
Sheep Diseases
The Farmers’ Guide
Original version developed by Emily Litzow for Department of Primary Industries and Regions,
Biosecurity SA Animal Health.
Updated in 2022 by Red Meat and Wool Growth Program with contributions from Dr Elise Spark,
Dr Jeremy Rogers, Dr Celia Dickason and Chris Van-Dissel for Department of Primary Industries
and Regions, Biosecurity SA Animal Health.
Funded by SA Sheep Industry Fund, Biosecurity SA and the Red Meat and Wool Growth Program.
Use of the information and advice in this guide is at your own risk. The Department of Primary
Industries and Regions and its employees do not warrant or make any representation regarding the
use, or results of the use, of the information contained herein as regards to its correctness, accuracy,
reliability, currency or otherwise. The entire risk of the implementation of the information and advice
which has been provided to you is assumed by you. All liability or responsibility to any person using
the information and advice is expressly disclaimed by the Department of Primary Industries and
Regions and its employees.

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
2
Contents
How to use this guide 4
Reporting serious or unusual animal disease signs 5
Funding for disease investigations 6
Key to disease diagnoses by signs and symptoms 7
Key to disease diagnoses by season 9
Key to poisoning or toxicity by plant 10
Exotic diseases 11
Exotic diseases 12
Learn how to recognise emergency animal diseases 13
Anthrax 14
Bluetongue 15
Foot and mouth disease (FMD) 16
Sheep diseases & conditions 17
Acidosis (grain overload) 18
Annual ryegrass toxicity (ARGT) 19
Arthritis 20
Botulism 21
Cheesy gland (CLA) 22
Cobalt deficiency 23
Coccidiosis 24
Copper deficiency 25
Copper poisoning 26
Dermatophilosis and dermatitis (‘dermo’, lumpy wool) 27
Exposure losses 28
Foot abscess 29
Footrot 30
Grass tetany (hypomagnesaemia) 31
Large lungworm 32
Listeriosis (circling disease) 33
Lupinosis 34
Mastitis 35
Milk fever (hypocalcaemia) 36
Nitrate poisoning 37
Ovine brucellosis (Brucella ovis) 38
Ovine Johne’s disease (OJD) 39
Oxalate poisoning 40
Perennial ryegrass staggers 41
Phalaris poisoning 42

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
3
Phalaris staggers 43
Photosensitisation 44
Pinkeye 45
Pneumonia 46
Polioencephalomalacia (PEM, star gazing disease) 47
Pregnancy toxaemia (twin lamb disease) 48
Pulpy kidney (enterotoxaemia) 49
Pyrrolizidine alkaloid poisoning 50
Scabby mouth 51
Selenium deficiency (white muscle disease) 52
Tapeworm cysts (bladder worm, sheep measles, hydatids) 53
Tetanus (lockjaw) 54
Vibriosis (Campylobacteriosis) 55
Other conditions 56
Sheep lice 57
Sheep worms 58
Flystrike 59
Management guides 60
Good biosecurity 61
One Biosecurity 62
Vaccination 63
Grain introduction 64
NLIS obligations 65
Fit to load 66
Humane destruction 67
Acknowledgments & further reading 68
Useful contacts and online resources back cover

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
4
How to use this guide
This guide has been designed as a quick-reference tool to
help farmers take action when faced with a broad range of
sheep diseases on the farm. It will help you assess signs
and symptoms and identify possible causes and provides
information on diagnosis, treatment options, prevention
and general sheep health management.
Printed and digital resources are referenced throughout to
assist you with further, more detailed reading on a number
of sheep diseases, conditions and best practice guidelines.
You will also find a list of useful contacts and websites on
the back of this guide.
Photo credit: Animal Health Australia

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
5
Always keep an eye out for serious or unusual signs and
symptoms in livestock including:
• unexplained deaths
• sores or ulcers on feet or inside mouth (this may result
in a reluctance to eat or move)
• excessive salivation (drooling should always be treated
suspiciously)
• reduction in milk yield from cows and eggs from chickens
• diarrhoea, especially if it has blood in it
• excessive nasal discharge (unless you know what has
caused it)
• staggering, head drooping or severe lameness, especially
if more than one animal at the same time.
Serious animal diseases must be reported. Early reporting
provides the best chance to contain and manage an outbreak
before it spreads. If you notice any serious or unusual signs
or symptoms with your animals, you can:
• call the 24-hour Emergency Animal Disease Hotline
on 1800 675 888
• contact your local Department of Primary Industries and
Regions (PIRSA) Animal Health office (see back cover for
phone numbers)
• contact your local veterinarian.
Reporting serious or unusual
animal disease signs

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
6
Funding for disease investigations
Subsidies are available to support private veterinary
investigations into animal diseases where an infectious
agent is a potential cause. This is to help producers
maintain and demonstrate South Australia’s highly
regarded animal health status.
The program covers all livestock species, companion
animals, and wildlife (including feral animals) and is aimed
primarily at early detection and diagnosis of emergency
animal diseases.
For further information, contact your local veterinarian,
who may access these funds through PIRSA.
Scan QR code to learn more
about disease surveillance
or visit www.pir.sa.gov.au/
livestock-disease-surveillance

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
7
Abscess
• Cheesy gland
• Foot abscess
Abortion/stillbirth
• Ovine brucellosis
• Listeriosis
• Vibriosis
Anaemia
• Oxalate poisoning
• Worms
Blindness
• Pinkeye
• Polioencephalomalacia
Convulsions
• Annual ryegrass toxicity
• Grass tetany
• Phalaris poisoning
• Phalaris staggers
• Polioencephalomalacia
• Pulpy kidney
• Perennial ryegrass
staggers
• Tetanus
Coughing
• Lungworm
• Pneumonia
Downer sheep
• Annual ryegrass toxicity
• Botulism
• Exposure losses
• Grass tetany
• Lungworm
• Milk fever
• Oxalate poisoning
• Phalaris poisoning
• Phalaris staggers
• Polioencephalomalacia
• Pregnancy toxaemia
• Pyrrolizidine alkaloid
poisoning
Infected wound
• Malignant oedema
Infertility
• Ovine brucellosis
Ill thrift
• Cobalt deficiency
• Coccidiosis
• Copper deficiency
• Copper poisoning
• Lungworm
• Lupinosis
• Nitrate poisoning
• Ovine Johne’s disease
• Oxalate poisoning
• Polioencephalomalacia
• Pyrrolizidine alkaloid
poisoning
• Selenium deficiency
• Worms
Jaundice
• Copper poisoning
• Lupinosis
• Pyrrolizidine alkaloid
poisoning
Key to disease diagnoses by signs and symptoms

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
8
Lameness
• Acidosis
• Arthritis
• Foot abscess
• Footrot
Leg paddling
• Annual ryegrass toxicity
• Grass tetany
• Listeriosis
• Oxalate poisoning
• Phalaris poisoning
• Polioencephalomalacia
Nervous/neurological
signs
• Annual ryegrass toxicity
• Botulism
• Copper deficiency
• Grass tetany
• Listeriosis
• Lupinosis
• Milk fever
• Oxalate poisoning
• Perennial ryegrass
staggers
• Phalaris poisoning
• Phalaris staggers
• Pulpy kidney
• Tetanus
Salivation/frothing
at mouth
• Botulism
• Grass tetany
• Listeriosis
• Phalaris poisoning
Scabs
• Cobalt deficiency
• Dermatophilosis
• Lupinosis
• Pyrrolizidine alkaloid
poisoning
• Scabby mouth
Scours
• Acidosis
• Coccidiosis
• Copper poisoning
• Nitrate poisoning
• Pyrrolizidine alkaloid
poisoning
• Worms
Sudden death
• Acidosis
• Annual ryegrass toxicity
• Copper poisoning
• Exposure
• Flystrike
• Grass tetany
• Listeriosis
• Milk fever
• Oxalate poisoning
• Phalaris poisoning
• Polioencephalomalacia
• Pregnancy toxaemia
• Pulpy kidney
• Ryegrass staggers
• Tetanus
• Worms
Wool abnormalities
• Copper deficiency
• Dermatophilosis

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
9
Key to disease diagnoses by season
Spring
Sept/Oct/Nov
• Annual ryegrass toxicity
• Cobalt deficiency
• Foot abscess
• Lupinosis
• Oxalate poisoning
• Pyrrolizidine alkaloid
poisoning
• Selenium deficiency
Summer
Dec/Jan/Feb
• Annual ryegrass toxicity
• Cobalt deficiency
• Lupinosis
• Pneumonia
• Pyrrolizidine alkaloid
• Poisoning
• Perennial ryegrass
staggers
• Selenium deficiency
Autumn
March/April/May
• Lungworm
• Lupinosis
• Phalaris poisoning
• Phalaris staggers
• Pneumonia
• Pyrrolizidine alkaloid
poisoning
• Perennial ryegrass
staggers
Winter
June/July/August
• Exposure losses
after shearing
• Foot abscess
• Lungworm
• Nitrate poisoning
• Oxalate poisoning
• Phalaris poisoning
• Phalaris staggers
• Pneumonia

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
10
Key to poisoning or toxicity by plant
Annual ryegrass toxicity
• Annual ryegrass
(Lolium rigidum)
Lupinosis
• Lupin stubble
(Lupinus species)
• Lupin hay
(Lupinus species)
• Lupin grain
(Lupinus species)
Nitrate poisoning
• Capeweed
(Arctotheca calendula)
• Oats (Avena sativa)
• Canola (Brassica napus)
• Wild turnip (Brassica rapa)
Oxalate poisoning
• Soursob
(Oxalis pes-caprae)
• Sorrel (Acetosella vulgaris)
Phalaris poisoning
• Phalaris
(Phalaris aquatica)
Phalaris staggers
• Phalaris
(Phalaris aquatica)
Photosensitisation
• Salvation Jane/
Paterson’s curse
(Echium plantagineum)
• Heliotrope/potato weed
(Heliotropium europaeum)
• Caltrop (Tribulus terrestris)
• St John’s Wort
(Hypericum perforatum)
• Buckwheat (Polygonum
fagopyrum)
• Hairy panic (Panicum
effusum)
• Sweet grass (Panicum
laevifolium)
• Lantana (Lantana camara)
• Fungus of facial eczema
(Pithomyces chartarum)
• Fungus of lupinosis
(Phomopsis
leptostromiformis)
• Blue-green algae
(Anacystis cyanea)
Pyrrolizidine alkaloid
poisoning
• Salvation Jane/
Paterson’s curse
(Echium plantagineum)
• Heliotrope/potato weed
(Heliotropium europaeum)
• Caltrop (Tribulus terrestris)
Perennial ryegrass
staggers
• Perennial ryegrass
(Lolium perenne)

