
457
Approach to the Emergency Patient
Chapter 32
APPROACH TO THE EMERGENCY
PATIENT
TRESS GOODWIN, MD*; KATHERINE ELLIS, MD
†
; CRAIG GOOLSBY, MD, ME
‡
INTRODUCTION
WHY EMERGENCY MEDICINE IS DIFFERENT
EMERGENCY DEPARTMENT CONCEPTS AND PROCEDURES
Prehospital Arrivals
The Initial Assessment
Sick Versus “Not Sick”
The Safety Net
The Emergency Department Workup
PATIENT ISSUES AND CHALLENGES SPECIFIC TO THE EMERGENCY
DEPARTMENT
CHALLENGES IN DEPLOYED EMERGENCY MEDICINE
SPECIFIC CHIEF COMPLAINTS AND RED FLAGS
Abdominal Pain
Chest Pain
Headache
Trauma
Shock
Poisoning
Cardiac Arrest
Case-Based Approach Summary
DISPOSITION
SUMMARY
*
†
‡
-
458
Fundamentals of Military Medicine
INTRODUCTION
Military medical providers (MMPs) face numerous
challenges in both stateside and deployed medical
practice. One of the most daunting and time-sensitive
challenges is managing a patient with an acute life-
threatening illness or injury. Patients with anaphylaxis,
severe hemorrhage, unstable cardiac dysrhythmias,
or intractable seizures need the .
Many practitioners do not encounter these types of
patients in their normal practice, and therefore lack
a conceptual framework and organized approach to
handle an unexpected emergency. Regardless of their
medical background, a practitioner can apply funda-
of high-pressure situations. For students and providers
of all levels, this chapter will provide the approach of
a specialty-trained emergency physician (EP) to the
fundamentals of assessing and treating severely ill
and injured patients.
1
This chapter will introduce readers to the concepts
of simultaneous diagnosis and treatment, working
with imperfect or limited information, and operating
in resource-constrained environments. This approach
is critically important to the MMP who confronts the
challenges of a deployed environment with limited
access to specialty consultants, including EPs. The
chapter also touches on a variety of core emergency
patient presentations. While it is not intended to be
managing these patients.
Beyond the normal challenges of civilian emergency
medical practice, in which patients are primarily treated
in designated emergency departments (EDs), military
with scarce resources. Mental preparation for emer-
WHY EMERGENCY MEDICINE IS DIFFERENT
. When a
patient presents to an outpatient orthopedics de-
partment, for example, the patient’s issue is often
focused and within a limited subset of diagnoses,
such as fractures or joint pain. The same applies to
problems are often diagnoses rather than .
For example, a patient visits their primary care doctor
for diabetes management, and the goals of the visit
and expected outcomes are anticipated and often
predictable. Emergency patients typically present
with symptoms or a chief complaint. These symptoms
could represent a benign or life-threatening condi-
this distinction. Thus, practitioners must shift their
mindset to “complaint-based” or “symptom-driven”
evaluations of patients. Not all evaluations will lead
patient with “chest pain” or “abdominal pain” after
having excluded life-threatening conditions during
their workup process.
2
. There have been
numerous poorly informed popular media reports
about patients using EDs for non-urgent issues and
EDs primarily serving the uninsured. However, mul-
tiple studies have shown that nonacute issues do not
constitute the majority of ED visits, and that many
ED users are indeed insured and have a primary
care provider.
3–6
When a patient presents to the ED,
they are concerned enough about their symptoms
to seek emergency care, and their complaints are
often high risk. Emergency patients often believe
their symptoms are life threatening or warrant im-
mediate evaluation. An emergency practitioner must
recognize and acknowledge this worry. Sometimes
patients only need reassurance and education, and
then they can be safely discharged to their home or
returned to duty. It is important to remember that
even patients with benign conditions require respect
and a thorough evaluation of their complaint by an
experienced provider.
. EPs
face the need to form an immediate rapport with
patients, with whom they have no prior patient-
doctor relationships, in a high-stress environment.
The EP must rapidly earn the patient’s trust so he
or she will feel comfortable disclosing personal
details. In a deployed setting, EPs also care for
unique populations, such as local nationals and
enemy prisoners of war, which makes establishing
rapid rapport and an effective treatment relation-
ship even more complex.
. Test
results are often not available in time to make crucial
treatment information. Patients can arrive obtunded
and unable to provide a history. EPs often cannot fol-
low up with patients after discharge. These are just a
few examples of uncertainty emergency providers will
face. These situations can be uncomfortable, but mental
preparation for these realities can help non-emergency
specialists succeed.
459
Approach to the Emergency Patient
EMERGENCY DEPARTMENT CONCEPTS AND PROCEDURES
Prehospital Arrivals
Few non-EPs interact routinely with prehospital
providers. Prehospital crews transport most emer-
gently ill or injured patients, whether deployed or
stateside, for emergency care. In the United States,
patient transport is done by a combination of
paramedics and emergency medical technicians in
transport is done by military medics with varying
skill sets and in a multitude of platforms, such as heli-
copters, armored vehicles, or vehicles of opportunity.
Depending on the training and equipment of these
providers, the arriving patient may already have
had interventions and diagnostics performed, such
as venous access, an electrocardiogram, or a blood
glucose measurement. Most often, the prehospital
providers will call and report to the EP, allowing
the ED to prepare for the patient’s arrival. For ex-
ample, if an urgent surgical patient is inbound, the
EP can prepare and gather all necessary equipment,
have blood prepared to transfuse, and summon any
needed help or consultants prior to the patient’s ar-
rival. Preparation is even more important in mass
casualty events when a large number of patients
arrive at the same time.
The Initial Assessment
MMPs caring for emergency patients should hone
their ability to perform a “doorway assessment” for
a quick evaluation of the patient’s condition. Simple
observations by a well-trained eye are crucial to gath-
ering information and starting rapid treatment. Here
are questions to consider when evaluating a patient
on arrival:
• Did the patient arrive via ambulance or come
into the waiting room?
• Did the patient walk into the room or arrive
via wheelchair or stretcher?
• Does the patient walk without assistance?
With a steady gait?
• What is the patient doing? Writhing in pain?
Lying motionless? Talking on a cell phone?
• What is the patient’s work of breathing? Are
they gasping for air, wheezing, or breathing
comfortably?
• What is the patient’s level of pain? Are they
holding a particular area, grimacing, or moan-
ing?
• Is the patient actively vomiting?
• What is the patient’s mental status? Do they
acknowledge you walking in the room and
make appropriate eye contact, or is their
mental status altered?
• Is the patient morbidly obese, normal, or ca-
chectic?
• What about the skin: does the patient appear
pale, mottled, cyanotic, jaundiced, burned, or
covered in a rash? Do you see hemodialysis
access in their arm?
• What is the patient’s hygiene? Clean? Dishev-
eled? Neglected?
• What does the room smell like? Alcohol?
Gangrene?
• Is family, battle buddy, or a caretaker at the
bedside, or did the patient arrive alone?
All the above questions, and many more, can be
answered in seconds. Practitioners should be mindful
of all available information when seeing emergently ill
or injured patients. This review, combined with vital
signs, and very brief historical information can yield
important information needed to begin an emergency
assessment and stabilization.
Sick Versus “Not Sick”
EPs use the term “sick” to refer to seriously ill or
injured patients. While the vast majority of ED patients
have some degree of illness or injury, most will not
be critically ill. Determining “sick” from “not sick”
sounds simple, but is in reality a challenging skill that
must be developed by anyone providing emergency
care. Some patients’ situations are fairly obvious—in
clear respiratory distress, unconscious, or with hem-
orrhaging wounds. These conditions should be im-
mediately stabilized. The more challenging patients
are the ones who are not overtly sick, but have char-
acteristics that make them high risk and more likely
to decompensate.
