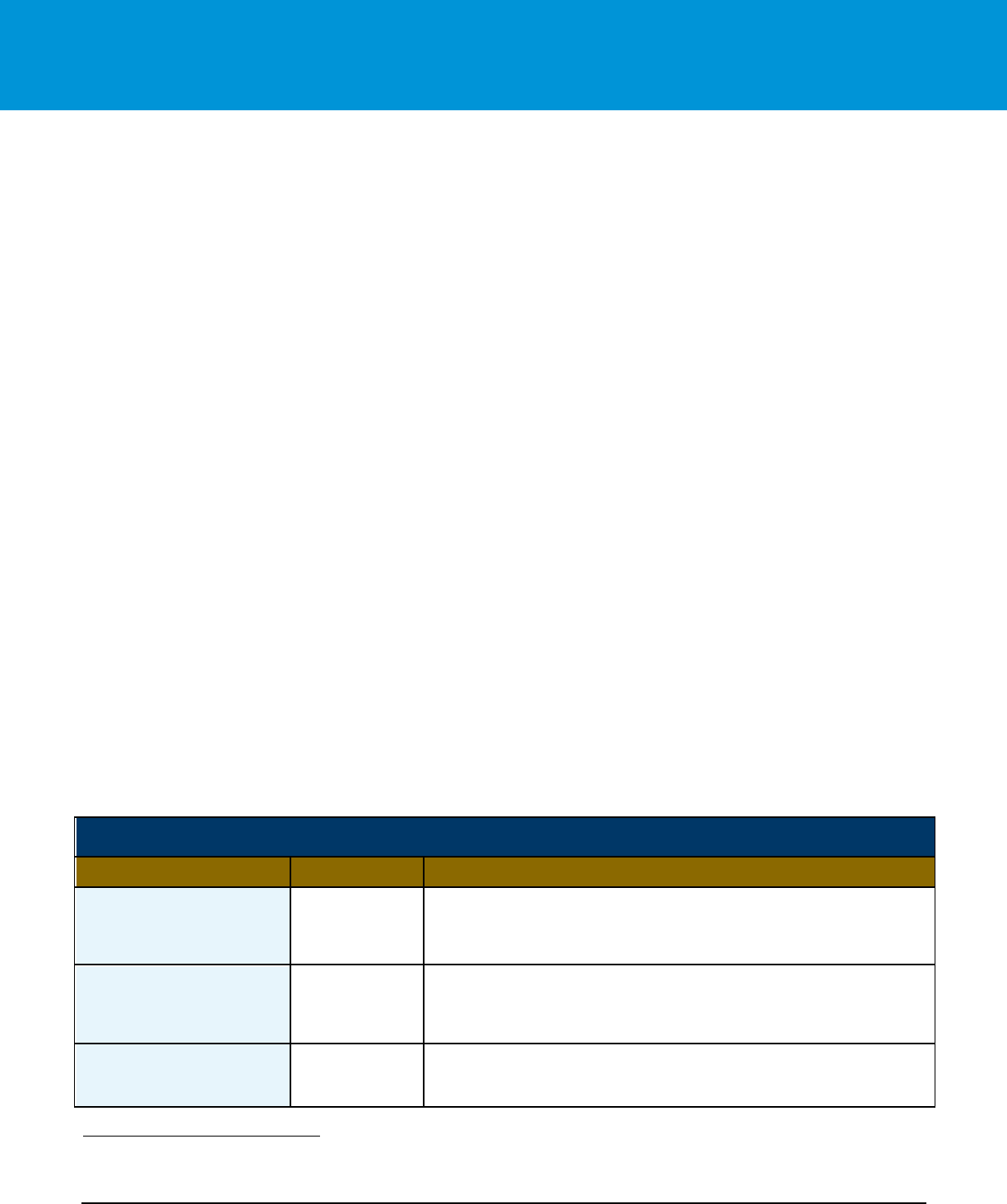
Table 8. Maternity Care MS-DRG Trigger Codes
Trigger Category
Code Type
Code
Code Description
Vaginal Deliveries
MS-DRG
805
Vaginal Delivery without Sterilization and/or D&C with MCC
MS-DRG
806
Vaginal Delivery without Sterilization and/or D&C with CC
MS-DRG
807
Vaginal Delivery without Sterilization and/or D&C
Cesarean Deliveries
MS-DRG
786
Cesarean Section without Sterilization with MCC
MS-DRG
787
Cesarean Section without Sterilization with CC
MS-DRG
788
Cesarean Section without Sterilization
CC – Complications or Comorbidities
MCC – Major Complications or Comorbidities
Costs associated with long-acting contraceptive (LAC) and sterilization procedures (IUD, Implant, and Tubal Ligation)
were flagged and excluded, using episode inclusion/exclusion criteria. This evaluation cycle used updated DRGs,
which provided more specificity and meaningfully reduced the number of episodes flagged for exclusion. The majority
of LAC and sterilization procedures were already removed from the beginning of the analysis because they were tied
to sterilization-specific delivery DRGs (i.e., 796, 797, 798, 783, 784, 785), which were excluded from the final trigger
code list.