Exotic diseases

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
12
Exotic diseases
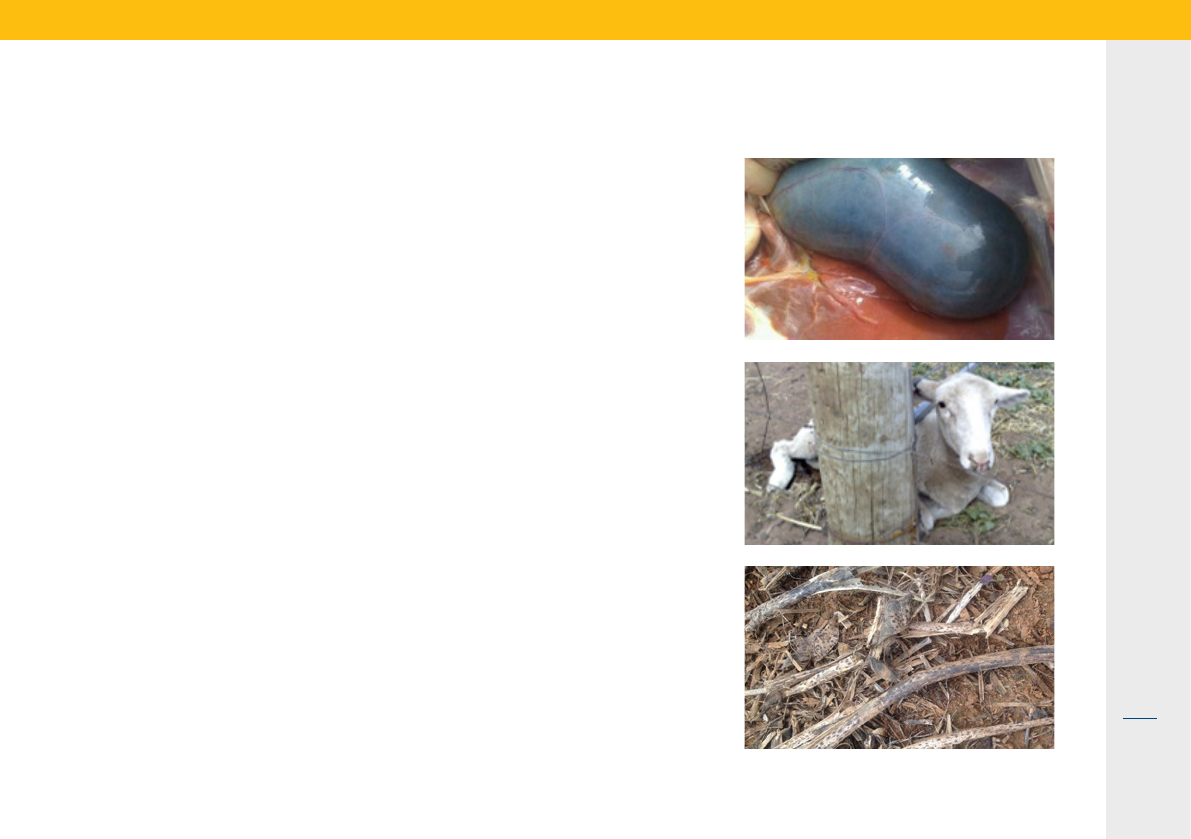
This sheep has barbers pole (Haemonchus).
These sheep have lice.
This sheep has bluetongue, an exotic disease.
This sheep has scrapie, an exotic disease.
Exotic diseases don’t always look spectacular. They often look the same as common diseases seen every
day on South Australian farms.
Help protect the future of our livestock industry by seeking veterinary assistance as soon as you notice a
problem and report your concerns to the Emergency Animal Disease Hotline on 1800 675 888.
Source: National Animal Disease Information Service (NADIS)

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
13
Use the new app to learn how to identify signs of emergency
animal disease (EAD) in sheep.
Download to your mobile phone by searching ‘Sheep EAD AR’
in the app store.
The tool generates a flock of augmented reality sheep providing
an opportunity for the user to identify the sick animal by looking
for signs and symptoms.
The diseases included in the tool are:
• foot and mouth disease
• bluetongue
• scrapie
• sheep pox
Learn how to recognise
emergency animal diseases
Scan QR code
to watch the
demonstration
video.

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
14
Problem
Anthrax has not been diagnosed in SA
for many years, but occasional detections
have occurred in NSW and as well as
isolated outbreaks in WA and QLD.
Anthrax is caused by a bacteria that
affects cattle, sheep, goats and humans.
The bacterium produces spores when
exposed to air that persist in soil for many
years. The disease is spread by contact
with infected animals or by feed and water
that have been contaminated. An outbreak
could be a possible cause of unexplained
sudden death in livestock and can
affect trading opportunities locally and
internationally. More common in summer
but can occur all year round.
Humans can contract anthrax by handling
infected animals, carcasses, animal
products and wool. Take care if handling
animals suspected of dying from anthrax
and contact your medical practitioner
immediately if you have been exposed.
Signs and symptoms
• Sudden death usually first sign,
preceded by rapidly worsening
weakness and staggering.
• Bloody or tarry discharge from mouth,
nose or anus of dead animals.
• Sudden drop in milk production,
red-stained milk or urine.
Diagnosis
• If unexplained sudden death occurs
and anthrax is suspected do not open
or move the carcass. Seek advice
from your local veterinarian or call
your PIRSA animal health office for
assistance diagnosing anthrax with
a ‘penside’ test.
• Diagnosis is most likely in animals
that have recently moved from eastern
states.
• A lack of rigor mortis, with rapid
decomposition of carcass. Pulpy
kidney is often assumed to be the
cause.
Treatment
• Treatment is rarely possible as affected
animals die quickly.
• High doses of penicillin may be
effective in early cases, however may
interfere with anthrax vaccine.
Prevention
• Vaccination is effective, full protection
takes 10-14 days to develop after
administration.
• Vaccination may only occur with the
approval of SA’s Chief Veterinary
Officer (Chief Inspector of Stock).
Emergency animal disease, notiable and zoonotic
Anthrax
If you suspect your stock have
anthrax contact your local PIRSA
Animal Health office immediately
or report to the Emergency Animal
Disease Hotline on 1800 675 888.

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
15
Problem
Bluetongue virus (BTV) is spread by
biting insects such as Culicoides midges,
resulting in production losses and high
death rates (up to 70% in sheep).
Many BTV strains that cause severe
disease are exotic to Australia. Some
BTV strains are present in northern and
north-eastern parts of Australia, but SA is
a transmission free area.
SA’s reputation for high health status
livestock plays a key role in accessing
livestock export trade markets and
provides significant economic benefits
to rural communities. Some countries
only source livestock from areas free of
BTV, highlighting the importance of SA
maintaining its BTV-free status.
Signs and symptoms
• Fever (40 to 41°C), nasal discharge,
breathing difficulty.
• Lameness and reddening around the
coronary band (top of the hoof).
• Swelling of the lips, tongue and head.
• Some animals have a swollen, blue-
coloured tongue, but this isn’t always
seen and is not a reliable sign.
• Rapid weight loss and drop in
production.
• Death rates of 20 to 40% common.
Diagnosis
• If unexplained sudden death occurs
and bluetongue is suspected do not
open or move the carcass.
• To prevent spread of disease it is
critically important to seek advice
from your local veterinarian or call
Emergency Animal Disease Hotline
on 1800 675 888 immediately.
Treatment
• No effective treatment for bluetongue.
Prevention
• Isolation - if an outbreak occurs,
infected animals should be isolated.
• Insecticide - can be applied to reduce
insect numbers and minimise further
spread.
• Good hygiene - minimise the spread of
BTV by not sharing needles between
animals when injecting and thoroughly
washing and decontaminating other
equipment between animals.
Bluetongue
Emergency animal disease, notiable
If you suspect your stock have
bluetongue contact your local
PIRSA Animal Health office
immediately or report to the
Emergency Animal Disease Hotline
on 1800 675 888.

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
16
Foot and mouth disease (FMD)
Problem
Australia is free of foot and mouth disease
(FMD). It is a highly contagious animal
disease that affects cattle, sheep, goats,
pigs, deer and camelids (all cloven-hoofed
animals). An incursion of the virus would
have severe consequences for Australia’s
animal health and livestock trade.
FMD is carried by live animals and in meat
and dairy products, as well as in soil,
bones, untreated hides, and vehicles and
equipment used with infected animals. It
can also be carried on people’s clothing
and footwear.
Signs and symptoms
The most overt sign in sheep may be
lameness. This will appear similar to
endemic disease causes of lameness
like footrot. Close inspection is required
to see some of the other signs of FMD.
Affected sheep may:
• seem depressed
• develop sudden lameness
• be reluctant to stand
• form blisters around top of foot and
between claws
• have lesions on tongue and dental pad
(hard to detect)
• result in significant deaths in lambs.
Diagnosis
• Report these signs immediately to your
veterinarian or the Emergency Animal
Disease Hotline on 1800 675 888.
• Samples will be collected from your
animals and will be sent urgently to
an appropriate animal health laboratory
for diagnostic testing.
Treatment
• No effective treatment for FMD.
• Australia has detailed, well-rehearsed
FMD response plans and arrangements
in place should an outbreak occur.
Prevention
• Farm biosecurity - practice good farm
biosecurity at all times to prevent the
introduction and spread of FMD.
• Buying animals - only buy from
properties with good biosecurity and
disease control practices in place.
• Isolating animals - quarantine new
animals before introducing into existing
flocks.
• Traceability - keep National Livestock
Identification System (NLIS) and
property identification code (PIC)
records up to date.
• Report signs immediately to the
Emergency Animal Disease Hotline
on 1800 675 888.
Emergency animal disease, notiable
If you suspect your stock have
foot and mouth disease contact
your local PIRSA Animal Health
office immediately or report to the
Emergency Animal Disease Hotline
on 1800 675 888.
Scan QR code to learn
more about FMD or visit
www.pir.sa.gov.au/fmd

Sheep diseases & conditions

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
18
Problem
Sheep consume too much high-risk grain
such as wheat or barley which damages
their gut microflora. Some affected sheep
die, others recover slowly but are often
chronically lame.
Signs and symptoms
• Signs occur within 24-36 hours of
changing to a grain rich diet.
• Mildly affected sheep may have
diarrhoea but continue to eat.
• Severely affected sheep may stop
eating, be tender-footed, get up and
down frequently, lie down for extended
periods and grind their teeth.
Diagnosis
• History of eating high risk grain without
being acclimatised and clinical signs.
• On post mortem - damage to the
rumen wall and large amount of whole
grain in first stomach.
Treatment
• Diet - remove animals from grain, feed
good quality hay and provide access
to water.
• Consult veterinarian for a treatment
plan – fluids and sodium bicarbonate
(bicarb soda) can be helpful if given
quickly after overconsumption.
• Antibiotics - often recommended for
surviving sheep that have suffered
rumen damage.
Prevention
• Diet - high risk grains should be
gradually introduced. Avoid sudden
ration change, including grain type and
include grain buffering pellets with the
grain. A provision of extra calcium is
very important (see page 65).
• Access - take care when allowing
sheep to graze newly harvested
paddocks. Prevent sudden access to
unharvested paddocks or spilled grain
(e.g. around silos).
Acidosis (grain overload)

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
19
Annual ryegrass toxicity (ARGT)
Problem
Sheep graze annual ryegrass infested with
a nematode carrying a toxin-producing
bacterium. Severely affected sheep may
die within hours to a week after symptoms
show. Most deaths occur between
October and December when infected
plants have maximum toxicity.
Signs and symptoms
• Signs become obvious when a mob are
driven 100-200 metres, affected sheep
are unable to keep up and have a high-
stepping gait.
• Sheep may go down for minutes
or hours, then return to the mob
appearing normal.
• Severely affected sheep lose
coordination of hind limbs, fall over
with convulsions.
• Arched neck, stiff legs or paddling
legs sweeping the ground.
Diagnosis
• Signs develop four days to several
weeks after sheep graze infected
paddock or are fed infected hay.
• History of eating annual ryegrass
(including toxic hay) and clinical signs.
• On post mortem - rumen, pasture,
hay and grain can be tested for toxic
bacteria.
• Blood test analysis of liver and brain
can confirm the disease.
Treatment
• Access - remove animals from infected
paddock as quietly as possible.
• Humane destruction - sheep unable
to get up within 12 hours should be
humanely euthanised (see page 67).
Prevention
• Plant management - reduce number
of annual ryegrass plants by heavy
grazing in late winter and early spring,
with herbicide treatment and cutting
hay before plants become toxic.
• Introduced feed - all bought feed
should be accompanied by a vendor
declaration.
• Stock monitoring - monitor stock daily
during high-risk months in known
ARGT areas. Early detection will
minimise losses.
Mature annual ryegrass. Photo credit: Andrew Storrie
Annual ryegrass. Photo credit: DPIRD