A blunt trauma patient (eg, someone who had a
signs of trauma, a fairly benign exam, and stable
vitals. However, they may decompensate as internal
injuries, such as a lacerated spleen, worsen. Know-
ing that this patient has a high-risk history should
prompt the emergency practitioner to continue to
monitor and reevaluate the patient (see below for
“sick” patients).
460
Fundamentals of Military Medicine
The Safety Net
EPs use the term “safety net” in one of two ways. A
civilian ED is the safety net of the medical community.
An ED is the only medical facility open 24 hours a
day, 7 days a week, 365 days a year. When a patient’s
not have a primary care doctor or are visiting from
out of town, the emergency room may be the only
option. The ED may be the only option for the unin-
sured, under-insured, homeless, and mentally ill. In a
policy statement, the American College of Emergency
Physicians wrote:
Having the only universal mandate for providing
health care—the Emergency Medical Treatment
and Labor Act (EMTALA)—the nation’s more than
4,000 hospital emergency departments are a portal
for as many of three out of four uninsured patients
admitted to US hospitals, making them a vital,
although often unrecognized, component of the
safety net.
3
The safety net concept also refers to an initial
series of steps designed to stabilize patients. Once
must rapidly establish the safety net. While most
emergency patients will not rapidly decompensate
during their initial ED course, sick patients might. A
mantra often cited by medics and EPs alike is, “IV,
O
2
, monitor, advanced airway equipment.” These
procedures—establishing intravenous (IV) access,
placing the patient on oxygen and a cardiac monitor,
and ensuring advanced airway equipment is readily
available at the bedside—are the foundation of the
safety net.
The safety net should be started immediately.
On entering the room of a sick patient, emergency
providers should order the team to initiate safety
net procedures while rapidly anticipating next steps.
Should antibiotics be started? Does the patient require
intubation or additional venous or intraosseous access?
The key to establishing the safety net is preparedness,
and becoming comfortable starting treatment while
performing diagnostic studies. An elderly, hypoten-
sive, tachycardic patient with altered mental status is
sick. If the provider waits for all imaging and lab tests
to return, the patient may not survive. Additionally,
antibiotics, or cardioversion prior to performance of
any labs or additional diagnostic testing. These rapid
steps may be uncomfortable for many MMPs but may
save an emergency patient’s life.
The Emergency Department Workup
The focus of an emergency patient’s workup and
care is based on the chief complaint. Patients may
have many ongoing medical issues at a given time
and present with multiple complaints. However,
one acute issue typically prompts the ED visit, and it
should be the focus of the provider’s history, physi-
cal exam, and diagnostic testing. As in other areas of
medicine, patient history and physical examination
provide most of the needed information to drive any
necessary testing to diagnose and indicate appropri-
ate disposition the patient.
Unlike in some other areas of medicine, emergency
providers need to think in a mentality.
Medical students are typically trained to take a history
diagnosis, and then consider which diagnosis is most
likely. Emergency providers follow these steps as well;
however, instead of considering which diagnosis is
most likely, they must consider which is most lethal—
for emergency care often have emergency problems
and are at higher risk than those seen in outpatient
clinics. This does not mean that all patients require
exhaustive testing to exclude emergency diagnoses;
rather, it is imperative that an emergency provider
these diagnoses and exclude them by history,
physical examination, or testing if indicated.
For example, when a 30-year-old asthmatic patient
presents to an ED with a chief complaint of “shortness
of breath,” the diagnosis is most likely an asthma ex-
acerbation. However, a pulmonary embolus is a more
lethal diagnosis. If the provider does not consider
and at least mentally address this possibility, he or
she might miss an important emergency condition.
Knowing the potentially fatal diagnoses for each
patient complaint and focusing a workup to exclude
them are key knowledge and skills for emergency
providers.
Again, testing should be focused on the patient’s
chief complaint. MMPs should consider available re-
sources and choose tests that will management
of their patient. An example of a widely available test
that can rapidly change management is a pregnancy
test in a woman of childbearing age with an abdominal
or pelvic complaint. This one simple qualitative answer
can drastically change the direction of diagnostics and
treatment. On the other hand, an example of an often
unnecessary test is a rib x-ray series. For a patient with
mild chest trauma who is suspected of having either
a rib fracture or rib contusion, rib x-rays are usually
not indicated. Rib fractures and contusions are treated
461
Approach to the Emergency Patient
in the treatment. A chest x-ray may be indicated to
exclude pneumothorax or another abnormality, but
emergency management or patient disposition or
follow-up. Management is the same—pain manage-
ment and prevention of atelectasis or pneumonia with
incentive spirometry.
PATIENT ISSUES AND CHALLENGES SPECIFIC TO THE EMERGENCY DEPARTMENT
Most EDs have individual patients who frequently
use the ED for care. Sometimes derogatorily called
and often for similar presentations. They are usually
older, have chronic medical conditions such as coro-
nary artery disease or asthma, and can be a source of
use the ED as their only source of care, but studies have
shown that they are also likely to utilize outpatient
clinics and have high rates of hospital admission.
4–6
As with other patients, the challenge is to know when
their issues are acute and life threatening. They must
be evaluated during each encounter with the same
thoughtful approach as any other patient. Additional
resources, such as social worker consultations, should
also be considered to help address other factors of their
frequent ED utilization.
EPs play a crucial role in detecting signs of abuse
in patients—ranging from infant/child abuse, to
intimate partner violence, to elder abuse and ne-
glect.
7
Patients presenting with multiple visits and
various injuries, along with stories inconsistent with
addition, concern should be raised if the patient
seems evasive or inappropriately frightened, or if
an overbearing and perhaps defensive partner or
family member is in the room.
8
In children, bruises
in various stages of healing as well as fractures or
injuries not consistent with their age or mobility
9
Often the ED may
having reasonable suspicion with at-risk patients
with concerning injuries could be the intervention
that saves their life.
CHALLENGES IN DEPLOYED EMERGENCY MEDICINE
Deployed MMPs face additional challenges in the
personal safety can be a concern. During deployment,
MMPs are far from loved ones and may have limited
ability to communicate with them. Additionally, prac-
titioners may be working outside their normal comfort
zone in their patient care duties. Several challenges for
emergency providers follow.
. MMPs will almost
certainly care for more than American troops when
deployed. They may treat contractors, local nationals,
third-country nationals, enemy prisoners of war, and
a host of other individuals. Caring for these popula-
tions may involve certain rules and unique challenges,
but the basic principle remains that MMPs provide
a baseline standard of care to every patient, regard-
less of background. Department of Defense Directive
2310.01E, which covers the Defense detainee program,
mandates “humane treatment,” which includes “ap-
detainee’s condition, to the extent practicable.”
10
As in
caring for diverse patients stateside, this may require
a language interpreter and adaptation to cultural
concerns. It is important that each MMP is aware of
resources available to help care for these patients, and
. Military emergency providers
in scope than those typically seen during stateside
duty. This book covers mass casualty in a separate
chapter (Chapter 34, Mass Casualty Preparedness and
Response), but it is important for emergency providers
to develop or understand their facility’s contingency
plan during a mass casualty event.
. The resources
available will vary dramatically depending upon the
practice environment. Section II of this book, Op-
erational Health Service Support, covers this topic in
more detail. The military designates various levels of
care based on availability of resources, ranging from
-
patients or perform advanced diagnostics. Those at a
Role 3 facility, such as an Air Force theater hospital,
will likely have computed tomography (CT) scanners,
a host of medications, and access to operative care
with surgical subspecialists. While MMPs should still
consider tests that would change patient management,
practicing at home.