Member Exclusion Criteria
• Exclude age <18 or >64 years.
• Exclude discharge status Left Against Medical Advice (LAMA) or discontinued care.
• Exclude expired or expired in a medical facility
• Exclude when primary payer is not a Blue Plan

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 19
Blue Distinction Centers for Maternity Care| Program Selection Criteria
• Exclude members not continuously enrolled for the duration of the episode
• Exclude multiple birth (e.g., twins)
• Exclude gender equal to male or unknown
• Exclude if episode did not include both professional and facility claim.
• Exclude if episodes included claims for long-acting contraceptive (LAC) and/or sterilization procedures.
Clinical category costs are adjusted for the impact of significant patient co-morbidities, via risk adjustment methods.
No other clinical exclusions are applied.
Episode Duration
Each delivery episode type has time windows before and after the episode trigger event (in-patient hospitalization
for delivery) within which relevant services may be included. The trigger start date is the First Service Date from the
facility header claim identified as the trigger claim. The episode window for maternity begins 280 days prior to date
of admission of the index admission and ends 90 days following discharge from the index admission. Episodes are
included in the analysis only if the member is continuously eligible for relevant (primarily PPO) BCBS benefits
throughout the episode duration
Cost Components Included in Episode
After an episode was “triggered,” services must be linked to the episode in a comprehensive and consistent manner
to ensure completeness and comparability of costs. Services and related costs were included if they were logically
related to the episode – either vaginal delivery or cesarean delivery.
Table 9 below provides more detailed examples of professional services billed using the following routine obstetric
services codes during the episode duration:
Table 9: Professional Services Billed for Routine Obstetric Service Codes
CPT
OB Maternity Service
59425
Antepartum care only; 4-6 visits
59426
Antepartum care only; 7 or more visits
59400
Routine OB care including antepartum, vaginal delivery, postpartum
59409
Vaginal delivery only
59410
Vaginal delivery only including postpartum care
59412
External cephalic version, with or without tocolysis; antepartum manipulation
59414
Delivery of placenta (separate procedure)
59510
Routine OB care including antepartum, cesarean, and postpartum
59514
Cesarean delivery only
59515
Cesarean delivery only; including postpartum care
59610
Routine obstetric care including antepartum, vaginal delivery and postpartum care, after previous
cesarean
59612
Vaginal delivery only, after previous cesarean delivery (with or without episiotomy and/or forceps)
59614
Vaginal delivery only, after previous cesarean delivery; including postpartum care
59618
Routine obstetric care including antepartum care, cesarean delivery, and postpartum care, following
attempted vaginal delivery after previous cesarean delivery

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 20
Blue Distinction Centers for Maternity Care| Program Selection Criteria
CPT
OB Maternity Service
59620
Cesarean delivery only, following attempted vaginal delivery after previous cesarean delivery;
59622
Cesarean delivery only, following attempted vaginal delivery after previous cesarean; including
postpartum
59430
Postpartum care only (separate procedure)
Adjusting Episode Costs
Adjustments in episode costs are needed for both the validity and fairness of cost comparisons among facilities and
included the following two types of adjustment:
• Factor adjustment – which adjusts for factors known to have a predictable impact on costs of care.
• Outlier management – which protects against rare, unpredictable high-cost and very low events that could
have a dramatic impact on average costs for a facility.
Two types of factor adjustments are made commonly in health cost comparisons:
• Adjustments for predictable cost differences related to geography; and
• Adjustments for predictable cost differences due to risk; or, more specifically, due to differences in the
clinical characteristics of patients and age that have a measurable and predictable impact on costs.