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
20
Problem
Inflammatory condition of one or more
joints causing pain, lameness and
reduced animal productivity. Can affect
carcass quality leading to trimming and
condemnation.
Signs and symptoms
• First signs are heat and swelling around
one or more joints, commonly knee and
hock joints.
• Restricted and painful movement
of affected joints, mild lameness
developing to permanent lameness.
Diagnosis
• Mostly seen in lambs prior to weaning
due to bacteria entering through broken
skin (e.g. the umbilicus at birth, marking
or mulesing wounds).
• Examining the joints for swelling and
heat.
• On post mortem - bone changes in the
joints, thickened joint fluid and tissue
around the joint.
Treatment
• Consult veterinarian for a treatment
plan - if detected early, antibiotic
treatment can reduce the extent of
damage.
Prevention
• Vaccination - given to ewes before
lambing and lambs at marking to
prevent one of the most common
causes of arthritis, Erysipelothrix.
• Stress - keep stress to a minimum at
lamb marking by avoiding extremes
in temperature, keep droving to a
minimum before and after marking
and allow lambs to mother up as soon
as possible.
• Good hygiene - at marking, avoid
overcrowding or extended holding in
yards and place lambs on their feet
when releasing from the cradle.
Arthritis
Scan QR code to learn
more on VR carcass
feedback tool

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
21
Problem
Sheep ingest a toxin produced by
Clostridium botulinum causing gradual
onset of paralysis and sometimes death.
Most common in pastoral areas in
association with phosphorus deficiency
as stock chew old bones for phosphorus.
Can also occur when sheep ingest
contaminated feed (e.g. rotting vegetable
or animal matter).
Signs and symptoms
• Early signs are staggering, loss of
appetite, drooling, mild excitability,
nervous twitching and jaw champing.
• As the disease progresses sheep
become dull, respiration becomes
laboured and flaccid paralysis of limbs
sets in.
• Affected sheep will go down and die
quietly, generally within two to three
days of initial signs.
Diagnosis
• Based on flock history and clinical
signs.
Treatment
• Humane destruction – severely
affected animals should be humanely
euthanised (see page 67).
• Diet - provide food and water while the
toxin runs its course.
Prevention
• Vaccination - vaccinate at risk sheep
on properties where phosphorus
deficiency or botulism is known to
be a problem. Two doses of botulism
vaccine one year apart provides lifelong
prevention (see page 63).
• Nutrition - address nutritional
deficiencies to prevent bone chewing.
Botulism

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
22
Treatment
• No effective treatment.
Prevention
• Vaccination - in combination with
clostridial vaccine, ensure annual
boosters are given one to six months
before shearing (see page 63).
• Shearing - shear in age groups,
youngest to oldest. Keep yard time to
a minimum for recently shorn sheep.
• Dipping - wait until cuts have healed
(two to four weeks post shearing),
dip oldest animals last, use disinfectant
in the dip.
• Good hygiene - if an abscess is
ruptured at shearing or crutching,
disinfect the handpiece, floor and
anything else contaminated.
Problem
Sheep affected with a bacterial infection
that causes abscesses in the lymph nodes
and lungs. Can affect wool production
and occasionally cause ill-thrift and
wasting. Affects carcass quality leading to
trimming and condemnation.
Signs and symptoms
• Often no obvious signs, but readily
detected in the carcass at slaughter.
• Recently formed abscesses containing
creamy, greenish pus that hardens into
layers, commonly found in lymph nodes
on the shoulder point, groin and lungs.
Diagnosis
• Burst abscesses may be seen at
shearing or CLA is detected in the
carcass at slaughter. Occasionally
abscesses can be found in the brain.
Cheesy gland (CLA)
Scan QR code to learn
more on VR carcass
feedback tool

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
23
Problem
Most common in young sheep during
spring and summer on properties with
sandy, coastal soils. Affected sheep
become deficient in vitamin B12, leading
to reduced energy metabolism, ill-thrift
and anaemia.
Signs and symptoms
• Reduced appetite, ill-thrift (poor doers),
anaemic, sometimes scaley ears and
nose.
• Sheep may have weepy eyes and
photosensitisation (page 44).
Diagnosis
• A blood test can detect vitamin
B12 deficiency.
Treatment
• Vitamin B12 injections, cobalt bullets
and grinders, cobalt supplements in
water or feed.
Prevention
• Vitamin B12 injections - in cobalt
deficient areas, lambs should be
injected at marking, and again two
months later (often in conjunction with
a clostridial vaccine, see page 63).
• Cobalt bullet - weaners remaining on
cobalt deficient pastures can be given
a cobalt bullet at three months old.
Cobalt deciency

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
24
Problem
Most common in lambs before and after
weaning and following transport stress
or overcrowding. Caused by protozoan
parasites that damage the intestinal wall,
leading to severe dehydration, weight loss
and death.
Can affect ewes from pastoral country
relocated to higher rainfall areas and
occasionally sheep in confinement
feeding situations.
Signs and symptoms
• Loss of appetite and weight loss.
• Scouring - often a dark brown liquid
containing flecks of blood or shreds of
intestinal lining.
• Severely affected lambs are obviously
weak, if driven will fall behind the mob
and may go down.
Diagnosis
• Clinical signs.
• Faecal worm testing can detect
coccidiosis but won’t indicate the
extent of damage to intestinal lining.
• On post mortem - examination of the
intestines, particularly large intestine.
Treatment
• Sulphadimidine - given by injection or
drench, two doses are recommended
three days apart. Contact your local
veterinarian.
• Hydration - acutely scouring animals
will benefit from electrolyte therapy to
replace fluids.
• Off label treatment (e.g. Baycox) - can
be used under veterinary prescription.
Prevention
• Diet - feed weaners well with a high
protein diet. Late lambs should not
graze on pastures used by earlier
lambs. Other treatments added
to formulated rations could be
considered.
• Stress - minimise stressful conditions.
• Good hygiene - cocciodiosis is
commonly associated with unhygienic
living conditions.
• Disease management - control
concurrent disease problems,
especially worms.
Coccidiosis

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
25
Problem
Occurs when sheep have insufficient
copper in their diet over a period of
weeks, most common on coastal sandy
soils, sandy loams and swamp land.
Leads to ataxia (uncoordinated
movement) in young animals, steely wool,
abnormal bone formation, ill-thrift and
scours in severe cases.
Signs and symptoms
• Wool abnormalities, ‘steely wool’ - loss
of crimp, hard feel to fleece, reduced
tensile strength and elasticity,
depigmentation of black fleece.
• Diarrhoea, anaemia, sway back and
uncoordinated staggery gait
• Fragile bones that may fracture easily
in young sheep, affected bones are thin
but not deformed.
Diagnosis
• A blood test or tissue analysis -
liver is the best sample to test.
• Pasture analysis.
Treatment
• Supplementation - options include
copper oxide capsules, copper
glycinate injections (e.g. Multimin) and
in-water treatments.
• Pasture or fertilizer treatments.
• Sheep should not be treated with
copper unless deficiency is confirmed
– excess copper can be toxic. Consult
your veterinarian.
Prevention
• Diet - copper absorption is
compromised by a diet high in other
competing minerals.
• Pasture - where concentration of
copper is low, top dress with copper.
• Copper oxide capsules or copper
glycinate injection - can be used in
areas where copper deficiency is
known.
Copper deciency

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
26
Diagnosis
• Based on flock history and clinical
signs.
• On post mortem analysis of liver
samples.
Treatment
• Contact your local veterinarian for
acute cases – treatment is possible
but unlikely to be available in time.
• No effective treatment for chronic
copper poisoning.
• Reduce copper absorption - salt lick
blocks containing molybdenum may
reduce further copper absorption in
the gut.
Prevention
• Diet - avoid feedstuffs and
supplements with extra copper
unless animal has confirmed copper
deficiency.
• Stress - minimise stressful conditions
when handling animals.
Copper poisoning
Problem
Occurs when toxic levels of copper
accumulate in the liver, with sudden death
often the first indication, any survivors
develop jaundice. The three types of
copper toxicity include:
1. Acute copper poisoning - caused by
supplementing sheep that already have
normal to high copper reserves.
2. Chronic copper poisoning - occurs
when excessive copper accumulates
in the liver over a period of several
months.
3. Pyrrolizidine alkaloid poisoning -
certain plants such as heliotrope and
Salvation Jane can cause copper to
accumulate in the liver.
Signs and symptoms
• Acute copper poisoning - severe
diarrhoea (often bluish in colour), red-
brown urine, dehydration, death within
two days of recumbency.
• Chronic copper poisoning - sheep are
disinterested in surroundings, stand
apart from the mob, stop eating, red-
brown urine, jaundice. Death occurs
between three to five weeks after early
signs.
Salvation Jane
Heliotrope. Photo credit: DPIRD

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
27
Treatment
• Usually self-curing.
• Antibiotics - can speed recovery and
minimise risk of flystrike. Contact your
local veterinarian.
• Zinc - in some cases, zinc sulphate
washes can be effective after shearing
Prevention
• Wet sheep - minimise contact between
wet sheep and don’t keep wet sheep in
the yards any longer than necessary.
• Carrier sheep - sheep with mild lesions
are the main source of infection,
spreading the condition when fleece
becomes wet for extended periods.
• Shearing - shear affected sheep last
when dermatitis present to prevent
significant spread via the hand piece
comb.
Problem
A common skin infection caused by
Dermatophilus congolensis bacterium,
mainly in weaners and hoggets (especially
Merinos). Causes elevated body
temperature, hard scabs on skin under the
wool and can lead to occasional deaths.
Can make shearing difficult and result in
flystrike and wool damage. Occurs mostly
in medium to high rainfall areas.
Signs and symptoms
• On non-woollen areas including face
and ears - thin, flat scabs usually
shorter than 1 cm.
• On wool producing skin - a thick
discharge mats wool fibres together at
the base of the staple and dries into a
scab.
• Severely affected sheep have hard
plates of scabs across their back.
Diagnosis
• Examining affected sheep.
• Laboratory confirmation is necessary
for a definitive diagnosis.
• High protein feed may be a factor.
• Unusually wet or humid weather
Dermatophilosis and dermatitis (‘dermo’, lumpy wool)
Photo credit: Dr Will Berry

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
28
Problem
Sheep experience body heat loss
too quickly to maintain normal body
temperature, resulting in collapse,
becoming comatose and then death.
Most common within two weeks of
shearing, especially with extreme cold,
rain and windy conditions.
Signs and symptoms
• Sheep will seek shelter nearby and be
reluctant to move.
• If body heat loss continues sheep will
collapse, become comatose and die
within hours.
Diagnosis
• Consider factors including time
since shearing, available shelter,
current weather, sheep size and
body condition.
Treatment
• Shelter - protect stock from cold
conditions and draughts. Move stock
that have collapsed into a shed.
• Body temperature - if animal is down,
provide body insulation and warmth.
Prevention
• Shelter - recognise high risk weather
and move recently shorn animals to
shelter as early as possible.
Exposure losses

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
29
Diagnosis
• Based on foot examination of lame
sheep - abscess contains light brown
or green pus that will build up over time
and then burst.
• Can be confirmed by laboratory
analysis.
Treatment
• Hoof paring - toe abscesses respond
well to hoof paring which provides
drainage for the pus.
• Antibiotics - heel abscesses are
generally deeper and may require
antibiotic treatment. Contact your local
veterinarian.
• Natural healing - once the abscess
bursts, healing occurs without further
treatment.
Prevention
• Muddy paddocks - keep susceptible
sheep out of muddy paddocks where
possible.
Problem
Bacteria infects the toe or heel after a
foot injury, resulting in severe lameness,
reluctance to stand or move and
sometimes damage to foot joints.
Common in heavier sheep, rams, and
pregnant ewes.
Signs and symptoms
• Usually only one foot is affected -
becoming hot and swollen.
• Toe abscess in front foot - normal
infection site is a crack in the hoof.
• Heel abscess - more common in heavy
adult sheep, starts as a skin infection
between the toes and extends to the
heel.
• Sheep are very lame and lose condition
until the abscess bursts and pus drains
out.
• Distinguishable from footrot due to the
presence of swelling and pus and often
lesions that burst above the coronet.
Foot abscess