462
Fundamentals of Military Medicine
SPECIFIC CHIEF COMPLAINTS AND RED FLAGS
This section consists of case scenarios focusing on
several common patient complaints. It is not meant to
be a complete list of chief complaints seen in the ED;
rather, it is designed to help MMPs learn the process
of evaluating a patient from an emergency medicine
perspective. The scenarios and workups described
include some repetition, partly because emergency
medicine providers approach many patients in a
similar way. As discussed previously, the EP will ask,
“is the patient sick or not sick?” and then proceed to
a more thorough history and exam as appropriate.
-
thing the patient reports in the history, a physical
study. Some may seem obvious, such as a patient who
is unconscious, but others are subtler. The scenarios
that follow also take into account some of the unique
challenges of military medicine: austere locations,
limited resources, long transport times, and a diverse
patient population.
Abdominal Pain
-
°
Abdominal pain can be a complex and frustrating
chief complaint for the EP. A recent study showed
that 6.5% of ED patients have abdominal pain as
their presenting complaint, and of these, 21% were
-
nal pain.”
11
A focused history and physical exam can
those patients who need further testing.
Even before the EP sees the patient, her vital signs
indicate she has tachycardia and borderline hypoten-
sion, and is potentially sick. The patient should be
asked more history about her abdominal pain: When
or worse? Are there associated symptoms such as nau-
sea, vomiting, changes in bowel movements, changes
in urination, anorexia, or vaginal bleeding? Does she
have a history of chronic abdominal problems such
bowel disease? Has she had prior abdominal surger-
ies? When was her last menstrual period?
All women and girls of childbearing age, even in the
A pregnancy test is the most important test to order
for this patient because the results will direct further
imaging studies and disposition. A pelvic exam can
be considered if there is concern for pelvic pathology.
Abnormal vital signs must be addressed. If the patient
If she is in pain, she may need either PO or IV pain
medication. Most abdominal pain patients should
initially be kept NPO (nil per os, or nothing by mouth)
until a surgical emergency is excluded.
-
This patient must be worked up for ectopic preg-
nancy, a potentially life-threatening condition in which
the fetus implants outside of the uterus, usually in the
ovarian tube. The patient should be kept NPO. Appro-
priate labs to consider include complete blood count
to evaluate for anemia given her history of vaginal
bleeding, basic metabolic panel, quantitative human
chorionic gonadotropin (HCG), and blood type and
IV pain medications. A pelvic ultrasound should be
performed, which can be used not only to identify an
ectopic pregnancy, but also to evaluate other serious
causes of abdominal pain such as an ovarian torsion or
tuboovarian abscess (Exhibit 32-1). A skilled EP may
be able to perform this test at the bedside. Depending
on the facility’s resources, ultrasound technicians and
radiologists may be available to perform and interpret
the study.

463
Approach to the Emergency Patient
EXHIBIT 32-1
ABDOMINAL PAIN:
CAN’T-MISS DIAGNOSES
• perforated ulcer
• cholecystitis
• pancreatitis
• ischemic bowel
• diverticulitis
• appendicitis
• pyelonephritis
• ectopic pregnancy
• ovarian torsion
• testicular torsion
• tuboovarian abscess
• pelvic inflammatory disease
• myocardial infarction
• bowel obstruction
• volvulus
• gastrointestinal bleed
• abdominal aortic aneurysm
This exam is concerning for a ruptured ectopic preg-
nancy: a surgical emergency. The patient may be losing
bedside FAST (focused abdominal sonographic study
the abdomen (Figure 32-1). A FAST exam is a rapid,
bedside test that can be used to evaluate for the pres-
Figure 32-1. Ultrasound showing ruptured ectopic preg-
nancy.
the capability, the patient should go to the operating
room with a gynecologist for surgical repair. If those
resources are not available, she should be immediately
transferred to the nearest facility with surgical capabil-
ity, which may include transfer to a general surgeon
if a gynecologist is unavailable.
The presence of abnormal vital signs, and especially
worsening vital signs throughout a patient’s visit,
should warn the EP there might be a life-threatening
problem. Rebound and guarding on physical exam
are concerning for a ruptured viscus. In this case, the
-
ent clinical scenario, rebound tenderness may be a sign
of appendicitis, cholecystitis, diverticulitis, perforated
peptic ulcer, ruptured abdominal aortic aneurysm,
or other serious conditions. These patients all need
prompt surgical consultation.
problems, acidosis, and severe anemia may also
prompt admission or transfer. Stable abdominal pain
patients with normal vital signs and reassuring physi-
and with non-concerning labs and imaging studies (as
indicated), may possibly be safely discharged to quar-
ters or full duty. Discharged patients with abdominal
pain should have a repeat abdominal exam in 24 to 48
-
tions to return sooner for worsening or concerning
symptoms. These return precautions may include
worsening pain, persistent vomiting, high fevers, or
other new concerns. If the patient is unable to follow
up with their primary care physician, it is reasonable
to have them return to the ED.
Chest Pain
°
Chest pain accounts for 3% of ED visits and can
range from common active duty problems such as
muscle strains, costochondritis, and viral syndromes
to truly life-threatening etiologies.
12
Six life-threatening
causes of chest pain a provider should consider in
every chest pain patient are acute coronary syndrome,
464
Fundamentals of Military Medicine
pulmonary embolus, aortic dissection, hemothorax,
pneumothorax, esophageal rupture, and pneumonia
(Exhibit 32-2). Before any chest pain patient can leave
the ED, these diagnoses should be ruled out, either by
history and physical exam or with diagnostic testing.
The patient should be asked to describe his chest
pain: when did it start? What does it feel like? What
-
toms such as shortness of breath, nausea, diaphoresis,
or cough? He should be questioned about his risk
factors for acute coronary syndrome, such as smok-
ing, family history, hypertension, hyperlipidemia,
and diabetes. He should also be questioned about
risk factors for a pulmonary embolus: smoking, pro-
longed immobility, leg swelling, family history, and
known hypercoaguable disorder. In any chest pain
patient, it is important to conduct a thorough review
of systems and inquire about recent fevers, coughing,
or other illness, as well as recent cardiac or esophageal
procedures.
Physical exam should focus on cardiopulmonary
and abdominal exams, as well as assessing the extremi-
ties for peripheral edema and distal pulses, and the
neck for jugular venous distension. All chest pain pa-
tients should quickly have an electrocardiogram (ECG)
performed and interpreted by an EP. The American
College of Emergency Physicians and the American
College of Cardiology recommend that an ECG be
performed within 10 minutes of arrival for all patients
with chest pain.
12
Most EDs have quality standards
that require an ECG to be performed and interpreted
by an EP within 10 to 15 minutes of a patient’s arrival.