A geographic adjustment factor was applied to the episode cost, to account for geographic cost variations in
delivering care. Adjustments made for predictable cost differences related to geography used the 2023 Geographic
Adjustment Factors (GAFs) for 112 Geographic Practice Cost Index (GPCI) localities level, as defined by CMS.
Risk adjustment was used to adjust for variation in cost that may relate to differences in patient severity (with or
without comorbidity), as well as case mix, using the following steps:
• Identified patient severity levels, using the MS-DRG risk stratification system.
• Three separate age-bands (18-34 years, 35-39 years, and 40+ years) were created for better risk
assessment within each broad clinical category. As a result, there will be a total of nine sub-categories
to calculate nine risk adjustment factors under both vaginal and cesarean deliveries.
• Managed outliers through winsorization within risk bands. Outliers were identified in each risk band as
those values for which geographically adjusted costs were the top 2 percent and bottom 2 percent of
episode costs. Outlying cost values were truncated to these points, to preserve their considerations in
calculating the overall episode cost estimate while moderating their influence.
Calculated Risk Adjustment Factor
The mean of the geographically adjusted, winsorized episode costs for each clinical category/risk level combination
at the national level is the expected cost for that clinical category/risk level combination. The national expected cost
for each clinical category/risk level combination is divided by the national mean cost for the clinical category, to
calculate the Risk Ratio for each clinical category/risk level combination. The Risk Adjustment Factor (which is the
inverse of the Risk Ratio) is multiplied by each facility’s geographically adjusted and winsorized facility episode

Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 21
Blue Distinction Centers for Maternity Care| Program Selection Criteria
costs for each clinical category/risk level combination to normalize for risk, resulting in a final episode cost that is
both geographically adjusted, and risk adjusted.
Minimum Case Volume Requirement
For reliability, a minimum of 5 episodes are needed in each clinical category to be included in the cost calculation of
at the facility level. For maternity, this means that a facility must have 5 vaginal delivery episodes and 5 cesarean
delivery episodes to meet minimum case volume.
Establishing the Cost Measure
Each episode was attributed to the facility where the primary procedure/surgery occurred, based on trigger events
that occurred at that facility for each of the two clinical categories: vaginal delivery and cesarean delivery. Each
facility has a separate calculation for the Clinical Category Facility Cost (CCFC) based on the median value of the
adjusted episode costs. Confidence intervals (90 percent) were calculated around each Clinical Category Facility
Cost (CCFC) measure; the Upper Confidence Limit (UCL) of the measure was divided by the National Median
Episode Cost to become the Clinical Category Facility Cost Index (CCFCI). The combined cost index of the median
UCL was rounded down to the nearest 0.025 to give facilities the benefit of the doubt and to avoid situations where
a facility narrowly missed BDC+ eligibility by an immaterial margin. The rounded median UCL was the measure
used for cost scoring. For reliability, a minimum of five procedures was required within a clinical category for the
data to be included in the calculation of a Composite Facility Cost Index (CompFCI) for a facility.
Using each of the Clinical Category Facility Cost Index values, an overall Composite Facility Cost Index (CompFCI)
was calculated for the facility. Each Clinical Category Cost Index was weighted by that facility’s own volume and
facility costs to calculate a composite measure of cost called the Composite Facility Cost Index.
Composite Facility Cost Indices (CompFCI) for each facility, calculated using the UCL of individual clinical category
facility cost indices (CCFI), were then compared to the cost threshold set by BCBSA. A facility was selected for
BDC+ designation if the CompFCI was lower than or equal to the cost threshold set by BCBSA, demonstrating that
the expected composite facility cost index was lower than or equal to the cost threshold cost index.
Questions
Contact your local Blue Plan with any questions.
Blue Distinction Centers (BDC) met overall quality measures for patient safety and outcomes, developed with input from the medical community.
A Local Blue Plan may require additional criteria for facilities located in its own service area; for details, contact your Local Blue Plan. Blue
Distinction Centers+ (BDC+) also met cost measures that address consumers’ need for affordable healthcare. Each facility’s cost of care is
evaluated using data from its Local Blue Plan. Facilities in CA, ID, NY, PA, and WA may lie in two Local Blue Plans’ areas, resulting in two
evaluations for cost of care; and their own Local Blue Plans decide whether one or both cost of care evaluation(s) must meet BDC+ national
criteria. National criteria for BDC and BDC+ are displayed on www.bcbs.com. Individual outcomes may vary. For details on a facility’s in-network
status or your own policy’s coverage, contact your Local Blue Plan and ask your facility before making an appointment. Neither Blue Cross and
Blue Shield Association nor any Blue Plans are responsible for non-covered charges or other losses or damages resulting from Blue Distinction
or other provider finder information or care received from Blue Distinction or other providers.