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
30
Footrot
Problem
A highly contagious bacterial disease of
one or more feet, resulting in reduced
growth, ewe fertility, growth rates and
productivity.
Flock outbreaks can cause significant
economic loss and incur high costs
associated with controlling and
eradicating the disease.
Signs and symptoms
• Inflamed, red, moist skin and pasty
scum between the digits.
• Chronic and severe lesions with
foul smell.
• Loss of appetite, raised body
temperature, extreme pain.
Diagnosis
• Based on examination of affected feet -
consult your local PIRSA Animal Health
office or veterinarian.
• Laboratory analysis - virulence test on
bacterial swab.
Treatment
A treatment or eradication program for
footrot involves three phases:
1. Control - footbathing or vaccination
during the spread period to reduce
level of infection in the flock to until
eradication becomes feasible.
2. Eradication - remove all infected sheep
during the non-spread period.
3. Surveillance - closely observe the flock
to make sure the disease has been
eradicated and to prevent reinfection.
Notiable disease
If you suspect your stock have
footrot contact your local PIRSA
Animal Health office or report to the
Emergency Animal Disease Hotline
on 1800 675 888.
Scan QR Code to learn more
about ‘Footrot’ or visit
www.sheepconnectsa.com.au/
management/health/foot

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
31
Treatment
• Supplementation - ewes respond
quickly to magnesium injections.
Treated sheep will get up and walk
away within minutes.
• Supplementation - as grass tetany
is often seen in conjunction with
low calcium, a solution containing
both calcium and magnesium is
recommended - this is readily available
from most rural stores.
• Timing - treatment must be given as
soon as possible after initial signs to
be effective.
Prevention
• Stress management - ewes with young
lambs should be handled as little as
possible as physical stress can bring
on grass tetany.
• Supplementation - magnesium
supplements should be available,
usually combined with calcium
supplements during periods of greatest
risk. Magnesium oxide can also be
sprayed on to hay if needed.
• Diet - providing hay when there is lush,
rapid pasture growth can reduce the
risk of disease.
Problem
Sheep develop low blood levels of
magnesium and or calcium, leading to
a stiff gait, paddling convulsions and
sudden death. Most common in prime
lamb mothers within six weeks of lambing.
Can be caused by pasture application
of excessive nitrogenous dressings and
potassium fertilizers.
Signs and symptoms
• Excitable and uncoordinated sheep,
throwing head about, grinding teeth
and shaking with muscle tremors.
• Affected sheep will collapse within
three hours, paddle their feet and froth
at the mouth.
• Violent convulsions and death
occurring four to six hours after
initial signs.
Diagnosis
• Based on flock history, signs shown by
affected sheep and the rapid response
to treatment.
• On post mortem - fluids from inside the
eye tested for magnesium levels.
Grass tetany (hypomagnesaemia)
Photo credit: Dr Bruce Watts

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
32
Problem
A parasitic worm that irritates the airway
causing weight loss and in severe cases
leads to pneumonia and death. Most
common in cooler, wetter areas, in
autumn or winter.
Lambs between four and six months
are most at risk, but sheep of all ages
can be affected.
Signs and symptoms
• Sheep affected by a moderate
infestation will experience coughing,
lethargy and weight loss.
• Severe infestation may cause breathing
difficulty, nasal discharge, ill thrift,
pneumonia, suffocation and death.
Diagnosis
• Lungworms identified in faecal egg
count and culture.
• On post mortem - lungworms found
in the airway and lungs.
Treatment
• Drenching - many sheep drenches are
registered for lungworm treatment.
Prevention
• Drenching - a regular drenching
program can prevent infestation.
Large lungworm

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
33
Listeriosis (circling disease)
Problem
A bacterial infection, causing encephalitis.
Can lead to high death rate including
abortion, stillbirth and neonatal death.
Mostly associated with sheep feeding
on mouldy silage or spoiled hay but can
be sporadic, with no obvious cause.
Listeriosis can present health risks to
humans.
Signs and symptoms
• First signs include depression,
anorexia, disorientation, head tilt and
circling. Animals usually die within a
few days.
• Abortion in ewes in late pregnancy.
• Facial paralysis (often one-sided)
causing droopy ear and eyelid, muzzle
pulling to one side and lack of muscle
tone in lip of the affected side.
• Profuse salivation.
Diagnosis
• Based on clinical signs.
• On post mortem - analysis of the brain
and spinal cord with tissue cultures.
Treatment
• Antibiotics - recovery depends on
early intervention with high doses of
antibiotics, however death can occur
despite treatment in severe cases.
Contact your local veterinarian.
• Diet- remove suspect feed
(e.g. spoiled silage).
• Isolation - separate ill sheep to prevent
spreading the disease between animals.
Prevention
• Diet - take care to avoid feeding
livestock spoiled silage.
• Pasture - avoid boggy pastures and
areas where soil has a high pH level.
Notiable disease
If you suspect your stock has
listeriosis contact your local PIRSA
Animal Health office or report to the
Emergency Animal Disease Hotline
on 1800 675 888.
Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
34
Problem
Liver disease caused by eating lupin
stubbles or lupin grain infected with a
fungal toxin – any lupin stubble exposed
to rain following harvest is potentially
dangerous. Can lead to anorexia, collapse
and many deaths.
Sheep that recover will have chronic
liver damage and do poorly for months,
ewes can be predisposed to pregnancy
toxaemia the following season. Most
common in summer and autumn.
Signs and symptoms
• Affected sheep will stop eating, stand
apart or lag behind the mob and
become staggery when driven.
• Membranes and skin become
jaundiced and may shows signs of
photosensitisation (page 44).
• Some animals die within three days of
eating contaminated lupins, others will
slowly waste away over several weeks.
Diagnosis
• Based on a history of grazing lupin
stubble or eating lupin grain and
clinical signs.
• On post mortem - the animal will be
jaundiced with yellowing fat, skin and liver.
Treatment
• No effective treatment - follow steps
to minimise number of sheep affected
and severity.
• Hydration and shelter - remove the
mob from lupin stubble and grain
and give access to good quality water
and shelter.
• Diet - feed affected sheep a low protein
diet of hay and low protein grains.
Prevention
• Monitoring - check sheep daily when
grazing lupin stubble, drive the mob
for 500 metres to identify any animals
lagging behind.
• Rain - if rain occurs or there is a heavy
dew, remove sheep from lupin stubble.
• Timing - graze lupin stubbles as soon
as possible after harvest and remove
stock once all the grain has been eaten.
• History - avoid grazing sheep with a
history of liver damage.
• Quality and testing - feed sheep good
quality lupin grain. Hay, grain and stubble
can be tested to detect toxin levels at any
livestock feed testing service.
Lupinosis
Photo credit: Dr Belinda Edmonstone

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
35
Diagnosis
• History of ewes grazing in long
stubbles, sometime long grass.
• Scabby mouth infection has been
recorded as a cause.
Treatment
• Antibiotics - condition sometimes
responds to antibiotic injections if
detected early, but generally ewes with
hard, lumpy udders will not return to
function, and should be culled.
Prevention
• Weaning - if older lambs are suckling
ewes, earlier weaning may assist in
reducing cases.
Problem
Inflammation and infection of the udder
causing heat, swelling and lumps leading
to milk supply shutting down.
A common problem in ewes, usually
sporadic, but in some years seems to
affect more ewes than other times.
Signs and symptoms
• Heat and swelling of udder, usually
when lambs are more than four weeks
old, often twins, before weaning.
• Hard and lumpy udder, may be swollen,
painful and hot in early stages
• Milk supply shut down.
Mastitis

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
36
Treatment
• Supplementation - ewes respond
quickly to calcium injections - treated
sheep will get up and walk away
within minutes.
• Supplementation - as milk fever is
often seen in conjunction with low
magnesium, a solution containing
both calcium and magnesium is
recommended – this is readily available
from most rural stores.
• Timing - treatment must be given as
soon as possible after initial signs to
be effective. Consult your veterinarian.
Prevention
• Stress - ewes in last month of
pregnancy or with young lambs should
be handled as little as possible to avoid
physical stress.
• Diet - avoid grazing late pregnant or
lactating ewes on excessively lush
pasture or cereal crops.
• Supplementation - supply a mix of two
parts stock salt to one part stock lime
throughout pregnancy and lactation.
If ewes have been in confinement
consuming over 50% grain-based diet,
stock lime or calcium supplements
should be continuously available.
Problem
Very low levels of blood calcium, most
common in late pregnancy or the first few
weeks after lambing.
Can quickly lead to paralysis and death.
Often seen in conjunction with low blood
magnesium (hypomagnesaemia or grass
tetany). Confusion between milk fever and
pregnancy toxaemia is common.
Signs and symptoms
• Early signs include staggery gait,
muscle tremors, sheep move or
struggle when approached.
• Affected sheep go down in a sitting
position with head turned around to
their flank or may appear very weak
and unable to stand.
• Death will occur within 24-36 hours
of initial signs.
Diagnosis
• Based on flock history, clinical signs
and rapid response to treatment.
Milk fever (hypocalcaemia)
Difference between pregnancy
toxaemia and hypocalcaemia
Pregnancy
toxaemia
Hypocalcaemia
(milk fever)
Gradual onset Sudden onset
Sheep appear dull Sheep appear
alert but may
stagger or
convulse
Sheep are
unresponsive
when approached
Sheep move or
struggle when
approached
Death occurs
within 5-7 days
Death occurs
within 24 hours
Poor response
to treatment
Good response
to treatment

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
37
Problem
Sheep consume plants containing high
nitrate levels, leading to gut inflammation,
reduced oxygen in the blood and death.
Most common when sheep graze lush
pastures containing plants such as
capeweed, oats, canola and wild turnip.
Nitrate concentrations are usually higher
in young plants and following the break of
a drought in the first week after rain.
Signs and symptoms
• Main symptom of affected sheep is
scouring that does not respond to
worm drenches.
• Severely affected sheep may have
brownish or dark discolouration of
mucous membranes (e.g. gums).
• Breathing difficulty, due to changes in
the blood’s oxygen carrying capacity.
Diagnosis
• Based on a history of grazing plants
with a high nitrate level.
• On post mortem - fluids in the eye may
be seen.
Treatment
• No effective treatment.
• Diet - remove animals from high nitrate
feed to stop the scouring.
Prevention
• Diet - avoid grazing pastures
dominated by plants high in nitrate.
Green feed stock blocks are a viable
option on risky pastures.
• Reduce poisoning - provide access
to well dried cereal hay to prevent
further poisoning.
• Supplementation - supplement with
high starch grain (seek expert advice).
Nitrate poisoning
Wild turnip
Capeweed
Canola

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
38
Diagnosis
• Feeling the testicles - a lump can often
be felt in the epididymis (however
not all rams with brucellosis will have
palpable lumps and lumps can be from
other causes).
• A blood test can detect brucellosis two
to three weeks after becoming infected.
Treatment
• No effective treatment in individual
rams.
• Flock control by test and slaughter
program - contact your local
veterinarian for more information.
Prevention
• Buying rams - take care when selecting
rams, check testicles for lumps
and only buy from accredited ovine
brucellosis-free flocks.
• Ram sharing - don’t borrow, lend or
share rams. Maintain secure boundary
fences and check your own rams
before mating.
Problem
Rams develop bacterial venereal infection
leading to infertility and lowered lambing
percentage due to abortions, stillbirths
and birthing of small, weak lambs.
Most common in meat breed rams, less
common in Merinos. Can lead to extended
lambing periods.
Signs and symptoms
Rams:
• Soft, painful swelling of the epididymis
(the duct carrying the sperm from the
testicles).
• Duct doubles in size and hardens,
causing a blockage so no sperm can
be released.
Ewes:
• No obvious signs of ill health.
Ovine brucellosis (Brucella ovis)
InfectedNormal

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
39
Ovine Johne’s disease (OJD)
Problem
Incurable wasting disease with a very long
incubation period, often resulting in death.
Sheep can be infected at any age by
consuming pasture or water contaminated
with faeces.
Infected animals may carry and spread
the disease without ever showing
obvious clinical signs. Factors including
age, breed, stress and the presence of
other diseases can make sheep more
susceptible to OJD.
Signs and symptoms
• The disease has a long incubation
period - most infected sheep show no
signs of illness before two years of age.
• Severe wasting, leading to death within
six to 12 weeks from onset. Sheep
continue to eat and drink normally until
they are too weak to graze.
• Affected sheep will not respond to
drenching (appear wormy).
• Chronic scouring may sometimes be
seen but is not a common symptom.
• Classic symptom of the disease in
a mob is a distinct ‘tail’ with sheep
ranging in condition from good to very
poor.
Diagnosis
• Faecal sampling - a pooled faecal
sample from a selection of sheep
over two years old. Contact your local
veterinarian or PIRSA officer.
• On post mortem - affected animals will
have thickened intestines and enlarged
lymph nodes.
Treatment
• No effective treatment.
Prevention
• Purchase low risk stock - look for
SheepMAP accredited properties,
low-rainfall areas, approved vaccinate
status.
• Vaccination - consider vaccinating your
flock with Gudair
®
(see page 63).
Notiable disease
If you suspect your stock have OJD
report to the Emergency Animal
Disease Hotline on 1800 675 888.
• Mandatory requirements - completed
National Vendor Declarations
(NVD) and National Sheep Health
Declarations (NSHD) are mandatory for
all sheep entering and moving within
South Australia.