EXHIBIT 32-2
CHEST PAIN:
CAN’T-MISS DIAGNOSES
• acute coronary syndrome
o unstable angina
o ST elevation myocardial infarction
o non-ST elevation myocardial infarction
• aortic dissection
• pulmonary embolism
• pneumothorax
• hemothorax
• pneumonia
• esophageal rupture
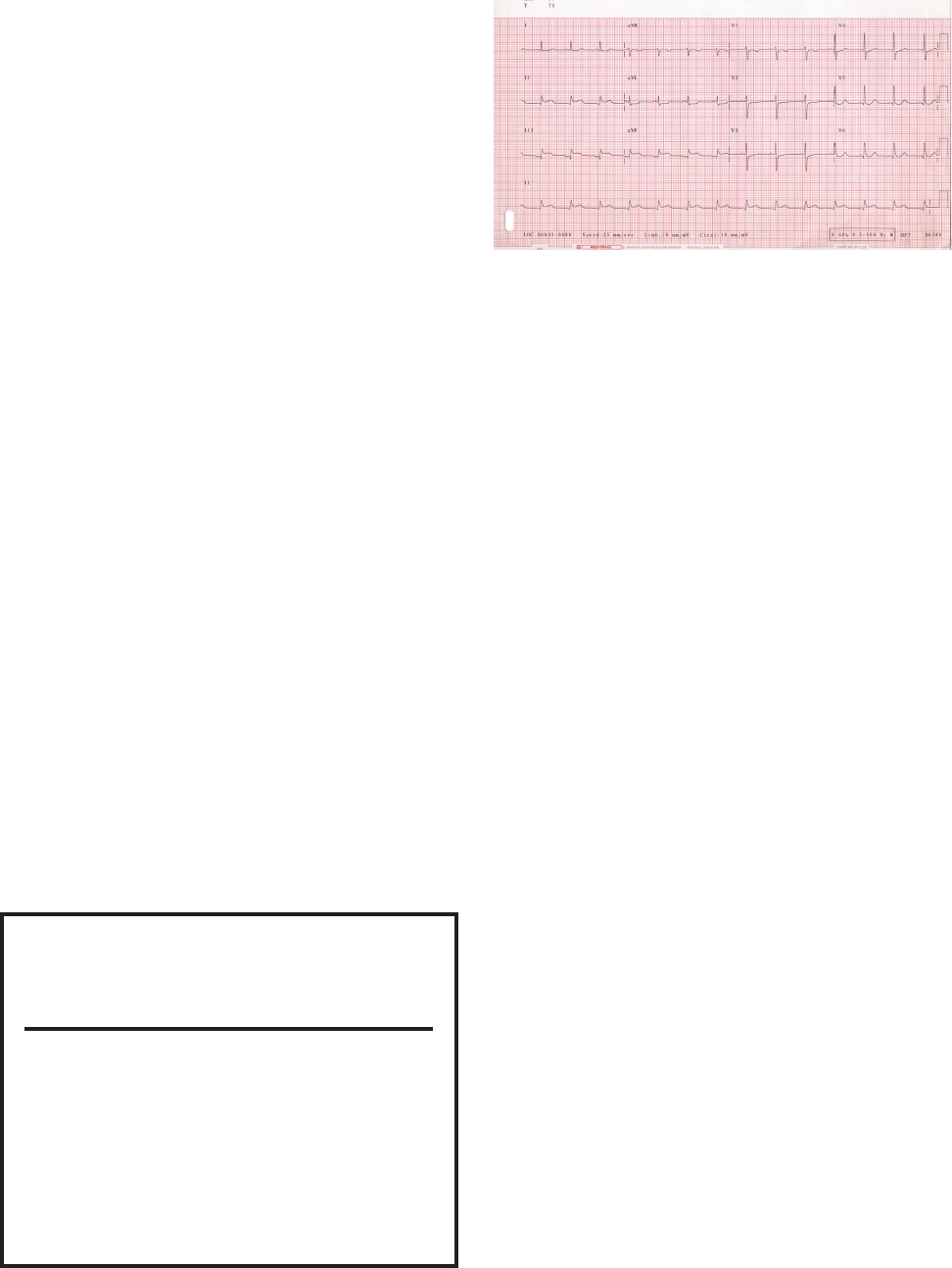
The ECG shows an ST-elevation myocardial
infarction (STEMI)—a true cardiac emergency. ST
elevation on ECG indicates that damage (infarction)
is occurring throughout all layers of the heart muscle.
A thrombus (clot) has occluded blood supply to part
of the heart, and heart muscle tissue is dying.
13
Once
this is diagnosed, the EP must immediately initiate
treatment, potentially before a full history or physical
exam can be obtained. The patient should be placed
on oxygen and should receive aspirin. He should
receive nitroglycerin for ongoing pain. However,
nitroglycerin can drop a patient’s blood pressure and
should be used judiciously once IV access has been
becomes hypotensive).
In many stateside military and civilian facilities,
STEMI patients are taken immediately to the cardiac
catheterization lab to undergo an invasive procedure
this resource is usually not available. Instead, patients
can be given thrombolytics, which are IV medications
that help break up the clot. These medications all
carry risks of bleeding complications, and the patient
After receiving thrombolytics, the patient will likely
require transport to a higher level of care for cardiol-
ogy consultation and intensive care management. In
this case, the STEMI seen on ECG makes the patient’s
disposition easy for the EP. But what if his ECG had
There are many other life-threatening causes of
chest pain that can present with a normal or nonspe-
Figure 32-2. Twelve-lead electrocardiogram with ST seg-
ment elevation in leads II, III, and aVF for an inferior acute
myocardial infarction. April 12, 2005.
Reproduced from: https://en.wikipedia.org/wiki/

465
Approach to the Emergency Patient
work and imaging performed. A chest x-ray can be
-
mothorax or pneumonia. If there is a high suspicion for
an aortic dissection or pulmonary embolus, a CT of the
chest with IV contrast should be obtained, because they
are not readily diagnosed with a standard chest x-ray.
Elevated cardiac enzymes may clinch the diagnosis of
MI in a patient with a borderline ECG.
Many patients who present to the ED with chest
who are older and have risk factors for acute coronary
threatening causes of chest pain without a period of
observation. Patients with potential cardiac risk factors
and no etiology of their chest pain found in the ED
require observation, repeat exams, repeat ECGs, and
serial cardiac enzyme screens in addition to some form
of stress test. According to the resources at a facility,
this process may be done in the ED, a chest pain obser-
vation unit, or an inpatient ward, or via a coordinated
outpatient approach. All patients who are discharged
with a diagnosis of chest pain should have close follow-
up with their primary care physician or appropriate
specialist and should be given clear return precautions.
Headache
Three-quarters of Americans experience a head-
ache each year, and headaches account for 2 million
ED visits.
14
Most of these patients have a primary
headache disorder such as migraines, cluster head-
aches, or tension-type headaches, and can be treated
symptomatically and discharged. However, a subset
have a “secondary” headache: a pathologic process
such as a tumor or vascular event in which head pain
is the presenting symptom. To help distinguish be-
tween a regular migraine headache and a headache
with a potentially more serious cause (Exhibit 32-3),
the patient should be asked additional questions.
How did the pain start? What does it feel like? Does
located? What time of day is it worse? What medica-
tions are you taking? Are there associated symptoms
such as fever, nausea, vomiting, photophobia, or
EXHIBIT 32-3
HEADACHE:
CAN’T-MISS DIAGNOSES
• intracranial hemorrhage
• meningitis
• intracranial mass
• cerebrovascular accident
• acute angle closure glaucoma
• hypertensive encephalopathy
is concerning for meningitis, a life-threatening infec-
Many medications such as nitroglycerin, calcium
of headache, and many recreational drugs can cause
headaches as well. If the patient has recently decreased
headache. Multiple members of a family with new
headaches, especially in the winter months, should
raise suspicion for carbon monoxide poisoning.
14
New headaches that worsen over a period of weeks,
especially headaches that are worse in the morning,
are concerning for elevated intracranial pressure from
a mass lesion or neoplasm.
-
Pain that is abrupt and maximal at onset is concerning
for a subarachnoid hemorrhage.
14
The patient will need
IV access, a careful neurological exam, and immediate
non-contrast head CT. Except for glaucoma patients,
virtually all patients presenting with headache should
receive analgesia and should be kept in a quiet, dark
area.
All patients with headaches also require a thorough
neurological exam. Tenderness over the sinuses or
purulent drainage from the nose could indicate sinus-
itis. In elderly patients, the temporal arteries should
be palpated to evaluate for temporal arteritis. Acute
angle closure glaucoma can present with headache in
addition to visual changes, conjunctival injection, and
pupillary changes. If this diagnosis is suspected, pa-
tients should have their intraocular pressures checked.
for further imaging. Patients with altered mental status
or new onset seizures also require further imaging.