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 22
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Appendix A: Obstetric Hemorrhage Patient Safety Bundle Elements
Appendix B: Severe Hypertension Patient Safety Bundle Elements
Severe Hypertension Patient Safety Bundle Elements
1. Facility has rapid access to standardized medications used for severe hypertension/eclampsia.
2. Facility ensures accurate measurement and assessment of blood pressure for every pregnant and
postpartum patient, including: (1) notification of OB Provider if systolic BP ≥ 160 or diastolic BP ≥110 for two
measurements within 15 minutes; and (2) after the second elevated measurement, initiates treatment with
antihypertensive medication(s) that are recommended to be administered ASAP (preferably within 60
minutes of verification).
3. Performs multidisciplinary reviews for monitoring of outcomes and process metrics, which include (at least)
required reviews by the perinatal quality improvement (QI) committee for appropriate and timely treatment of
severe range blood pressure and/or Severe Maternal Morbidity (SMM) Indicator (as defined by Centers for
Disease Control and Prevention).
4. Provides trauma informed support program for patients, their identified support network, and staff for all
serious complications of severe hypertension.
5. Provides educational information, which includes (at least) warning signs/ symptoms of severe hypertension/
preeclampsia, and who to contact with medical/ mental health concerns about the patient
6. Initiates postpartum follow-up visits to occur within 3 days of discharge for individuals whose pregnancy was
complicated by hypertensive disorders.
Obstetric Hemorrhage Patient Safety Bundle Elements
1. Uses an evidence-based risk assessment tool for hemorrhage risk at defined stages of labor (prenatal, on
admission, pre-birth, and on transition to postpartum care) for all patients.
2. Measures cumulative quantitative blood loss on all patients.
3. Performs active management of the 3rd stage of labor (department-wide protocol).
4. Completes multidisciplinary reviews for monitoring of outcomes and process metrics (at least) for obstetric
hemorrhage (OBH) cases resulting in 4 or more units of blood products and/or Severe Maternal Morbidity
(SMM) Indicator (as defined by Centers for Disease Control and Prevention) in perinatal quality
improvement (QI) committee.
5. Provides trauma informed support program for patients, their identified support network, and staff for all
significant hemorrhages.
6. Provides educational information, which includes (at least) warning signs/symptoms of obstetric hemorrhage
and who to contact with medical/mental health concerns about the patient.
Blue Cross Blue Shield Association is an association of independent Blue Cross and Blue Shield companies.
BDCMC01_072523 23
Blue Distinction Centers for Maternity Care| Program Selection Criteria
Appendix C: Safe Reduction of Primary Cesarean Births Patient Safety
Bundle Elements
Safe Reduction of Primary Cesarean Births Patient Safety Bundle Elements
1. Implements standardized admission criteria, triage management, education, and support for women presenting
in spontaneous labor.
2. Offers standardized techniques of pain management, comfort measures, and labor support methods that
promote labor progress and prevent dysfunctional labor.
3. Uses standardized methods in the assessment of the fetal heart rate status, including interpretation and
documentation based on National Institute of Child Health and Human Development (NICHD) terminology, and
encourages methods that promote freedom of movement.
4. Upholds standardized induction scheduling, to ensure proper selection and preparation of women undergoing
induction of labor.
5. Utilizes standardized evidence-based labor algorithms, policies, and techniques, which allow for prompt
recognition and treatment of labor dystocia.
6. Adopts policies that outline standardized management of Category II Fetal Heart Rate patterns and uterine
tachysystole.
7. Monitors primary cesarean delivery rates (using both a sample of cases [as determined by the facility] and
individual physician cases) for compliance with standardized evidence-based algorithms for labor dystocia and
management of Category II Fetal Heart Rate patterns to discuss in perinatal quality improvement (QI)
committee.
8. Provides trauma informed support for patients, their identified support network, and staff if necessary for
patients impacted by primary cesarean deliveries.