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
40
Chronic oxalate poisoning:
• Affected sheep are generally poor doers
and are anaemic with pale membranes.
• Sporadic death occurs within an
affected mob.
Diagnosis
• Based on a history of sheep grazing
high oxalate plants and clinical signs.
• On post mortem - examining the kidney,
pale white streaks may be seen, kidney
may feel gritty when cutting and fluids
in the eye.
Treatment
• Supplementation - can sometimes be
treated with calcium solution (as for
hypocalcaemia, page 36) but usually
ineffective.
• No effective treatment for chronic
poisoning.
Prevention
• Access - prevent hungry sheep
accessing paddocks with large amounts
of soursob or sorrel (e.g. around
shearing sheds).
• Sheep yards - clear sheep yards of
high oxalate plants before allowing
sheep to enter.
Problem
Sheep consume plants with a high
concentration of oxalates (e.g. soursob
and sorrel), resulting in muscle tremors
and a staggered gait, followed by
exhaustion, coma and death.
Often seen from March to June in SA
when soursobs are the only green feed
available before the break of the season.
A common cause of sudden death during
this period.
Signs and symptoms
Acute oxalate poisoning:
• First signs occur within one to three
hours of sheep eating high oxalate
plants.
• Affected sheep have muscle tremors
and a staggery gait, they go down but
will be alert and struggle when handled.
Leg paddling may occur.
• Within hours sheep become exhausted,
stop struggling, sink into a coma and
die soon after. Sheep will often be
found dead without signs of struggling.
Oxalate poisoning
Soursob
Sorrel

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
41
Diagnosis
• Based on a history of sheep grazing
toxic perennial ryegrass and clinical
signs.
Treatment
• Diet - remove sheep from toxic pasture.
Most animals will recover within four
days once removed.
• Stress - avoid disturbing affected
animals and move as quietly as
possible.
Prevention
• Sheep yards - plant cultivars that are
inoculated with non-toxic endophytes.
• Diet - monitor sheep on suspect
pasture and remove quickly if
symptoms develop.
Problem
Sheep consume perennial ryegrass plants
contaminated with a toxin producing
fungus, causing a staggery gait and
leading to productivity losses.
Outbreaks most common during late
summer and autumn months.
Signs and symptoms
• Signs develop slowly over days and
severity greatly varies.
• Mildly affected sheep show trembling
head, shoulder and flank muscles
after exercise.
• Moderately affected sheep stop with
muscle tremors, head shaking and
a staggery, uncoordinated gait after
being driven for 20-100 metres.
• Severely affected sheep will go down
with convulsions and acute muscle
spasms when disturbed.
Perennial ryegrass staggers
Perennial ryegrass

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
42
Diagnosis
• Based on a history of sheep grazing
rapidly growing phalaris pasture and
clinical signs.
Treatment
• No effective treatment for phalaris
poisoning.
Prevention
• Sheep yards - learn to recognise
rapidly growing phalaris and prevent
sheep from grazing on it.
• Access - remove sheep from affected
paddocks immediately and keep off
for two to three weeks (during the
fast-growing phase when plant is most
toxic).
Problem
Sheep consume new growth phalaris
which contains a toxin, causing heart
failure and sudden death.
Most commonly seen after the autumn
break.
Signs and symptoms
• Sudden death, often with convulsions,
within hours of sheep entering a
paddock of young phalaris.
• Affected sheep collapse on their side,
arching neck, paddling legs, champing
jaw, with dilated pupils and profuse
salivation.
Phalaris poisoning
Phalaris

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
43
Diagnosis
• Based on history of sheep grazing
phalaris pasture for prolonged periods
and clinical signs.
• On post mortem - by examining the
brain under microscope.
Treatment
• No effective treatment - affected sheep
should be culled from the mob.
Prevention
• Cobalt bullet - can be used to prevent
phalaris staggers by stimulating
production of toxin-fighting bacteria in
the rumen.
• Vitamin B12 injections - are ineffective
at preventing phalaris staggers.
• Pasture, crop and water supplements -
may not be effective, and may be more
costly.
Problem
Sheep graze phalaris pastures that are
cobalt deficient, causing difficulty eating
leading to significant weight loss.
Most sheep will survive but never fully
recover.
Signs and symptoms
• Affected sheep are uncoordinated with
head nodding, muscle tremors and a
stiff gait.
• If driven, sheep will go down with
convulsions but will get up and walk
away soon after.
• Some sheep can die while having
convulsions, others may die from
accidents caused by staggering.
Phalaris staggers
Phalaris

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
44
Diagnosis
• Based on examining affected sheep.
Treatment
• Identify cause - first step is to address
the underlying cause of the condition.
• Shelter - protect affected animals from
direct sunlight.
• Nursing - confine to shearing shed
while recovery takes place and provide
good quality hay.
• Medication - affected animals
may benefit from antibiotic, anti-
inflammatory or antihistamine
injections. Consult your veterinarian.
Prevention
• Grazing - avoid long term or repeated
grazing of pastures or stubbles
containing toxic plants such as potato
weed, which cause chronic liver
damage.
• Diet - allow access to hay or straw
when introducing sheep to immature,
lush, green pastures. If symptoms seen,
remove sheep immediately from this
pasture.
Problem
Photosensitisation is a symptom of
several diseases such as, liver damage
and plant toxicity. Sheep consume
immature forage causing Phylloerythrin
production that results in skin that is
overly sensitive to sunlight, impacting
wool quality and growth rates.
Most common in spring, on fast growing
lush pasture and sometimes associated
with aphid infestations. Cases can be
mild and recover quickly or severe,
resulting in death.
Signs and symptoms
• Early signs include restlessness,
seeking shade, shaking their head and
rubbing eyes and ears.
• Later signs range from mild to severe
sunburn, loss of appetite, jaundice
and death.
• Areas of skin not covered by fleece
are most affected, such as face, ears
and vulva.
• Fluid can build up under the skin
causing swelling of the face - swollen
eyelids with tears dribbling down the
cheeks and swollen ears may droop
and be covered in fine scabs.
Photosensitisation

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
45
Diagnosis
• Based on examining the eye
of affected sheep.
Treatment
• Most cases recover without treatment
in two to three weeks.
• Inspection - inspect eye for irritants
and remove if possible.
• Antibiotic spray or powder - two
doses are recommended, 48 hours
apart. Antibiotic spray or powder is
readily available.
• Antibiotic ointment and injections -
can be more effective than spray or
powder, especially in severe cases,
but must be used under veterinary
advice.
Prevention
• Yarding - avoid yarding sheep as
dust and flies can make the infection
spread through the mob.
• Flies - manage flies in yards if
possible.
Problem
A common and painful bacterial eye
infection that can cause blindness and
affect weight gain.
Sheep are most at risk when exposed
to hot and dusty conditions and flies.
Signs and symptoms
• Early signs include inflammation
of eye membranes and clear tears
running down the cheek.
• Cornea (clear eye surface) develops a
blue haze, becoming cloudy and white
over three to four days. Shallow ulcers
may develop on cornea.
• Disturbed vision - if the disease
spreads to both eyes, affected sheep
will become blind and begin to lose
weight.
• As the eye heals, blood vessels grow
onto the cornea making the eye
appear pink.
Pinkeye

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
46
Diagnosis
• Based on history and clinical signs.
• On post mortem - very dark and
consolidated lungs.
Treatment
• Antibiotics - treatment can aid
recovery. Contact your local
veterinarian.
Prevention
• Driving - drive sheep slowly and allow
sheep to walk slowly back to paddock
after yarding.
• Yarding - avoid overcrowding and
prolonged yarding. Avoid hot, dry and
dusty conditions. If unavoidable, work
early in the morning and hose yards to
reduce dust.
• Stress - avoid mixing mobs and sudden
diet changes. Provide shelter, good
nutrition, appropriate vaccinations,
drenching and supplements.
• Off label vaccination programs - cattle
vaccines can be useful in some cases -
consult your local veterinarian.
• Drenching - be careful not to lift a
sheep’s head too high and avoid plunge
dipping thirsty sheep.
Problem
Inflammation of the lungs, causing
breathing difficulties, leading to
productions losses and sometimes death.
Caused by bacteria and viruses in sheep
with compromised immunity (weaners are
most susceptible).
Most common during summer through
autumn, particularly in hot, dry and dusty
conditions.
Signs and symptoms
• Affected sheep may show signs of
cough, nasal discharge and lag behind
the mob.
• Mild cases can go unnoticed, but
growth rates are affected.
• A large proportion of the mob can
be affected with only a few deaths -
feedlot conditions will often see higher
number of deaths, very quickly.
• Signs may subside after four to six
weeks, but lasting adhesions in the
lungs and chest (pleurisy) are often
detected at the abattoir and trimmed
from the carcass.
Pneumonia
Scan QR code to learn
more on VR carcass
feedback tool

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
47
Diagnosis
• Based on clinical signs and response
to treatment in cases found early.
• On post mortem - by examining the
brain.
Treatment
• Supplementation - sheep respond
immediately to thiamine or vitamin B1
injections, available from most rural
stores or veterinarians. Some sheep
may require follow up treatment. Giving
thiamine powder orally in water solution
is also effective but slower.
• Humane destruction - sheep that are
down and do not respond to treatment
may have irreversible brain damage
and should be humanely euthanised
(see page 67).
Prevention
• Supplementation - thiamine powder
should be added to drinking water in
high-risk situations, or if cases occur.
Contact your local PIRSA Animal
Health office or veterinarian for advice.
Problem
A nervous disease of the brain, caused by
thiamine (vitamin B1) deficiency, resulting
in ear twitching, apparent blindness, star
gazing and sometimes, death.
May occur in sheep on a high grain diet
and diets including high thiaminases
plants (such as, bracken). Most common
in lambs in feedlots.
Signs and symptoms
• Early signs include listlessness and
loss of appetite. Sheep will separate
from the mob, appear blind and wander
aimlessly, stand still, or be found up
against a fence.
• Affected sheep will keep head lowered
to the ground or appear to be ‘star
gazing’ with a fixed stare into the sky
over the horizon, or have front legs
stretched out and head arched back.
• Severely affected sheep will go down
and if startled, start galloping leg
movements and have convulsions.
• If left untreated, sheep will get weaker,
sink into a coma and die quickly.
Polioencephalomalacia (PEM, star gazing disease)