466
Fundamentals of Military Medicine
. What are your
The patient’s CT scan shows a subarachnoid hemor-
rhage—a neurosurgical emergency. In the ED, the ini-
tial management involves resuscitation, reversal of any
coagulopathies, and stabilization. The patient should
carefully monitored. She will need frequent neurologi-
cal exams, and if her neurological status deteriorates
further, she will require intubation for airway protec-
tion. She will require neurosurgical consultation and
to be monitored for additional bleeding, vasospasm,
-
tory drugs, aspirin, and other blood-thinners should
be avoided when treating her pain.
In managing headaches, special care should be giv-
en to certain populations. The elderly are unlikely to
develop new onset migraines, and are at much higher
risk for chronic subdural hematomas that can present
with only mild headaches. Physicians should have a
low threshold to order a CT scan on elderly patients
with new onset headaches.
14
In pregnant patients,
untreated, this condition can progress to eclampsia,
cerebral hemorrhage, or both. Most headache patients
with stable vital signs, a normal neurological exam,
Figure 32-3. Computed tomography head scan showing
subarachnoid hemorrhage.
-
diagnosis.
Trauma
-
According to the Joint Theater Trauma Registry
(JTTR), most combat-related injuries in Operation
Enduring Freedom and Operation Iraqi Freedom
occurred as a result of injury from explosions (78%),
usually IEDs. Due to improvements in body armor,
there was a low rate of thoracic injuries. The highest
rate of injury was to the extremities (54%), followed
by the abdomen, face, and head. JTTR statistics show
that hemorrhage is the leading cause of potentially
preventable combat-related death. Tactical Combat
Casualty Care (TCCC) principles and practice have
greatly reduced mortality from hemorrhage, along
with damage control resuscitation and surgery, rapid
patient evacuation, and sophisticated patient transport
mechanisms.
15
Initial stabilization of trauma patients in the de-
lifesaver or combat medic. Most medics and physicians
(discussed in Chapter 33, Tactical Medicine), and the
EP will likely also have been trained in Advanced
Trauma Life Support. Both of these courses provide a
standard, algorithmic approach to managing trauma
that focuses on immediate stabilization of the patient’s
life-threatening injuries. The pneumonic “XABCDE”
can be used to remember the sequence of care in a
then move on to airway, breathing, and circulation,
followed by disability and exposure. When a threat
to survival is found, it must be rapidly addressed and
-

467
Approach to the Emergency Patient
This collection of vital signs and physical exam
respiratory emergency and form of obstructive shock.
to hypoxia and hypotension from decreased venous
return and pressure on the heart. The patient should
undergo immediate needle decompression with a
14-gauge needle followed by chest tube insertion.
Circulation can be assessed quickly by palpating
pulses. A palpable radial pulse indicates a systolic BP
of at least 80, and a palpable femoral or carotid pulse
indicates a BP of at least 60. Tachycardia and hypo-
tension can be signs of shock, but it is important to
in a healthy, active duty population. Certain trauma
patients, such as the elderly, those in neurogenic shock,
and those taking beta-blocker medications, may not
be able to mount a tachycardic response. In any case,
hemorrhagic shock should be treated aggressively
The patient should have a quick evaluation of his
mental status (D for disability). This can be performed
using the pneumonic “AVPU”: alert/awake, verbal,
painful, or unresponsive (Exhibit 32-4). Is the patient
fully awake? Does he only respond to voice? Does he
only respond to painful stimuli, or is he completely
unresponsive? Also, he should be exposed from head
to toe to evaluate for any additional injuries.
At this point in evaluation, additional studies are
often performed as adjuncts to the primary survey.
A positive FAST exam in an unstable patient is an
indication for operative intervention. Trauma x-rays
(usually with portable chest x-ray and portable pelvis
EXHIBIT 32-4
“AVPU” SCALE FOR CONSCIOUSNESS
ASSESSMENT
• Alert. The patient is alert and awake.
• Verbal. The patient responds to verbal stimuli.
• Pain. The patient responds to painful stimuli.
• Unresponsive. The patient is unresponsive.
x-ray devices) are also performed at this point. A CT
injuries (Exhibit 32-5).
Once the XABCDEs have been performed and im-
mediate life threats addressed, the patient should be
asked additional history and should undergo a head-
to-toe secondary survey. A pneumonic to guide the
additional history is “AMPLE”: allergies, medications,
past illnesses, last meal, and events involved in the
trauma. The secondary survey consists of a systematic
assessment of the patient, inspecting and palpating all
body parts for injuries while also performing a more
thorough neurological exam. As these steps are per-
formed, a nurse or tech should send a panel of blood
work to the lab. Depending on the nature and severity
of the trauma, these may include a type and cross for
blood, complete blood count, basic metabolic panel,
lactate, coagulation panel, urinalysis, alcohol level,
and drug screen. After these steps are completed, ad-
ditional imaging can be ordered based on the results of
the secondary survey and suspected injuries. This may
include extremity x-rays, a retrograde urethrogram
or cystogram, and CT scans of the head, spine, chest,
abdomen, and pelvis.
16
-
EXHIBIT 32-5
TRAUMA:
CAN’T-MISS DIAGNOSES
• shock
• airway compromise
• tension pneumothorax
• massive hemothorax
• open pneumothorax
• flail chest
• cardiac tamponade
• brain herniation
• aortic disruption
• spinal injuries
• pelvic ring disruption
• hemoperitoneum

468
Fundamentals of Military Medicine
Figure 32-4. Chest x-ray showing right-sided pneumothorax.
Figure 32-5. Computed tomography head scan showing
subdural hematoma.
The patient’s subdural hematoma will require ur-
gent neurosurgical evaluation and possible surgery
if his neurological status deteriorates. This is a case
in which the deployed environment provides unique
challenges. The patient presented to the ED at a multi-
national hospital, where a neurosurgeon is likely avail-
able. If he had presented further forward, he would
have required evacuation, possibly by a critical care air
transport (CCATT) or tactical critical care evacuation
(TCCET) team, to get him to neurosurgical care in an
-
agement of his chest tube, neurosurgical evaluation
of his subdural hematoma, and orthopedics, trauma,
and/or vascular evaluation of his amputation. Once
these conditions have stabilized to the point where he
of theater by a CCATT team.
Shock
-
-
Shock refers to a state of hypoperfusion in which
oxygen delivery to the tissues is inadequate to meet the
metabolic demands of the body. Broadly speaking, it is
and supply that results in cellular death.
17
If shock is
not rapidly treated, it leads to end-organ failure and
death. There are four broad categories of shock: hy-
povolemic, cardiogenic, distributive, and obstructive
(Table 32-1).
17
Hypovolemic shock is the most common, especially
circulatory volume, most commonly from hemorrhage
or dehydration. Treatment focuses on volume expan-
sion with blood, crystalloid, or both as indicated.
18
Cardiogenic shock is caused by cardiac dysfunction,
usually from an MI, and the heart pump is unable to
meet the demands of the body’s tissues. Treatment
support, and reperfusion therapy for MI. Obstructive
shock involves some blockage of blood leading into
or out of the heart, either from a physical blockage
such as a massive pulmonary embolus, or a pressure-
gradient blockage caused by a tension pneumothorax
or cardiac tamponade. The causes of obstructive shock
may all present as pulseless electrical activity (PEA)
and should all be considered when working through
the “H”s and “T”s during a code (see the Cardiac Ar-
rest section below). Lastly, distributive shock results in

469
Approach to the Emergency Patient
TABLE 32-1
CATEGORIES AND CAUSES OF SHOCK
Category Causes
Hypovolemic Trauma
Gastrointestinal bleeding
Severe dehydration (gastroenteritis,
burns)
Cardiogenic Acute myocardial infarction
Rate problems: bradycardia or tachycardia
Toxins
Cardiomyopathy
Distributive Sepsis
Anaphylaxis
Neurogenic
Toxins
Obstructive Pericardial tamponade
Pulmonary embolism
Tension pneumothorax
mediators and cytokines, which leads to a decrease
in systemic vascular resistance and a compensatory
increase in cardiac output. Sepsis is the most common
cause, but anaphylaxis, neurological injuries, and cer-
tain toxins can also cause this presentation.
17
Patients with shock require the EP’s immediate
-
taneously with the history and exam, and before
diagnosing the shock state’s etiology. The EP should
rapidly assess the patient’s general appearance and
vital signs. Patients in shock will often be hypoten-
sive, tachycardic, and tachypneic. If the patient has
respiratory distress or is unable to protect his airway
secondary to confusion, he may require intubation.
Supplemental oxygen should be considered for all
Patients in septic shock in particular may require
-
sure does not improve after 1 to 2 L of crystalloid,
or if the patient is unable to tolerate large volumes
heart failure), vasoactive medications, such as norepi-
nephrine or dopamine, may be required to increase
blood pressure and improve tissue perfusion. All
patients presumed to be in septic shock should have
labs ordered to look for the source of infection (blood
tests, etc) and be started on early, broad-spectrum
antibiotic therapy. As the patient is stabilized, the EP
can obtain a more detailed history and perform a full
physical exam.
In this case, a more thorough history and exam
points to a clear etiology for the patient’s symptoms:
distributive shock secondary to anaphylaxis from a
bee sting. The mainstay of treatment for anaphylaxis is
-
teract vasodilation and bronchospasm. Epinephrine is
typically given subcutaneously initially, but may also
be given via an IV route.
18
-
Patients with this type of shock may sometimes be
discharged from the ED. Patients with anaphylaxis
who are asymptomatic after one dose of epinephrine
can be observed for 4 to 6 hours and, if they remain
asymptomatic, safely discharged. Observation is
necessary because some patients may require a
repeat dose of epinephrine. Nearly all other patients
who present in shock will require admission, often
to the ICU, for continued fluid resuscitation and
patients in shock are stabilized and then transported
out of theater by CCATT, whose staff are able to
continue treatment with vasoactive medications, blood
level of care. Indicators that shock has resolved include
normalization of vital signs, improved urine output,
down-trending lactate, and normal volume status.
18
It is important to remember that certain special
most common causes of shock are dehydration second-
ary to infectious gastroenteritis and hemorrhagic shock
secondary to trauma.
17
Pediatric patients are able to
compensate for a large amount of volume loss with
minimal change in vital signs. Thus, they can appear

470
Fundamentals of Military Medicine
well even in the early stages in shock. When these
compensatory mechanisms fail, they will deteriorate
rapidly, and the EP must be ready to intervene. In
contrast, the elderly have limited reserves and are often
unable to tolerate the hemodynamic changes of shock.
The elderly are more susceptible to infectious diseases
and are also more likely to present with cardiogenic
shock. Underlying comorbidities such as cardiac or
renal disease may make them unable to tolerate ag-
them closely for the development of complications
such as pulmonary edema.
Poisoning
-
Poisonings, whether from an accidental or inten-
of toxicology is a subspecialty of emergency medicine.
It is estimated that at least 5 million poisonings occur in
the United States each year, although the actual num-
ber may be even higher due to underreporting.
19
The
poisoned ED patient can present in conditions rang-
ing from completely awake, alert, and asymptomatic
to completely obtunded with unstable vital signs. As
with any ED patient, assessment begins as soon as the
EP looks at the patient and continues with the ABCs.
Initial priorities are securing the patient’s airway
and treating potentially reversible causes of her altered
mental status. These treatments, often referred to as the
“coma cocktail,” include 100% oxygen to treat hypoxia,
(followed by the administration of dextrose if glucose
is low), and naloxone to reverse an opioid overdose. If
chronic alcoholism is suspected, thiamine can be given
before glucose. If the patient is obtunded, the airway
should be secured with intubation. Many toxins can
rate, salicylates can increase the respiratory rate and
cause pulmonary edema, and various inhalants may
cause bronchospasm. As the ABCs are addressed and
concerning conditions stabilized, the EP must also re-
member to place the patient on “suicide watch” with
20
If the patient is able to talk, or if there are others
who can provide the history, it is important to ask the
following questions: What was ingested? How much
was ingested? When did this occur? Why? (Was it an
accidental or intentional overdose?) A head-to-toe
physical exam should be performed on all patients,
-
tus, pupils, skin, and presence of track marks or other
evidence of drug use. Some poisonings cause common,
recognizable “toxidromes,” described in Exhibit 32-6.
20
-
-
Although additional history has helped identify the
patient’s likely ingestion, she should still undergo a
broad workup to look for complications of her inges-
tion and to identify any possible co-ingestions. Most
acutely poisoned patients are worked up with cardiac
EXHIBIT 32-6
POISONING “TOXIDROMES”
Anticholinergic
• mad as a hatter (altered mental status)
• blind as a bat (mydriasis)
• hot as Hades
• red as a beet
• dry as a bone
Cholinergic
• salivation
• lacrimation
• urination
• defecation
• gastrointestinal upset
• excessive bradycardia
Sympathomimetic
• tachycardia
• hypertension
• mydriasis
• diaphoresis
• hyperthermia
• agitation
Opioid
• miosis
• apnea
• hypoxia
• flash pulmonary edema (rare)
471
Approach to the Emergency Patient
monitoring; an ECG; complete blood count; compre-
hensive metabolic panel, acetaminophen, salicylate,
and ethanol levels; urinalysis; and urine or serum drug
screen. Females of childbearing age should be tested
for pregnancy. If the patient has metabolic acidosis,
a serum osmolality may help further narrow the dif-
ferential. Other than acetaminophen, salicylates, and
are usually sent to a lab, but results take several days.
The EP must treat presumptively based on the history,
In treating the poisoned patient, the EP must
consider methods of preventing absorption or aid-
ing elimination of the toxin. These include activated
charcoal, whole bowel irrigation, and gastric lavage.
Activated charcoal is given PO or via nasogastric tube
to absorb toxins still in the gastrointestinal tract. It is
but is occasionally given later for extended-release
toxins or potentially lethal ingestions.
21
It does not bind
metals, alcohols, or hydrocarbons and should be used
cautiously in patients with altered mental status, who
are at increased risk for aspiration.
Whole bowel irrigation is infrequently utilized and
involves giving the patient polyethylene glycol solu-
tion (eg, GoLytely [Braintree Laboratories; Braintree,
of a toxin. It is occasionally used for patients who have
ingested extended-release preparations and patients
with illicit drug packet ingestions (“body packers”).
Gastric lavage is seldom performed due to a high risk
patient presents immediately after a lethal ingestion,
pill fragments from the stomach.
19
Acetaminophen is one of the most common and
most dangerous ingestions seen in the ED. Because
an acute ingestion will often have minimal symp-
toms, and because the potential for long-term liver
damage is high, the EP should consider checking
acetaminophen levels for every poisoned patient. In
overdose, acetaminophen is metabolized to N-acetyl-
p-benzoquinone imine (NAPQI), which causes liver
nomogram. A level of 150 or greater at 4 hours is con-
sidered toxic. Patients with a toxic ingestion should
be started on the antidote, N-acetylcysteine. Starting
this antidote promptly after ingestion can prevent liver
damage and death.
N
often to the ICU, for close cardiopulmonary monitor-
ing. If a poisoned patient is asymptomatic after several
hours of observation in the ED, they may possibly be
safe for discharge after psychiatric evaluation. Con-
sultation with a poison control center, if available, is
present with an intentional ingestion as a suicide at-
tempt will likely need to be removed from theater and
transported back to the United States for psychiatric
treatment.
Cardiac Arrest
An estimated 250,000 Americans die each year from
unexpected cardiac arrest. Many of these cases occur
outside of a hospital, and most occur in men aged 50 to
75 who have underlying heart disease.
22
In a way, the
cardiac arrest patient is the quintessential emergency
medicine patient: obviously sick and in need of rapid
assessment and interventions that, if performed cor-
Managing a cardiac arrest and its aftermath can be an
intellectually stimulating yet emotionally draining
experience for the EP. In an arrest, the EP will end up
treating not only the patient, but also his or her family,
who will require extensive explanation and support,
whatever the outcome.
The initial goals in managing a cardiac arrest
include the principles of BLS: to “support or restore
return of spontaneous circulation or until ACLS [ad-
vanced cardiac life support] interventions can be initi-
ated.”
23
chest compressions. The old pneumonic “ABC” has
been altered to “CAB” for these patients to shift focus
-
ers should check for a carotid pulse for no more than
10 seconds. If no pulse is present, responders should

472
Fundamentals of Military Medicine
start cardiopulmonary resuscitation (CPR), pushing
hard and fast, 100 to 120 compressions per minute,
and allowing full chest recoil between compressions.
The patient should receive two rescue breaths with a
pocket mask or bag valve mask between compressions.
The airway should be opened with a head tilt, chin
patient should be shocked as recommended by the
23
As more advanced practitioners arrive on scene,
and once the patient arrives in the ED, more advanced
resuscitation techniques can be started. The ACLS pro-
also includes advanced airway techniques, such as in-
tubation, and IV medications such as epinephrine and
amiodarone. End-tidal capnography can be a useful
and the correct placement of the endotracheal tube.
Cardiac arrest from a primary cardiac disorder often
presents with this rhythm or with pulseless ventricular
tachycardia, which is treated in the same manner. In
patients return to their baseline neurological status.
23
and IV amiodarone. IV access should be obtained as
quickly as possible, and if IV access is not immedi-
ately available, an interosseous line should be placed
instead. Many ACLS medications can also be given
via the endotracheal tube, but given the widespread
availability of interosseous lines and their ease of in-
sertion, the endotracheal tube method is being used
be rapidly obtained because hypoglycemia can be a
rapidly reversible cause of altered mental status and
cardiac arrest.
associated mechanical pumping.
23
Successful resuscita-
tion of a patient in PEA should be focused on rapidly
identifying and treating the cause. The EP may think
of the “H”s and “T”s (Exhibit 32-7) to remember all the
potential causes of PEA. All patients in PEA should be
treated with oxygen and ideally intubated to correct for
-
cose screen can rapidly identify hypoglycemia. Blood
that is rapidly run through an i-STAT machine (Ab-
hypokalemia or hyperkalemia and acidosis. Patients
in PEA should be kept warm. A bedside ultrasound
can be performed to evaluate for cardiac tamponade
and to evaluate the right side of the heart for changes
consistent with a large pulmonary embolus. Based
on the clinical scenario, the patient may require an
emergent pericardiocentesis to treat a tamponade,
Figure 32-6. Rhythm strip showing ventricular fibrillation.
Reproduced from: https://commons.m.wikimedia.org/wiki/
ECGpedia).png.
Figure 32-7. Rhythm strip showing pulseless electrical
activity.
Reproduced from: https://en.m.wikipedia.org/wiki/
EXHIBIT 32-7
CARDIAC ARREST “H”S AND “T”s
• hypovolemia
• hypoxia
• hydrogen ion (acidosis)
• hyper/hypokalemia
• hypoglycemia
• hypothermia
• toxins
• tamponade (cardiac)
• tension pneumothorax
• thrombosis (acute coronary syndrome and pul-
monary embolism)

473
Approach to the Emergency Patient
needle decompression for tension pneumothorax, or
IV thrombolytics for suspected pulmonary embolus
or MI. The patient should continue to receive high-
quality CPR and IV epinephrine every 3 to 5 minutes.
If a reversible cause of PEA is not rapidly discovered
and corrected, the patient’s prognosis is extremely
poor. Only 1% to 4% of patients with PEA survive to
hospital discharge
24
(see Exhibit 32-7).
-
Asystole has a very poor prognosis because even
minutes without oxygen to the brain portends very
poor functional outcomes. For patients in asystole,
treatment should still be focused on restoring perfu-
sion with high-quality CPR and identifying a reversible
cause. After 20 minutes of combined BLS and ACLS,
resuscitation is unlikely to be successful. Bedside ultra-
sound can be a useful adjunct in evaluating for cardiac
activity. If the patient has been in asystole for 20 min-
utes and shows no cardiac activity on ultrasound, it
then ensure that the patient’s family is updated and
their questions are answered. If possible, the patient’s
primary care doctor should be contacted as well.
Only a small percentage of resuscitated cardiac
arrest patients survive to hospital discharge, and of
Figure 32-8. Rhythm strip showing asystole.
Reproduced from: https://commons.m.wikimedia.org/wiki/
injury. If the patient regains a pulse but does not
regain consciousness, the EP should initiate targeted
temperature management. Randomized control trials
versus targeted temperature management. Maintain-
ing a constant temperature between 32° and 36°C
for at least 24 hours postarrest is the current recom-
mendation, and this has been shown to improve both
survival rates to hospital discharge and neurological
outcomes.
24
The procedure is usually started in the ED
If acute coronary syndrome is suspected, the postarrest
patient should be strongly considered for emergent
cardiac catheterization.
Case-Based Approach Summary
The above cases are only a sample of the life-
threatening chief complaints an EP may encounter.
They are meant to emphasize the common processes
in the approach to the emergency medicine patient,
regardless of initial patient complaint. In these cases,
the EP must quickly determine whether the patient is
“sick or not sick.” Another key skill is the ability of the
EP to simultaneously obtain history and diagnoses,
while starting to treat the patient. Unlike the orderly,
thorough approach to the patient history taught in
medical schools, the EP must quickly obtain basic his-
tory while simultaneously relaying orders to nurses
and technicians and rapidly thinking through a list
of “can’t miss/worst case scenario” diagnoses. This is
often done with incomplete records and potentially
no help from the patient themselves if they are in
extremis. These cases also emphasize the challenges
in diagnosis and treatment based on the EP’s practice
environment: forward deployed location, theater hos-
pital, or stateside medical facility. Once initial patient
stabilization is complete, the EP can focus on the next
phase of patient care: disposition.
DISPOSITION
Potential dispositions from the ED include admis-
sion to the hospital for observation, additional workup,
facility with a higher level of care; discharge home or
to self-care; and of course, unfortunately, transfer to
the morgue. The EP must consider numerous factors to
determine the most appropriate place for disposition.
For example, considering a terminal patient whose
primary issue is managing pain and maintaining qual-
ity of life, sending them home may be the best course.
Their terminal disease will not be cured by a hospital
admission, and admission can in fact be detrimental
(the hospital can expose patients to numerous noso-
comial infections and be less comfortable). Discharge
home is appropriate as long as pain medications can
be administered at home.
The decision to admit or discharge a patient is
one of the unique challenges of emergency medicine.
The EP must make this decision in a timely manner,
often with an incomplete history of present illness,
minimal to no knowledge of the patient’s past medi-
cal history, and equivocal testing. Although this can
474
Fundamentals of Military Medicine
with a patient. Performing serial examinations and
discussing the case with a consultant can help the
EP decide.
When collaborating with consultants, it is essen-
tial that the EP remain an advocate for the patient.
Consultants generally prefer brief presentations
previous chest pain patient, a consulting cardiolo-
gist might expect to hear, “I have a 55-year-old man
with multiple cardiac risk factors who presents with
a STEMI on ECG. We have treated him with aspirin,
nitroglycerin, and heparin, and would like him to go
to the cath lab. Could you come evaluate him in the
ED? Are there any other treatments you would like us
to start?” Depending on the case and resources at the
facility, a consultant may evaluate the patient in the
ED and ultimately discharge him, admit the patient
primarily, or manage the patient alongside another
service (usually internal medicine). When possible, it
them in person rather than providing advice over
the phone. In many EDs, and especially in austere or
Specialist consultants may be in other parts of the
country or region, or stateside. In these cases, sending
pictures of ECGs and other images to the consultant
may be the next best course of action. Some hospitals
have telemedicine services, in which a consultant
(often a neurologist for a stroke patient), can evaluate
the patient via a video monitoring system.
When patients require admission, the EP must de-
or if they require a transfer. In the stateside military
-
fer to a higher level of care; many stateside military
hospitals do not provide neurosurgical capabilities.
The patient presenting with a subarachnoid hemor-
rhage might require transfer to a civilian facility for
an even larger challenge. The deployed patient pre-
senting with a ruptured ectopic pregnancy would
certainly require transfer to a higher level of care for
surgical treatment.
If transfer is required, the EP’s next question is
how to most safely transport the patient: by air or by
ground. This decision will rely on a multitude of fac-
tors including the stability of the patient, the resources
of the facility, weather conditions, and the location
of the accepting hospital. This decision will often be
made in consultation with the accepting provider at
the next level of care.
EP may need to write admission orders for the inpa-
tient unit. These should be done in consultation with
may require phone calls to multiple consultants to
coordinate care.
Many patients can be safely discharged from the
ED. However, the decision to discharge can produce
anxiety for the EP and for the patient, especially if the
patient is being discharged without a clear diagnosis.
As discussed throughout the chapter, the purpose of
an evaluation in an ED is to recognize and stabilize
life-threatening conditions. Often, a skilled EP is able
to determine that there is no life-threatening condi-
tion present and no reason for admission, but the
cause of the patient’s chest pain, abdominal pain, or
other symptom, is still unclear. In these circumstanc-
es, the EP must have a discussion with the patient
about what has been done in the ED, what the next
steps should be (primary care follow-up, outpatient
follow-up with a specialist, further testing as an out-
patient, trial of medication, etc), and any reasons to
return to the ED.
Patients should be told what they should do to
improve their condition, for example, ice, rest, eleva-
sprain. What the patient is NOT allowed to do should
seizure may be stable for discharge with outpatient
neurology follow-up, but should be counseled not
to drive or engage in other high-risk activities. In the
patients with mild traumatic brain injury/concussion
may be in a condition to be discharged, but should be
counseled to avoid all strenuous physical activity until
headache and other symptoms completely resolve and
they have been cleared by their primary care doctor
or neurologist.
Patients should be told when and where to follow
up. For high-risk patients such as infants, pregnant
women, and the elderly, and for high-risk complaints
such as abdominal pain and chest pain, it is preferable
patient to follow up, ideally in 24 to 48 hours, for a
repeat evaluation. If this is not possible and the EP is
truly concerned for the patient, the best option may be
to have the patient return to the ED in 24 to 48 hours
for a recheck. This procedure has often been used for
has not been ruled out.

475
Approach to the Emergency Patient
SUMMARY
The approach to the emergency medicine patient,
involve fundamentals of emergency care during
evaluation and treatment of acute conditions. Perform
rapid “doorway” assessments, determine whether
the patient is sick or not sick, establish a safety net,
diagnostics and treatment. Utilizing lessons in this
chapter can help non-emergency MMPs provide bet-
ter patient care.
REFERENCES
1. Schneider SM, Hamilton GC, Moyer P, Stapczynski JS. Definition of emergency medicine. . 1998;5:348–
351.
2. Mahadevan SV, Garmel GM. A. Cambridge, UK: Cambridge University
Press; 2005.
3. American College of Emergency Physicians. The uninsured: Access to medical care. ACEP website. https://www.acep.
org/News-Media-top-banner/The-Uninsured--Access-To-Medical-Care/. Published 2016. Accessed February 12, 2017.
4. Sun BC, Burstin HR, Brennan TA. Predictors and outcomes of frequent emergency department users.
2003;10:320–328.
5. Vinton DT, Capp R, Rooks SP, Abbott JT, Ginde AA. Frequent users of US emergency departments: Characteristics
and opportunities for intervention. . 2014;31(7):526–532. doi:10.1136/emermed-2013-202407.
6. Ku BS, Fields JM, Santana A, Wasserman D, Borman L, Scott KC . The urban homeless: super-users of the emergency
department. . 2014;17:366–371. doi:10.1089/pop.2013.0118.
7. Clarke ME, Pierson W. Management of elder abuse in the emergency department. .
1999;17:631–644,vi.
8. McCloskey LA, Lichter E, Ganz ML, et al. Intimate partner violence and patient screening across medical specialties.
2005;12:712–722.
9. Jain AM. Emergency department evaluation of child abuse. . 1999;17:575–593,v.
10. Work RO. . Washington, DC: DoD; August 19, 2014. DoD Directive 2310.01E.
11. Hastings RS, Powers RD. Abdominal pain in the ED: A 35 year retrospective. . 2011;29(7):711–716.
12. American Heart Association. Recommendations for criteria for STEMI systems of care. http://www.heart.org/
HEARTORG/Professional/MissionLifelineHomePage/EMS/Recommendations-for-Criteria-for-STEMI-Systems-of-
13. Antman E. ST-elevation myocardial infarction. In: Fuster V, ed. .
Oxford, UK: Wiley-Blackwell; 2009: 55.
14. Lynch KM, Brett F. Headaches that kill: a retrospective study of incidence, etiology and clinical features in cases of
sudden death. . 2012;32:972–798.
15. Beekley AC, Bohman H, Schindler D. Modern warfare. In: Savitsky E, Eastridge B, eds.
. Ft Detrick, MD: Borden Institute; 2012: chap 1. http://www.cs.amedd.army.mil/borden/
book/ccc/UCLAchp1.pdf. Accessed March 17, 2017.
16. Kman NE. Trauma. Clerkship Directors in Emergency Medicine (CDEM) curriculum. http://www.cdemcurriculum.
. Accessed March 17, 2017.
476
Fundamentals of Military Medicine
17. Oker E. Shock. In: Hamilton H, ed. 2nd ed. Philadelphia,
PA: WB Saunders; 2003: 60–74.
18. Avegno J. Shock. Clerkship Directors in Emergency Medicine (CDEM) curriculum. http://www.cdemcurriculum.org/
. Updated 2008. Accessed March 17, 2017.
19. Wilson R, Wolf L. The poisoned patient. In: Hamilton H, ed. -
ing. 2nd ed. Philadelphia, PA: WB Saunders; 2003: 259–285.
20. Thibodeau L. Poisoning. Clerkship Directors in Emergency Medicine (CDEM) curriculum. https://cdemcurriculum.
com/poisonings/. Updated 2008. Accessed October 10, 2017.
21. Charcoal, activated. Drugs.com. https://www.drugs.com/monograph/charcoal-activated.html. Accessed January 25,
2018.
22. Lawson L. Cardiac arrest. Clerkship Directors in Emergency Medicine (CDEM) curriculum. https://cdemcurriculum.
com/cardiac-arrest/. Updated 2008. Accessed October 10, 2017.
23. Leschke R. Cardiopulmonary and cerebral resuscitation. In: Mahadevan S, Garmel G, eds.
. New York, NY: Cambridge University Press; 2005: 47–62.
24. Neumar RW, Shuster M, Callaway CW, et al. Part 1: executive summary: 2015 American Heart Association guidelines
update for cardiopulmonary resuscitation and emergency cardiovascular care. 2015;132(18 suppl 2):315–367.