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
48
Diagnosis
• Based on flock history, clinical signs
and eye fluid examination.
• On post mortem - liver will be pale
yellow, greasy and soft, carcass will
have plenty of fat, usually full-term twin
lambs inside.
Treatment
• Timing - treatment must be given as
soon as possible after initial signs to be
beneficial. Persistent and appropriate
treatment may save some ewes, but
success diminishes the longer they are
left untreated and recumbent. Consult
your veterinarian for treatment and
management of an outbreak.
• Glucose and hydration - treatment
can include glucose and rehydration
solutions, such as Vytrate and Ketol
(propylene glycol) administered orally
– readily available from most rural
stores. Repeated treatments may be
necessary.
• Humane destruction - if recumbent
ewes do not respond with three
hours of treatment, euthanasia is
recommended.
Problem
Very low blood sugar in ewes due to
inadequate energy in feed and high energy
demands of pregnancy, leading to lethargy,
weight loss and often death.
Most common during last six weeks of
pregnancy or immediately after lambing. If
energy requirements are not met by feed
intake, the ewe will break down her own
body tissues - a rapid breakdown of tissue
results in an accumulation of toxins.
Older ewes carrying multiples are most at
risk, particularly if overfat or feed intake is
suddenly interrupted in late pregnancy (e.g.
by yarding). Often combined with calcium
deficiency (hypocalcaemia) (see page 36).
Signs and symptoms
• In affected flocks, the disease usually
appears as a continuing outbreak over
two to three weeks.
• Early signs include dullness, loss of
appetite and lagging behind the mob
when driven.
• As the disease progresses, affected
ewes will stand alone, appear dopey and
not move when approached. If driven, will
appear blind, stumble and collapse.
• Eventually, affected ewes will become
comatose and die
Pregnancy toxaemia (twin lamb disease)
Prevention
• Diet - give pregnant ewes best paddock
feed available during month prior to
lambing. Provide supplementary feed
during last few weeks if needed (take
care if introducing grain, see page 64).
• Condition score - in flocks where multiple
births are expected, ewes should be
a minimum condition score 3, and no
more than condition score 4. Consider
scanning and segregating twins, singles
and empties for better feeding outcomes.
• Stress - minimise physical stress by
avoiding unnecessary mustering, yarding
or time off feed.
Difference between pregnancy
toxaemia and hypocalcaemia
Pregnancy
toxaemia
Hypocalcaemia
(milk fever)
Gradual onset Sudden onset
Sheep appear dull Sheep appear
alert but may
stagger or
convulse
Sheep are
unresponsive
when approached
Sheep move or
struggle when
approached
Death occurs
within 5-7 days
Death occurs
within 24 hours
Poor response
to treatment
Good response
to treatment

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
49
Diagnosis
• Based on a history of sudden death
while on a high-risk diet.
• On post mortem - by examining
intestine contents and isolating the
toxin brain and urine.
• Pulpy kidney is commonly assumed
cause of sudden death in sheep
where no investigation is conducted.
Unexplained sudden deaths can also
be caused by other diseases, including
anthrax (see page 14).
Treatment
• No effective treatment.
Prevention
• Vaccination - effective in preventing
pulpy kidney (see page 63). Vaccinate
sheep at least 10 days prior to heavy
grain feeding or introducing to a
feedlot. Vaccination can be effective in
the face of an outbreak.
• Diet - avoid sudden diet changes,
ensure grain is introduced correctly
(see page 64).
Problem
A clostridial (bacterial) disease that
mostly affect lambs grazing lush
feed, causing sheep to go down with
convulsions and leading to rapid death.
Can also occur in sheep of all ages,
especially if consuming grain.
Most common in flocks with an
inadequate vaccination program.
Signs and symptoms
• Affected sheep are usually found dead
due to rapid onset of the disease.
• Death can occur within hours of initial
signs - sheep will not survive longer
than 24 hours.
• Initial signs include dullness followed
by sheep going down with convulsions
and frothing at the mouth.
Pulpy kidney (enterotoxaemia)

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
50
Diagnosis
• Based on a history of grazing the toxic
plants and clinical signs.
• On post mortem - in cases of chronic
copper poisoning, fat and skin of the
carcass will be severely jaundiced.
• On post mortem - in cases of chronic
ill-thrift and photosensitisation, the liver
will be darker and harder with blunt or
lumpy edges.
Treatment
• No effective treatment.
• Humane destruction - sheep that
survive a severe poisoning incident
will have irreversible liver damage
and should be humanely euthanised
(see page 67).
Prevention
• Access and weed management -
prevent sheep accessing paddocks
with the toxic weeds.
Problem
Sheep consume plants containing
toxic alkaloids, such as Salvation Jane
(Patterson’s curse), heliotrope (potato
weed) and caltrop, resulting in chronic
ill-thrift, photosensitisation and permanent
liver damage that is cumulative over the
life of the animal.
Signs and symptoms
• Affected sheep will show signs of
chronic copper poisoning (disinterested
in surroundings, standing apart from
the mob, loss of appetite, red-brown
urine, jaundice - see page 26) or
chronic ill thrift and photosensitisation
(see page 44).
Pyrrolizidine alkaloid poisoning
Salvation Jane
Caltrop
Heliotrope

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
51
Scabby mouth
Problem
A highly contagious viral disease
affecting the skin, particularly the mouth
and nostrils, resulting in unwillingness to
eat. It is a hardy virus that can survive on
the ground for years. Also affects goats
and humans.
Signs and symptoms
• Can affect multiple animals, infection
is commonly seen on lips, in corners
of the mouth.
• Can also be found on ewes’ teats,
skin around the coronet, bulbs of the
heels and ears from wounds caused
by ear tags.
• Infection begins with a clear sticky
discharge, hardening into a thick
brown scab, firmly attached to the
skin. If the scab is not knocked or
pulled off, it generally dries up and falls
off in two to three weeks.
Diagnosis
• Based on examining infected sheep
- scabby mouth scabs are quite
distinctive. If necessary, diagnosis
can be confirmed by submitting scab
material to a laboratory.
Treatment
• Most cases recover without treatment
within three weeks.
• Flystrike - put precautions in place
against flystrike (see page 59).
• Diet - provide soft feed as affected
sheep may be reluctant to eat dry
coarse feed.
Prevention
• Vaccination - a scabby mouth vaccine
containing the live virus is effective in
preventing the disease (see page 63).
Avoid vaccinating ewes with lambs at
foot.
Zoonotic disease
Precautions must be taken when
handling infected sheep to prevent
health risks to humans.

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
52
Treatment
• Supplementation - selenium can be
administered to affected sheep by
injection or as a drench.
• Note: there is a very small safety
margin when administering selenium.
Treatment should only be given
following muscle disease diagnosis
and in strict accordance with
manufacturer’s advice.
Prevention
• Supplementation - vaccination,
drenching and slow-release pellets are
effective in preventing deficiency.
• Seek expert advice - if you suspect
selenium deficiency in your flock you
can discuss diagnosis, sampling and
management with your local PIRSA
Animal Health office or veterinarian.
• Note: care must be taken to not
overdose by supplementation with
repeat vaccination and drenching.
Problem
Sheep suffer deficiency in selenium or
vitamin E, impacting lifetime growth rates
and can lead to starvation, heart failure
and death from exposure or predation.
Most common in spring born lambs
at three to four weeks old, on clover-
dominant pastures. Deficiency may be
subtle and result in several health issues
in the flock, particularly in high rainfall
areas with heavy red or dark clay soils.
Signs and symptoms
• Affected lambs walk with a stiff gait
and appear weak.
• Severely affected lambs can die from
starvation, exposure or predation.
• Some lambs show laboured breathing
due to respiratory or cardiac muscle
failure. Pneumonia is a secondary risk
in these lambs.
Diagnosis
• Tentative diagnosis on post mortem -
examining the carcass for pale muscle
tissue.
• Blood and tissue tests can confirm the
disease - biopsies in live animals can
be performed by veterinarians.
Selenium deciency (white muscle disease)

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
53
Tapeworm cysts (bladder worm, sheep measles, hydatids)
Problem
Numerous diseases occur in sheep due
to different tapeworm species, including
bladder worm (Taenia hydatigena), sheep
measles (Taenia ovis) and Hydatids
(Echinococcus granulosus).
In all cases sheep show no clinical signs
and tapeworm goes undetected until
slaughter when affected organs are
condemned. If sheep measles is found
with five or more cysts present, the
carcass is condemned. Hydatids has
been detected in kangaroos in some
areas in SA.
Care must be taken treating working dogs
in these areas due to health risks present
to humans.
Symptoms
• Affected sheep show no clinical signs
of tapeworm.
Diagnosis
• Cysts on organs (liver, lungs and brain)
and muscles indicate tapeworm -
usually not identified until slaughter.
Treatment
• No effective treatment.
Prevention
• Worming - all dogs on farm should be
wormed monthly with a tapewormer
(must contain praziquantel).
• Contact your local PIRSA Animal
Health office for information on hydatid
detections in SA.
• Raw meat - don’t feed raw meat or
offal to dogs. Instead, cook through
or freeze at -10
oC
for ten days.
• Carcass management - burn or bury
carcasses to prevent scavenging.
Zoonotic disease
Precautions must be taken to prevent
serious health risks to humans.
Scan QR code to learn
more on VR carcass
feedback tool

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
54
Diagnosis
• Based on clinical signs.
Treatment
• No effective treatment.
Prevention
• Vaccination - is highly effective in
preventing tetanus. (See page 63
for more information on best practice
vaccination programs).
• Good hygiene - at lamb marking is
important in preventing tetanus.
Problem
A clostridial (bacterial) disease that
mostly affects lambs within three weeks
of marking (sheep of any age are at risk
following a wound), causing muscle
spasms, restricted jaw movement, usually
resulting in death within three to four days.
Most cases of occur in flocks with an
inadequate vaccination program. The
bacteria is widespread in the environment
and can survive in the soil for many years.
Signs and symptoms
• Early signs include walking with a stiff
gait.
• Muscle spasms including head
tremors, tightly closed jaw and pricked
ears.
• The tail is generally held out and legs
appear stiff - known as the ‘sawhorse’
posture.
• As disease progresses sheep will go
down with intermittent convulsions and
die within three to four days.
Tetanus (lockjaw)

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
55
Prevention
• Separate pregnant ewes - aborting
ewes are the main source of infection
for other ewes. Keep pregnant ewes
as far away from infection by mid-late
pregnancy and reduce stocking rates
as much as possible.
• Mixing infected ewes - if a diagnosis is
confirmed, infected ewes can mix with
ewes that have already lambed but not
pregnant ewes.
• Observing low lambing rates - if
lambing rates are below expected, this
condition could be operating in a low
grade, subclinical manner - seek advice
from your veterinarian.
• Vaccination - is effective in preventing
vibriosis (see page 63).
Vibriosis (Campylobacteriosis)
Signs and symptoms
• First signs of an outbreak are abortions
in the yards or ewes with blood-
stained breech wool. Early abortions
can go unnoticed as foetuses are only
centimetres in length.
• Most aborting ewes show no signs of
ill health and develop strong immunity
and subsequent fertility is good.
Diagnosis
• Based on flock history and examining
the aborted foetus and placenta (foetus
may have yellow and white 1-2 cm
patches on the liver).
• Can be confirmed by testing aborted
foetus and bacterial culture in
laboratory.
• Blood tests on ewes suspected of
having aborted.
Treatment
• No effective treatment - seek advice
from your local PIRSA Animal Health
office or veterinarian. It is essential to
collect and dispose of aborted lambs
hygienically.
Problem
Campylobacteriosis is the most common
cause of abortion outbreaks in sheep.
Sheep are infected by a bacterium
(campylobacter), shed in faeces,
resulting in abortion from three months
of pregnancy and can result in significant
lamb losses. It can be introduced to
susceptible flocks by carrier sheep
showing no symptoms and birds.
Outbreaks may re-occur every few years
due to lack of immunity in replacement
stock. In some intensive management
situations, abortions ‘storms’) have
occurred, such as in pregnant ewes
confined after fires.
If abortion storms occur, immediately
report to local PIRSA Animal Health office.
Zoonotic disease
Precautions must be taken when
handling foetuses and sheep to
prevent health risks to humans.

Other conditions

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
57
Treatment
• Chemical treatment - directly on the
sheep via backliner, plunge dipping
and jetting.
Prevention
• Good biosecurity - avoid introducing
lice into your property, be prepared
with a biosecurity plan.
• Learn about common sources of
infection (including, infested stray
sheep entering your property,
purchased sheep, sheep that may have
missed previous lice treatments).
• Fencing - stock proof all boundary
fences.
• New stock - closely inspect all
introduced stock.
• Treatment and control plan - implement
a lice treatment and control plan.
Problem
Sheep body louse or chewing lice
(Bovicola ovis) is a small insect that
is responsible for the majority of lice
infestations in Australian sheep.
An infestation of lice can reduce clean
fleece weight by up to 1 kilogram and
causes cotted, yellow wool, resulting in
price discounting.
Wool shedding sheep can still become
infested with sheep lice, despite their
wool shedding traits.
Signs and symptoms
• Lice, in low numbers, can be extremely
difficult to detect on sheep.
• Affected sheep can show signs of
rubbing, often indicated by wool pieces
on fences and yards.
Diagnosis
• Close inspection of sheep, often
requiring a magnifying glass is the only
accurate method to detect lice.
Sheep lice
Scan QR code for
the ‘Liceboss’ online
resource or visit
www.liceboss.com.au

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
58
Treatment
• Treatment is dependent on the type
of worm present, the class of sheep
and the region in which the sheep are
located.
• Drenching - typical treatment is a
chemical drench, applied orally.
Prevention
• Treatment and control plan - including
preparing low worm-risk paddocks,
grazing and nutrition management,
breeding and using chemical
treatments.
• Tailored solution - the most effective
approach is a solution tailored to
your specific situation, using the
tools and information available at
wormboss.com.au.
Problem
The most important roundworms
(nematodes) in sheep in Australia are
Barber’s pole worm (Haemonchus
contortus), black scour worm
(Trichostrongylus colubriformis and
T. vitrinus spp.) and brown stomach worm
(Teladorsagia circumcincta), causing
scouring, ill thrift resulting in weight loss
and occasionally death.
Signs and symptoms
• Key signs include bottle jaw, humped
back from abdominal pain, coughing
and pneumonia, anaemia, lethargy,
scours, weight loss and occasionally
death.
Diagnosis
• Faecal egg count to detect presence of
and type of worms present.
• Worm count at post mortem.
Sheep worms
Scan QR code for the
‘Wormboss’ online
resource or visit
www.wormboss.com.au

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
59
Treatment
• Shear and dress - remove wool from
around the strike area close to the skin
and apply registered flystrike dressing.
• Remove sheep - remove affected
sheep from the flock as struck sheep
can attract more flies.
• Culling - cull struck sheep from the
flock - susceptibility to flystrike is
heritable.
Prevention
• Planning - plan shearing, crutching and
lambing dates to minimise potential
flystrike occurring.
• Genetics - select genetics for low
wrinkle and flystrike resistant sheep.
• Treatment plan - develop a strategy for
chemical treatment, managing potential
chemical resistance and maintaining
accurate treatment records to avoid
chemical residues in wool sold.
Problem
Flystrike in sheep is caused by Lucilia
cuprina resulting in significant loss of
productivity and in severe cases, death.
Signs and symptoms
• Sheep appear generally sick and
restless and often become separated
from the flock.
• Flystrike affected wool becomes dark,
moist and foul smelling.
• In severe cases, maggots will be found
at the affected area with visible trauma
to the skin.
Diagnosis
• Identifying maggots on the skin under
close inspection.
Flystrike
Scan QR code for
the ‘Flyboss’ online
resource or visit
www.flyboss.com.au

Management guides

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
61
Good biosecurity principles
• Principle 1: Record all livestock
movements, purchases, sales and
treatments.
• Principle 2: Always buy livestock from
reputable sources.
• Principle 3: Make sure all purchased
livestock have an animal health certificate
from the vendor.
• Principle 4: Develop a treatment program
for new livestock (e.g. drenching, lice
treatment, vaccination).
Farm visitors
Visitors to your farm pose a potential risk of
introducing diseases and pests. It is important
to do a risk assessment of visitors including
whether they have recently been overseas.
• Principle 1: Keep visitors (friends, agents,
etc) out of livestock production areas.
• Principle 2: If people need to access
production areas, clean all tools, equipment,
and footwear.
• Principle 3: Visitors returning from overseas
travel should avoid contact with livestock
and farms for 7 days.
Remove excess foreign material from
the sole of your boots away from the
production zone and washing area
- you may do this by banging boots
together or using a tool to scrape out
the boot tread.
Wash boots/footwear in a bucket
filled with water and use a scrubbing
brush if required to remove all
excess foreign material. Clean any
tools or equipment in the same
bucket of water.
Finally, rinse clean boots/footwear
and tools in a separate bucket of
disinfectant or use a spray bottle
containing disinfectant.
Carefully and mindfully dispose
of dirty water and waste
disinfectant.
Good biosecurity
Boot wash procedure
On-farm biosecurity involves proactively managing and preventing risks caused by weeds, pests and diseases entering, emerging,
establishing or spreading.
2
4
1
3

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
62
Why register?
All producers in Australia must have
a farm biosecurity plan (Livestock
Production Assurance requirement).
One Biosecurity will generate an
approved biosecurity plan in a simple,
free, online process.
Other benefits include:
• generating an Animal Health
Declaration
• assisting with purchasing decisions
• providing credible assurance to
existing domestic and international
markets
• improving government and
industry disease surveillance and
early detection of animal health
emergencies.
Contact
For help registering your property
and completing your risk assessment
contact 1BSuppor[email protected]v.au or
call 08 8429 3300.
What is One Biosecurity?
The One Biosecurity program is free for
South Australian livestock producers and
has been designed to help producers
register, manage, and promote on-farm
biosecurity. The platform can also be
used as a resource for guidelines and
advice on livestock diseases.
Developed in collaboration with key
industry groups, One Biosecurity
recognises the important role producers
have in protecting and growing our state’s
livestock industry.
Once registered, you will be self-guided
through two core online components:
• Biosecurity Practices Questionnaire
(score 1-5 stars)
• Endemic Disease Risk Rating modules
(Risk Rating for a series of diseases
including Ovine Johnes, footrot, lice,
pestivirus and ovine brucellosis).
One Biosecurity
Scan QR code to
learn more about
One Biosecurity or visit
www.onebiosecurity.
pir.sa.gov.au

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
63
Vaccination is the key to preventing
many sheep diseases.
Why vaccinate?
Sheep are vaccinated to protect against
some of the common serious infectious
diseases.
Vaccination stimulates the body’s defence
system to build immunity to a particular
disease or combination of diseases.
Vaccinations should be administered
to livestock as part of an annual
management plan.
Vaccination
What vaccines are available?
Vaccine Diseases Vaccine program
3-in-1 clostridial + CLA Tetanus, pulpy kidney and
cheesy gland
Two doses at least four
weeks apart, annual boosters
(sheep and lambs)
5-in-1 clostridial Pulpy kidney, tetanus,
blackleg, malignant oedema,
black disease
Two doses at least four
weeks apart, annual boosters
(sheep and lambs)
6-in-1 clostridial + CLA Pulpy kidney, tetanus,
blackleg, malignant oedema,
black disease + cheesy gland
Two doses at least four
weeks apart, annual boosters
(sheep and lambs)
8-in-1 clostridial 5-in-1 (plus, helps prevent
lamb dysentery and post
parturient gangrene in ewes)
Two doses at least three to
four weeks apart
Arthritis (e.g. Eryvac) Erysipelas arthritis Two doses at least three to
four weeks apart
Scabby mouth
(e.g. Scabigard)
Scabby mouth Single dose for life
OJD (e.g. Gudair) Ovine Johne’s disease (OJD) Single dose for life
Footrot Footrot Two doses at least six weeks
apart. (Only through vets with
CVO approval).
Source: MLA https://www.mla.com.au/globalassets/mla-corporate/research-and-development/program-areas/animal-health-welfare-and-
biosecurity/210517-vaccination-in-sheep-flocks.pdf
Note: clostridial vaccines are available with or without added B12 and selenium.
Scan QR code to learn
more or visit
sheepconnectsa.com.au/
management/health/
vaccination

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
64
3. Gradually introduce grain
Gradually introduce grain over a period
of two weeks. Feed good quality hay,
not straw. The digestibility of the hay
is important.
4. Ration additives
Ensure grain rations are balanced and
consider a good composite premix.
Premixes can have mineral and trace
element supplements, buffers and
anti-coccidials. Seek nutritional advice.
5. Shade and shelter
Protect sheep from the elements and
provide shade.
6. Quality cereal hay
After implementing the changeover
strategy, a lamb’s diet should be made up
of at least 10% good quality cereal hay.
7. Observe and record
Observe sheep and keep good records of
any deaths (include as much information
as possible). Feedlot problems can
escalate quickly and involve large
numbers of stock - seek help and
veterinary advice early.
Steps for heavily supplementing diet with
grain or introducing grain to sheep in a
feedlot situation.
1. Background feeding
Early background feeding in the paddock
is important. Use the same type of
grain that will be fed in the feedlot to aid
digestion and help sheep adjust to the
new, predominantly grain, diet.
2. Vaccinate
Administer 3-in-1 or 6-in-1 vaccine at
least ten days before heavy feeding or
introducing to the feedlot to prevent
serious risks, including pulpy kidney.
Apply best practice methods to treat
and prevent lice and flystrike, drench as
required and supplement with vitamin
B12, A, D and E as needed.
Grain introduction

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
65
How do you do this?
• All livestock movements to a different
PIC must have a national vendor
declaration (NVD) and National Sheep
Health Declaration, even if the owner
of the livestock does not change.
• The NLIS database must be notified
when one or more sheep are moved
to a different PIC.
• The NVD details are included on
the livestock transfer on the NLIS
database.
• Access the NLIS database at
www.nlis.com.au
Support
Call Integrity Systems Company (ISC)
Support on 1800 683 111 for database
issues, LPA, eNVDs or PIRSA NLIS
Help Desk on 1800 654 688.
The National Livestock Identification
System (NLIS) is Australia’s system for
identifying and tracing cattle, sheep
and goats. The database records the
lifetime location data and movement
of all livestock in Australia using
individual identification (cattle) and flock
identification (sheep and goats). All
physical locations are identified by
a Property Identification Code (PIC).
When livestock are moved to another
PIC, being sold, adjusted or relocated
to another property, this movement must
be recorded on the NLIS database.
Who is responsible?
Depending on the livestock movement
that is occurring, different parties are
responsible for recording livestock
movements on the NLIS database, as
either mob-based movements with visual
NLIS tags or individual animal movement
with electronic RFID NLIS tags.
NLIS obligations
SaleyardSaleyard
Online
purchases
Online
purchases
AbattoirAbattoir
Private
purchases
Private
purchases
Show/
Field Day
Sporting
Event
Show/
Field Day
Sporting
Event
Moving
between
two
properties
Moving
between
two
properties
On Property
auctions
On Property
auctions
Agistment
movements
Agistment
movements
OthersOthers
YOUYOU
webaddress.com.au
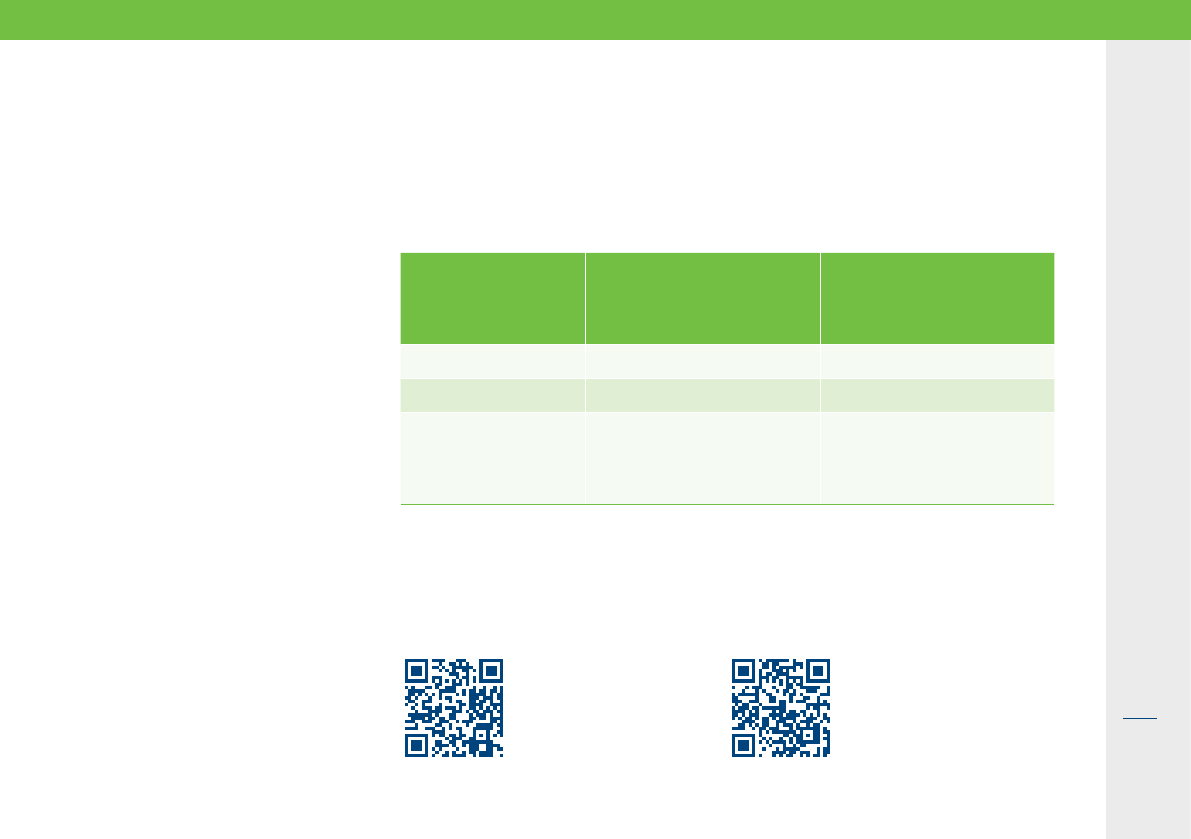
Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
66
Maximum time off water
It is recommended to take sheep off green feed and water at least 12 hours prior
to transport. Dry feed, such as hay, can be offered prior to loading even if water
has been withheld.
Class of animal Maximum time off water
(includes mustering/time
in yard prior to loading
Required spelling period
(to rest + food ad water
when maximum time off
water has been reached)
Sheep over 4 months 48 hours 36 hours
Lambs under 4 months 28 hours 12 hours
Ewes known to be
more than 14 weeks
pregnant, but not in
the last 2 weeks
24 hours 12 hours
It is an offence to load or transport
an animal in a way that causes it
unnecessary harm. The person in charge
of the animal is responsible - if in doubt,
leave it out.
An animal is not fit to load if it:
• is not strong enough to undertake
the journey
• cannot walk normally, bearing weight
on all legs (e.g. old or new fractures,
injury, deformity, foot abscess, joint
infection)
• is severely emaciated or visibly
dehydrated
• is suffering from severe visible
distress or injury (e.g. swollen pizzle,
exhaustion, panting, flystrike)
• has a condition that could cause it
increased pain or distress during
transport (e.g. ingrown horn, cancer
(vulva, udder, ear), swollen testicles,
advanced mastitis
• is blind in both eyes
• Is within two weeks of lambing and
the estimated journey time or time off
water is likely to exceed four hours.
Fit to load
Scan QR code to
learn more or visit
www.mla.com.au/
isitfittoload
Scan QR code for ‘Australian
Animal Welfare Standards and
Guidelines for Sheep’ or visit
www.animalwelfarestandards.
net.au

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
67
Using a firearm or captive bolt:
• the poll method (B) is preferable to the
frontal shot (A) for killing sheep.
Bleeding out by neck cut:
• can be used to destroy sheep if a
firearm or captive bolt is not available.
Ensure both jugular veins and carotid
arteries are severed using a suitable
and sharp knife. It is not advised to
sever the spinal cord or break the neck.
Confirming death after any
method of destruction is
essential:
• check for loss of consciousness and
deliberate movement, dilated pupils,
absence of the ‘blink’ reflex when the
eyeball is touched and absence of
breathing, jaw tone and tongue tone.
Humane destruction

Acknowledgments
& further reading

Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
69
Acknowledgments & further reading
Allan, S 2010, Foot Abscess in Sheep,
NSW DPI Primefact 7, NSW.
Animal Biosecurity Unit 2008, Ovine
Johne’s Disease, NSW DPI Primefact
661, NSW.
Australian Animal Welfare Standards
and Guidelines - Land Transport of
Livestock, Animal Health Australia (AHA)
2012, Canberra.
Brightling, A 2006, Livestock Diseases
in Australia, C H Jerram and Associates
Science Publishers, Australia.
Butler, R 2008, Ovine Brucellosis,
Department of Agriculture and Food
Farmnote 334, WA.
Chester, L 2010, Sheep Welfare –
Avoiding Losses due to Hypothermia,
Department of Agriculture and Food
Farmnote 453, WA.
Cotter, J 2011, Sheep Lice – Spread and
Detection, Department of Agriculture
and Food Farmnote 478, WA.
Erickson, A 2010, Hydatid Disease,
Department of Agriculture and Food
Farmnote 448, WA.
Hungerford, TG 1990, Hungerford’s
Diseases of Livestock Ninth Edition,
McGraw-Hill Book Company Australia
Pty Limited, NSW.
Gardner, J 2006, Pregnancy Toxaemia
and Hypocalcaemia of Ewes,
Department of Agriculture and Food
Farmnote 105, WA.
Jordan, D 2003, Livestock
Health Pregnancy Toxaemia and
Hypocalcaemia, DPI &F QLD Primenote
SW0107, QLD.
Joshua, E, Junk, G & Levot, G 2010,
Sheep Lice, NSW DPI Primefact 483,
NSW.
Karlsson, J Evans, D 2007, Lumpy
Wool (Dermo) & Fleece Rot, Department
of Agriculture and Food Farmnote 245,
WA.
Kessel, D 2008, Annual Ryegrass
Toxicity (ARGT) - Control Through
Management Of Annual Ryegrass
Pasture, Department of Agriculture
and Food Farmnote 258, WA.
Levot, G 2009, Sheep Blowflies, NSW
DPI Primefact 485, NSW.
Love, S 2008, Hydatids – The Basics,
NSW DPI Primefact 812, NSW.
Love, S 2008, Lungworms in Cattle,
Sheep and Goats, NSW DPI Primefact
811, NSW.
Love, S 2008, Sheep Measles – Another
Profit Killer, NSW DPI Primefact 55,
NSW.
Love, S 2011, Drench Resistance
and Sheep Worm Control, NSW DPI
Primefact 478, NSW.
Love, S & Hutchinson, G 2007,
Wormtest For Livestock and Guide To
Egg Counts, NSW DPI Primefact 480,
NSW.
The information in this publication has been collected from:
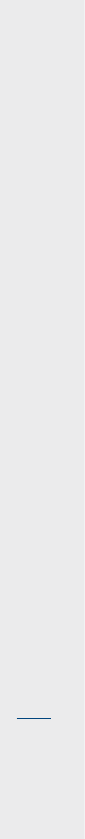
Sheep Diseases | The Farmers’ Guide | 4th edition | November 2022
70
Maxwell, D 2001, Livestock Health –
Cheesy Gland in Sheep and Goats, DPI
&F QLD Primenote SW0047, QLD.
N Maxwell, D 2003, Livestock Health –
Scabby Mouth in Sheep, DPI &F QLD
Primenote SW0056, QLD.
Moir, D 2005, Sheep Arthritis,
Department of Agriculture and Food
Farmnote 24, WA. Newman, R 2007,
Livestock Health – Tetanus in Sheep
and Goats, DPI &F QLD Primenote
SW0088, QLD.
Norris, R 2005, Scabby Mouth,
Department of Agriculture and Food
Farmnote 17, WA.
O’Dempsey, N & Knights, G 2003,
Livestock Health – Lumpy Wool in
Sheep, DPI &F QLD Primenote SW0052,
QLD.
Ollerenshaw, N & Knights, G 2005,
Livestock Health – Suppurative Arthritis
in Sheep, DPI &F QLD Primenote
SW0086, QLD.
Paton, M 2005, Cheesy Gland in Sheep
and Goats, Department of Agriculture
and Food Farmnote 46, WA.
Plant, JW 2004, Sheep Health –
Scabby Mouth, NSW Agriculture Agfact
A3.9.41, NSW.
Plant, JW & Seaman, J 2007, Ovine
Brucellosis, NSW DPI Primefact 472,
NSW.
Richards, J, Atkins, K, Junk, G & Casey,
A 2009, Breeding Merinos For Less
Breech Strike, NSW DPI Primefact 918,
NSW.
Robson, S 2007, Bacterial Arthritis in
Lambs, NSW DPI Primefact 463, NSW.
Robson, S 2007, Photosensitisation in
Stock, NSW DPI Primefact 449, NSW.
Seaman, J & Evers, M 2006, Footrot in
Sheep and Goats, NSW DPI Primefact
265, NSW.
Walker, B 1996, Cheesy Gland Caseous
Lymphadenitis in Sheep, NSW DPI
Agfact A3.9.21, NSW.
Walker, B 2000, How Vaccination
Works, NSW Agriculture
AgnoteDAI/190, NSW.
Walker, B 2005, Vaccination Programs for
Sheep, NSW DPI Agfact A3.9.47, NSW.
Walker, B 2006, Grain Poisoning of
Cattle and Sheep, NSW DPI Primefact
330, NSW.Waller, R 2010, Lamb
Feedlotting Tips, Compass Feeds Tech-
notes & Tips, SA.
Wilson, K, Armstrong, B & Knights, G
2005, Livestock Health – Management
of Blowflies, DPI &F QLD Primenote
SW0101, QLD.
Wilson, K, Armstrong, B & Knights, G
2005, Livestock Health – Management
of Body Lice, DPI &F QLD Primenote
SW0102, QLD.
White, C, Gartrell, J & Beetson, B 2004,
Copper Deficiency in Sheep and Cattle,
Department of Agriculture and Food
Farmnote 28, WA.
Unless stated otherwise, photos
have been sourced from PIRSA
Biosecurity Animal Health staff
and NSW DPI Primefacts.
Notes
Notes
Useful contacts and online resources
Emergency Animal
Disease Hotline
1800 675 888
PIC Registration Office (SA)
1800 654 688 or 08 8207 7919
LPA NVD Helpline
1800 6 83 111
NLIS Database Helpdesk
(National)
1800 654 743
NLIS Hotline (SA)
1800 654 688
RSPCA SA (Welfare)
1300 477 722
Livestock SA
08 8297 2299
Local PIRSA Animal
Health Offices
Glenside 08 8207 7900
Clare 08 8842 6222
Mt Gambier 08 8735 1300
Kingscote 08 8553 4949
Pt Augusta 08 8648 5160
Murray Bridge 08 8539 2110
Nuriootpa 08 8568 6400
Pt Lincoln 08 8688 3400
Struan 08 8762 9100
One Biosecurity
www.onebiosecurity.pir.sa.gov.au
Biosecurity SA
www.pir.sa.gov.au/animal-health
ParaBoss
(WormBoss, LiceBoss, FlyBoss)
www.paraboss.com.au
‘Is It Fit to Load’ Guide
www.mla.com.au/isitfittoload
SheepConnect SA
www.sheepconnectsa.com.au
Livestock SA
www.livestocksa.org.au
Local Veterinary Clinic
Name/clinic:
Contact number:

