
Steps toward a
healthier future:
Bariatric Surgery
Program Guide
Please bring this notebook to:
• Provider Seminar Class
• Psych Assessment
• Pre-Consult with Surgeon
• Pre-Op Consult with Dietitian
• Day of Surgery
• Post Op Appointments
DEPARTMENT OF GENERAL SURGERY
kp.org/wa
Updated April 2020
DA1940000-01-20
Table of Contents
1. Welcome & Overview ................................ 2
Care Team Contact Information ...............
5
Map & driving directions ............................ 6
2. Pre-op checklist ....................................... 10
Provider Seminar ..................................... 11
Weight loss requirement .......................... 12
Nutrition counseling requirement ............. 13
Support group .......................................... 13
3. Metabolic & bariatric surgery ................... 14
4. Pre-paring for surgery .............................. 24
Time-off for recovery ...............................
24
Birth control .............................................. 27
Smoking: ..................................................
27
Sleep apnea .............................................
28
kp.org/wa ................................................ 29
Hotels ...................................................... 30
5. Pre-op instructions ...................................
32
day of surgery ..........................................
35
hospital stay ............................................. 36
6. Nutrition plan ............................................ 44
Laying the foundations ............................ 45
Pre-op diet ............................................... 64
Day before surgery diet ........................... 70
Post-op diets: stages 1-5 .................... 71-99
Protein 101 ............................................ 100
Frequently asked questions ................... 118
7. Vitamins, supplements
& medications ............................
124
Probiotics ................................................. 134
Recommended supplement brands ........ 135
8. Post-op concerns .................................... 136
Hydration / dehydration ........................... 137
Nausea / vomiting .................................... 138
Constipation ............................................ 139
Dumping syndrome: ................................ 140
When/who to call ..................................... 141
9. Follow-up appointments .......................... 142
10. Keys to success ...................................... 144
Food journaling ........................................ 145
Newsletter & web page ........................... 146
Emotions.................................................. 148
Sleep apnea / post op ............................. 149
Hair loss................................................... 150
Excess skin ............................................. 151
11. Resources you find helpful ...................... 152
12. Poem ....................................................... 154
13. Glossary of terms .................................... 156
14. Document your measurements ............... 160
15. Free space for documents you’d like to add
to your notebook
1

2
We are pleased to welcome you into
our Bariatric Surgery Program.
Please be advised that your approval is for the program. You will need to have your bariatric benefit
at the time of surgery, which will be verified once your surgery is scheduled. Please notify us if you
have a change in your benefits. Do not be concerned about the expiration date on your authorization
letter. Your surgery does not need to be completed by that date.
We would like to introduce you to the overall process of this care and the team of health care
providers who will be working with you throughout your experience. You are an important part of the
team and will be actively involved in your care as you participate in this program. Adequate
preparation and planning before surgery and your active involvement after surgery will help you
accomplish the best possible results.
This notebook is your program information guide. It describes the steps leading up to surgery, what
to expect during your hospital stay and recovery, and how to maintain long term benefits from the
procedure. Please keep this notebook! You will find the answers to many of your questions, both
before and after your surgery.
We are committed to helping you throughout this life-changing and sometimes challenging
experience. Working together, we expect a difference in your long-term health. Keep this worthy
goal in mind to help cope with any frustrations you may encounter along the way.
In order to continue to improve the care we provide, we ask for your feedback and suggestions.
Did you know? Our bariatric surgery program helped earn Overlake
Hospital a coveted HealthGrades 2018 Bariatric Surgery Excellence Award
– and status in the top 5% for bariatric surgery excellence nationally.
3
Keep Up the Momentum
Once you get your notebook, read through it – and begin your journey toward
weight loss and improved health.
The medical testing and consults necessary will be ordered for you. Please keep in mind that if any
follow-up is recommended as a result of any testing or consults, that must also be completed. This
might include a sleep study or treatment / therapy for depression or eating disorder assessment and
possible treatment. When further Gastroenterology testing is required, that also extends your time in the
program.
It may seem like a long and possibly intimidating to-do list and you can expect the medical testing and
pre-op work-up process to take possibly 4-6 months to complete. You may also have the ability to
complete the process in less time. This depends largely on your motivation and continued momentum
through the steps.
If you are delayed to treat depression, an eating disorder or other issue, please follow through with the
recommendations. We know that this can be upsetting, to be delayed, however following through on the
recommendations will only serve to benefit you. Untreated or under-treated depression and eating
disorders can result is problems following surgery – sometimes significant problems that could result in
hospitalization and in rare incidence another surgery.
Our goal is to make sure you are ready and thoroughly prepared for your surgery. Being proactive and
motivated can make the process move along a bit faster and smoother.
Our growing team of bariatric professionals are here to assist all along your journey, from today and for
many years to come!
4
Welcome to the Kaiser Bariatric Surgery Program
We enjoy this field of surgery as we get to cure more disease than any other field of Medicine or
Surgery. With one operation, we achieve resolution or remission of type 2 Diabetes, hypertension, high
cholesterol, sleep apnea, morbid obesity, and urinary incontinence (females) in greater than 90% of
patients. For less than the average-annual cost of insulin for a given patient, we induce a remission of
the diabetes in 90% or more of patients (96% in the Kaiser Permanente (formerly Group Health) gastric
bypass data base).
The Four Pillars of any successful Bariatric Surgery Program are the Surgical, Medical, Behavioral, and
Nutritional components. Our Bariatric Program is expanding to include pre-operative and post-operative
help from each of these components.
Our Bariatric Program was started in 1994.
Dr. Anirban Gupta joined Kaiser Permanente (formerly Group Health) in 2016, transitioning his
practice from Ohio where he developed a MBSAQIP-Accredited bariatric program from the ground up.
He completed a Laparoscopic and Endoscopic Fellowship in Bariatric Surgery at Johns Hopkins in
2008 and completed his General Surgery training in University of Toronto in 2007.
Dr. M. Imad Haque joined Kaiser Permanente in 2020, transitioning his practice after a 21 year career
as an Army General, Trauma and Bariatric Surgeon at Madigan Army Medical Center. He completed a
Fellowship in Advanced Laparoscopy (Bariatrics), Endoscopy, and Ultrasound Fellowship at St.
Vincent Hospital Medical Center and Indiana University Medical Center in 2008. He completed his
General Surgery residency at Madigan Army Medical in 2003. He established the first multidisciplinary
bariatric surgery program for the Department of Defense in Europe in 2004. Dr. Haque retired as a
Colonel in the Army. He has multiple deployments to Syria, Iraq, and Afghanistan. He is passionate
about surgical process improvement and brings advanced Robotic Surgery (DaVinci) experience to the
program.
Dr Shireesh Saurabh joined Kaiser Permanente in 2019. He is a board certified general and bariatric
surgeon. He was in a practice in Iowa for 5 years, where he established an accredited bariatric surgery
program. He completed his general surgery training at Drexel University in 2013 and bariatric surgery
fellowship at University of Iowa in 2014.
We look forward to continuing our tradition of Bariatric excellence, with you as our partners!
5
Care Team
Your care takes place in different settings and is coordinated by the Bariatric Surgery Program team, to
make sure you have a successful and safe procedure. The team will provide you with information to
make sure you are ready for surgery and assist with your recovery afterwards. Each team member has
a special role and responsibility.
Kaiser Permanente Bellevue Medical Center
Our Bariatric Clinic is a part of the General Surgery Clinic
Hours: 8:00 am to 5:00 pm, Monday through Friday
Phone: 425-502-3454 Toll-free: 1-800-995-5658, extension 3454
Bariatric Surgeons: A general surgeon with specialized training in bariatric surgery.
Dr. Anirban Gupta
Dr. Shireesh Saurabh
Dr. Imad Haque
Bariatric RN Case Manager: A Registered Nurse (RN) manages the pre-op process/medical work up
and post op triage for problems / concerns. Phone: 425-502-3454
Bariatric Dietitian: Dietitian with specialized training and experience to provide dietary evaluation,
education, and counseling. Phone: 425-502-3454
Lisa Stariha
Fionna Marave
Bariatric Psychologist: Our bariatric psychologist specifically works with you to find successful ways to
meet your healthy lifestyle goals.
Dr. Janet Ng
Bariatric Physician Assistants (PA) and Nurse Practitioner (ARNP): with special education and
experience with bariatric surgery and bariatric follow up care.
Medical Assistant (MA): will assist in scheduling of appointments and coordination of care
6

7
Bellevue Medical Center
11511 N.E. 10th St.
Bellevue, WA 98004
425-502-3000
Note: Traffic can be difficult at any
time of day, coming from any
direction.
Please allow enough travel time
From Interstate 405 southbound
Take Exit 13B for N.E. 8th Street
East/West.
Turn right onto westbound N.E.
8th Street.
Turn right onto 112th Avenue N.E.
Turn right onto N.E. 10th Street,
driving over I-405.
Turn right into the medical center.
From Interstate 405 northbound
Take Exit 13A for N.E. 4th Street.
Turn right onto N.E. 4th Street.
Turn left onto 116th Avenue N.E.
Turn left onto N.E. 10th Street.
Turn left into the medical center.
*** Note: Parking fee runs from $3.00 - $7.00 **********
8
9
Entering the Bariatric Surgery Program
Medical research has shown that Bariatric Surgery is a safe and effective way to lose weight and
improve health for a specific group of patients. Our Bariatric Surgery Program is structured to help those
people reach their health goals. To help you get started and to know what to expect, the steps of the
programs are listed below.
Primary Care patient identification:
You and your primary care physician decide that you may benefit from this surgery. Your doctor submits
a Bariatric Referral to the Bellevue Bariatric Surgery Department, for review.
Medical record and coverage review by Clinical Review Unit:
Your medical history and individual insurance coverage are reviewed based on the criteria established
by your health plan.
Welcome and Introduction to Bariatric Surgery Program:
You will receive your Bariatric Notebook, Step’s toward a Healthier Future, at your first office visit. You
can also find the digital binder on the bariatric website, or we can send you a link via your kp.org email.
Bariatric Surgery Process:
If we don’t answer all of your questions after the Provider Seminar, or you think of more questions,
please jot them down for your next visit. At your first consult visit we will identify your needs and order
your labs and other tests. You may be sent to other specialists for pre-op work up.
Evaluation by other medical specialists as needed:
All consultations/assessments requested by our pre-op, Nurse Practitioner and/or your primary care
provider must be completed, as well as any follow up that might be recommended as a result of those
tests/consults/assessment. For example, the sleep medicine provider may recommend a sleep study.
You must follow through with that as well as any recommendations made based on the results of the
sleep study.
This further evaluation helps to make sure you are medically ready for surgery. We will not be
scheduling a consult with the surgeon until the medical work up has been completed.
10
Preparing for Bariatric Surgery
Once you receive your notebook, please read it through carefully. Failing to review all information may
result in missing important information and delaying your progress.
Provider seminar attendance is mandatory
Unsure?
If you are ambivalent or on the fence at all about moving forward with surgery, we absolutely
recommend that you attend this class before deciding not to proceed. This will allow you to make the
most educated decision, with information from the surgeon and dietitian.
Contacting the Bariatric Clinic
If your call is answered by the call center, please leave a message. Calls are returned based on priority,
with post op patients being called back first. You can be assured if you are calling prior to your surgery;
you will receive a call back, typically the same day. Please be patient! If you are calling after your
surgery, your call will be returned within an hour or two of your message. Post-op patients can also call
the General Surgery nurse at 425-502-3450 for more immediate assistance.
kp.org/wa email is an excellent way to communicate. If you do not have this option, please see section
4 for more information about it and how to sign up.

11
Pre-Op Checklist - Steps to complete before surgery
Please do not hesitate to call our office with any questions or concerns about completing this checklist.
Call: 425-502-3454 or e-mail through kp.org/wa or the Kaiser Permanente Washington mobile app (reply to
Bariatric RN email)
Step
What to expect
Date / Time
Complete?
Provider
Seminar
See details on next page.
Initial Visit & Nutrition Class
Develop individualized care plan
Psychology Visit Schedule visit after attending the Provider
Seminar. (Must attend prior to assessment)
Questionnaires Complete questionnaires and bring with you
to your first office visit.
Pre
-
op Visit & Class
Appointments Labs .................................................................. ____________ .........
Chest X-ray ....................................................... ____________ .........
EKG .................................................................. ____________ .........
Sleep Consult ................................................... ____________ .........
Pulmonary Consult .......................................... ____________ .........
Other: ............................................................... ____________ .........
Other: ............................................................... ____________ .........
Call or e-mail Pre-Op Nurse when all of the above have been completed
Phone: 425-502-3454 E-mail (reply to previous email) using kp.org/wa or the Kaiser Permanente Washington
mobile app
Pre-op Visit & Class
Meet in the morning with your surgeon to
develop a plan for surgery. In the afternoon,
attend a small group class to prepare you for
safe surgery and after-surgery care.
Date /
Time:
In addition to the above requirements, all patients must lose weight prior to surgery
The required amount of weight loss depends on your weight / BMI at the time of your referral into the program.
Patients with BMI’s higher than 60 may have a required weight loss goal prior to surgery. This is determined on an
individual basis.
**See Section 6 for suggestions to get you started in meeting this goal now**
My weight loss goal is:
_______________
My weight at Pre-op is:
_____________
My weight after surgery is:
____________

12
Provider Seminar
This 90-minute class will include presentations from one of our surgeons and provides valuable
information to help you prepare for your surgery, hospital stay, as well as address mental health and the
importance of developing diet and exercise routines.
Please feel free to have your support person view the presentation with you. The information presented
will help your support person to better support you in this journey. Class attendance is a requirement
prior to being scheduled for your consults.
Where: This seminar will be presented as an online education class
When: 8:30 a.m. to 10 a.m.
If you cannot attend on the day you are scheduled for, please reschedule.
Pre-Op Consults
It takes an average of 4-6 months to get through the program. The preop consult is your last step before
being scheduled for surgery.
Once you have met your goals and completed your testing and recommended therapies, our office will
call you to schedule the consults with the surgeon and dietitian. After being scheduled for surgery, you
will need to be sure to get your preop physical exam, labs and EKG within 30 days of your surgery date.
If you are unable to make your scheduled appointment, please notify the bariatric clinic in
advance, so that the appointment can be rescheduled: 425-502-3454.
13
Weight Loss Requirement
Reason:
The weight loss requirement helps to make your surgery safer and more likely to be laparoscopic, as
losing weight shrinks the liver. The liver lies over a portion of the stomach that the surgeon will be
working on. The term fatty liver refers to fat accumulation in the liver. If the liver is too large and can’t
safely be moved out of the way, your surgery may need to be converted to an open procedure, which
certainly results in more post-surgical pain and requires additional healing time. Losing just 5% of your
total body weight will result in a decrease of fat in the liver.
Making healthy eating and life style changes prior to surgery also shows acknowledgement that this is
not a quick fix and will require that you make changes for sustained results and it shows compliance with
the recommended changes prior to surgery.
How to make this happen:
There is no particular diet or plan outlined to accomplish the pre-op weight loss. Reading through the
diet guidelines in section 6 will help you to begin to make some changes in advance of surgery. Most
often making these changes will result in weight loss.
A good place to start might be downsizing meals, eliminating refined carbohydrates, such as bread,
pasta, cookies, crackers and pastries. These are changes that will be required after surgery. Making
small changes, one at a time helps to develop new habits. This is a good time to begin to make those
small changes, as they will help in reaching the 5% weight loss goal.
Beginning to add exercise to your daily routine will also assist in meeting this goal. Try adding short
walks to your daily routine, which burns calories. Add additional exercise as tolerated. Every little bit will
help in establishing new habits and burning calories.
What does the weight goal mean for you?
At your first video visit with the Surgeon, we will discuss your weight loss goal. We begin watching your
progress by using your weight at the time of your referral into the bariatric program. We want to see a
general downward trend. If you are working on your healthy habits you will see this happen.
Requirement:
During the last 2 weeks before your scheduled surgery, you will be asked to follow a Liver Shrinking Diet
Patients with a BMI of over 50 may be asked to stay on this Liver Shrinking Diet a little longer. The RN’s
and dietitians will work with you in your phone visits as you reach your weight loss goal.

14
Nutrition Counseling
Nutrition counseling is mandatory before and after surgery.
Nutrition Counseling:
o Initial visit
o Scheduled goal setting phone visits
o Pre-op consult
o Post op: coordinated with post op appointment (7-10 days post op)
o 2 month follow up: coordinated with 2 month clinic follow
o 6 month follow up: coordinated with 6 month clinic follow
o Ongoing access through phone and email communication (pre and post op)
Nutrition section of this notebook (section 6) will provide recommendations for pre-op diet and lifestyle
changes that will assist you in meeting your weight goal as well as help to begin to make changes in
preparation for life after surgery.
Making changes prior to surgery will help to make surgery safer and life after surgery that much easier.
You will find guidelines for each stage of the post op diet. The guidelines are meant to assist you in
making healthy / appropriate food choices along the way.
Call or email Bariatric Dietitian with any questions that you may have about the nutrition requirement.
Bariatric Support Group
Please see information about upcoming support groups on our web page:
http://www.kp.org/bariatric-patients/
15
Undergoing Bariatric Surgery
What is Bariatric Surgery?
There are several different surgical procedures which are classified as Bariatric Surgery.
The three surgeries that are performed at Kaiser are Gastric Bypass (Roux-en-Y) and Laparoscopic
Adjustable Gastric Band (Lap Band) and Laparoscopic Sleeve Gastrectomy. One or more of these
operations may not be covered depending upon your bariatric coverage.
Roux-en-Y Gastric Bypass Surgery (RNY)
The Gastric Bypass procedure has passed through several evolutions and modifications before it
reached its present state but the operation has been around for more than 30 years and the long
term results are well established. This operation bypasses about 97% of the stomach and creates a
tiny pouch at the top of the stomach, about one ounce in size. The pouch is created by dividing a
small portion of the upper stomach completely from the rest of the stomach, with a stapling/cutting
device. The food passageway is re-established by connecting the upper small intestine, or jejunum,
to the small pouch with a 10 – 12mm (1/3”) anastomosis, or connection. In time, this one ounce
pouch becomes more pliable and efficient, allowing one to eat larger, but still smaller quantities of
food. Over time, usually one to two years, weight loss will stop. The Gastric Bypass Procedure is
the most commonly performed bariatric procedure done in the United States.
The surgery can be performed via open procedure or by a laparoscopic procedure approach but
most procedures are done by the laparoscopic approach. If the surgery is done by an open
procedure, the incision extends from the breast done to the navel. If the surgery is done by the
laparoscopic procedure, there are 5-6 small incisions. During the operation, the abdomen is filled
with carbon dioxide air and a camera is inserted through one of the openings. The operation is done
while watching a high definition picture on a monitor. Occasionally a laparoscopic surgery needs to
be converted to an open procedure. The procedure appropriate for you will be determined by the
surgeon and discussed with you. See the diagram for the illustration of the anatomy following Roux-
en-Y Gastric Bypass Surgery.
How is food digested after surgery? When food is swallowed it enters the small upper pouch
of the stomach. This part of the stomach holds only about one ounce of liquid or 2-3 small bites of
food, at one time. From the upper pouch the food passes through a very small opening (about 1/3”
diameter) into the upper small intestine or jejunum, where nutrients are absorbed. Before surgery,
the stomach ground the food into digestible portions. The new small pouch stomach does not do
this. For the first month after surgery, food must be pureed or blenderized. Thereafter, thoroughly
chewing food before swallowing allows easy passage into the small intestine. The digestive
enzymes produced by the lower stomach, pancreas, and the liver empty 40-60 inches from the
stomach pouch-intestine connections. By making the connection close to the stomach, the majority
of the small intestine absorbs very well (only about 1/5 of the small intestine does not have bile and
pancreatic enzymes mixed immediately with the food). This helps to avoid the unpleasant side effect
of malabsorption.
16
How does Gastric Bypass Surgery help you lose weight?
This surgical procedure works by creating satiety or the feeling of being full and comfortably
satisfied. When the stomach walls are stretched by food, a message is sent to the brain,
giving a signal of appetite satisfaction. After gastric bypass surgery, a small meal in the
pouch creates the same feeling as if you had filled the whole stomach with a very larger
feast-type meal. This surgery changes the way the appetite center in the brain works. Your
brain tells you to eat smaller, healthier amounts of food.
The small size of the pouch also prevents you from eating too much at any one time. One
small bite beyond satisfaction of hunger will create a stuffed feeling; another small bite will
cause nausea; any additional food will cause pain and vomiting.
The duration of the feeling of satisfaction when eating small amounts depends not only on the
amount of food in the stomach, but also the length of time that the stomach remains filled. If
you drink liquids with meals, or within 60 minutes after eating, the thoroughly chewed food is
washed through the pouch, causing rapid emptying, resulting in the sensation of hunger
returning sooner, long before the next mealtime.
The goal for successful weight loss is to fill the small pouch with foods that are nutritious,
bulky in volume, and do not empty from the stomach pouch too rapidly. This kind of meal is
not difficult to achieve and we will assist you in making these appropriate food choices. High
calorie liquids, which readily pass through the small connection, scarred ring of the stomach
outlet are absorbed in the bowel and cause weight loss to be slowed or even stopped. For
this reason, high calorie liquids must be avoided.
The gastric bypass has an effect on a hormone produced in the intestine called Ghrelin which
controls appetite in the brain. After gastric bypass the amount of Ghrelin produced in the
stomach and small intestine is greatly reduced and this results in a marked decrease in
appetite.
The third major effect, that occur after gastric bypass that helps in weight loss is a condition
called dumping. In the normal stomach foods that have a high fat or sugar content are
diluted and processed by the stomach. There is a valve at the end of the stomach that
releases this processed food into the small intestine were digestion occurs. With gastric
bypass this function of the stomach is bypassed so that if these foods are eaten in any
significant amount if causes dumping. When foods that are high is sugar or fats like juice,
milk shake, ice cream, cake go directly into the small intestine after gastric bypass, fluid is
pulled into the intestine and patients feel weak, sweaty, have a rapid heart rate and can get
diarrhea. These effects remind patients that these foods should not be eaten. The amount of
dumping patient experience can be quite different, so the best option is to avoid these types
of foods.
What are the results of Roux-en-Y Gastric Bypass Surgery?
Success of the surgery is measured by achieving improved health and not specifically upon
amount of weight lost. Conditions such as diabetes, sleep apnea, hypertension, reflux and
arthritis are expected to improve as weight is lost. This surgery, along with change in eating
habits and exercise, has shown to be an effective method for losing and maintaining weight
loss in the majority of patients. Gastric bypass has a dramatic, rapid effect on type II
diabetes. In patients who have been diabetic for less than 10 years we often will have them
off of their oral medications and/or insulin before they leave the hospital. Even with diabetes
of greater than 10 years duration we will see dramatic reductions in the amounts of insulin
that are needed for excellent diabetes control.

17
What weight loss should I expect?
Results of the Kaiser Permanente Foundation Health Plan of Washington (formerly Group
Health) Bariatric Surgery Program shows an average of approximately 75% of excess body
weight loss and approximately 38% of total body weight loss at 18–24 months after gastric
bypass and maintenance of 67% excess weight loss at 5– 10 years after surgery. Rapid
weight loss usually occurs in the first six months after surgery, with more gradual loss
continuing for another 6 to 12 months. Weight loss plateaus should be expected. Weight
regain after 2 years can occur. This can range from no weight gain to regaining all of the lost
weight (this is rare). If appropriate lifelong habits are developed in the first 2 years after
surgery weight regain can be minimal. If old bad habits return, some weight gain will occur.
Working closely with your Bariatric Nutritionist after surgery and your bariatric team beyond
the first year after surgery will help continue progress toward your goals.
Remember, in addition to the surgery, your
food and exercise habits are essential lifelong
behavior changes necessary for successful
weight loss and maintenance.
This program gives you the tools to improve
your health. We will encourage you to do so.

18
RNY Gastric Bypass
19
Laparoscopic Sleeve Gastrectomy (LSG)
Laparoscopic sleeve gastrectomy was originally performed as a first-stage bariatric operation for high
risk patient who were to undergo a second stage gastric bypass or duodenal switch. Over the past 5-6
years it has been shown to be an effective primary bariatric operation, but longer term results are not yet
available.
Using surgical staplers the operation permanently removes a significant portion of the upper stomach
creating a long, tubular stomach along the lesser curve of the stomach. This portion of the stomach has
a lesser ability to stretch than the portion of the stomach removed. Unlike the gastric bypass there is no
rearrangement of the small intestine and food flows in the same direction as it did prior to the operation.
How does LSG help you lose weight?
The procedure has a number of effects that result in weight loss. With the removal of approximately 3/4
of the stomach, the sleeve gastrectomy causes restriction so patients are more quickly satisfied when
they eat. Like gastric bypass, sleeve gastrectomy reduces the production of the intestinal hormone
Ghrelin that decreases appetite.
What are the results of LSG Surgery?
The small stomach created after sleeve gastrectomy empties more quickly and may be responsible for
improvements in diabetes after the surgery. Initial results have shown that the effect on diabetes is
significant with effects that are close to what is seen with gastric bypass and superior to what is seen
with the Lap Band. With significant weight loss, improvement in other co-morbidities such as sleep
apnea, hypertension and arthritis are seen as well. Reflux symptoms can worsen after LSG.
What weight loss should I expect?
Results from the published medical literature show that approximate excess body weight loss at 3 years
is 66-68% and at 6 years is 53%. The number of patient followed for 6 years is small and longer term
results are not yet available at the time.
As with gastric bypass: Remember, in addition to the surgery, your food
and exercise habits are essential lifelong behavior changes necessary for
successful weight loss and maintenance.
This program gives you the tools to improve your health. We will
encourage you to do so.

20
Laparoscopic Sleeve Gastrectomy

21
Duodenal Switch and Other Malabsorptive Procedures
There are a group of bariatric operations that cause a malabsorption of proteins, fats and vitamins that
contribute to a patients’ weight loss. Because of the severe nutritional problems that can occur with
these operations they are done less frequently in the United States. Currently less than 5% of all
bariatric operations done in the US are of these types. The operations include duodenal switch,
biliopancreatic diversion, and distal gastric bypass.
In the duodenal switch operation the stomach size is reduced as it is for the sleeve gastrectomy but to a
lesser degree (remaining stomach is larger). In addition there is a change in the intestinal connections
that causes malabsorption of the nutrients mentioned above.
With the gastric bypass the digestive enzymes produced by the lower stomach, pancreas, and the liver
empty 40-60 inches from the stomach pouch-intestine connections. By making the connection close to
the stomach, the majority of the small intestine remains functional. In the duodenal switch the segment
of intestine where food and enzymes mix is 100 cm or 25 inches long, this results in decreased
absorption of fats and protein that help in weight loss but can also result in malnutrition.
With the increased risks associated with these operations, we do not recommend or perform
them at Kaiser Permanente.
Duodenal Switch

22
What are the risks of Bariatric Surgery?
All surgical procedures have some risk. Medical complications such as diabetes, cardiac or pulmonary disease, which
effect morbidly obese persons, can increase the risk of surgery. Pre-operative evaluation is undertaken to reduce
unnecessary risk. Being aware of the following risks allows you to make an informed decision about surgery.
National statistics have shown a 0.5 to 4% death rate related to immediate post- operative complications
following bariatric surgery. Mortality rates at Kaiser Permanente in Washington (formerly Group Health) has
been less than 0.75%.
Blood clots or Deep Vein Thrombosis (DVT)
DVT’s can occur with any major surgery. Blood flow through the legs can be slowed and a clot may form.
Pieces of the clot can move from the leg to the lungs and form an embolism. This can be life threatening.
Obesity and abdominal surgery increase the risk of this complication. Preventing DVT and embolism after
surgery is an important part of your recovery. Getting out of bed and walking, taking anticoagulation
medications, and using leg compression devices while in bed are some of the treatments used to avoid this
complication. Your surgeon will make a plan for you to reduce your individual risk of blood clots.
Lung infections or pneumonia
General anesthesia, pain following surgery, and obesity contribute to the risk of developing pneumonia. Use
the incentive spirometer at least every 1 to 2 hours while awake. Getting out of bed and walking after surgery
helps reduce the risk of this complication.
Use pain medication, as needed, to help stay comfortable enough to do these activities frequently. Continue
these suggestions even after you are discharged from the hospital.
Heart problems
Bariatric surgery can cause major stress to your heart. Confirming your heart’s good health before surgery and
close monitoring during hospitalization helps to minimize this complication.
Weakness in the abdominal wall or hernia
With the open procedure, the incision extends from the bottom of the breastbone to the navel. Obesity and a
long incision can lead to a weakening of the abdominal wall, which could allow a hernia to develop. This
complication occurs in approximately 20 to 25% of bariatric patients who have an open procedure. This risk is
reduced when the laparoscopic procedure is used.
Bleeding
Blood less can occur at the time of, or following surgery. Blood replacement or transfusion is not usually
required.
Gallstones
Significant weight loss, as occurs after Roux-en-Y Gastric Bypass and Laparoscopic Sleeve Gastrectomy
surgery, can increase the risk of gallstone formation.
23
Complications that can occur strictly after Roux-en-Y
Gastric Bypass
A leak at the site of the stomach-intestine connection
This usually occurs within the first days following surgery and requires further surgery to correct.
This occurs in approximately 1 to 2% of all Roux-en-Y Gastric Bypass surgeries.
Stricture
This complication occurs when the connection between the new small upper pouch of the
stomach and the jejunum becomes narrowed and food cannot pass effectively. An outpatient
procedure called a balloon dilatation can be performed endoscopically to correct this problem.
Strictures will typically occur about 4-6 weeks after surgery. See illustration of the anatomy
following Roux-en-Y Gastric Bypass surgery.
Marginal ulcers
This is an ulcer that forms in the area of the gastric pouch and jejunum connection. The risk of
this complication is low. It can be caused by use of anti-inflammatory medications such as
ibuprofen (use of these medicines after surgery needs be avoided). Smoking will also result in
the development of ulcers.
Stomach staple line breakdown or fistula
Continuously eating or drinking too much at a time can cause this complication and will create a
new connection between the stomach pouch and the remainder of the stomach. This is a rare
complication.
Dumping syndrome
Sweating, rapid heart rate, and a feeling of weakness, nausea, vomiting and/or diarrhea can
occur if foods high in simple sugars or fat empty into the jejunum undiluted. This is very
unpleasant and reinforces the negative results of inappropriate eating and drinking.
24
Other complications that can occur long term with bariatric
procedures
Nausea / Vomiting
Not chewing adequately, eating too much, or eating too quickly leads to this problem. Also,
eating/drinking inappropriate foods/drinks.
Constipation
Reduced food intake results in less waste products and firmer, smaller stools, which can be more
difficult to pass. Eating fiber foods, drinking water, taking probiotics and activity help to avoid this
problem. Any sugar-free fiber supplements, such as Metamucil may be use (once you are
drinking at least 64 oz. of fluids per day).
Hair loss
Consuming fewer calories in the first few months after surgery can result in some hair loss. This
is not usually a permanent condition and the hair grows back as calorie intake increase. Avoid
chemical treatments of the hair during the first year following surgery. The use of Biotin, a B
vitamin, can be useful.
Intestinal obstruction
A blockage can form with the new anatomy following this surgery. Frequent vomiting
unexplained by over eating, can be a symptom of this problem.
Informed Consent
The surgeon will review the above risks with you at your consult appointment. Ask questions about
anything you do not understand. You will be asked to sign an informed consent stating that you clearly
understand your treatment. Be sure to read the consent form before you sign it.
Receiving Anesthesia
Problems from anesthesia are rare. Your risks will be discussed with you during your interview
with the anesthesia provider on the day of your surgery. Be sure you ask any questions and
resolve any concerns you might have at that time.
Your anesthesia provider watches you the entire time that you are in the operating room (OR).
Your blood pressure, heart rate and rhythm, and oxygen saturation are carefully observed and
monitored throughout the surgery.
25
Before your surgery (Preparing for surgery)
Arrange for help after surgery
Your hospital stay is expected to be 1-2 nights in the hospital. 90% of patients will go home on
the afternoon or evening of day 2 after surgery. For instance, if your surgery is Monday, you
would expect to go home on Wednesday afternoon.
Open Roux-en-Y (RNY), your hospital stay is expected to be 3-4 nights in the hospital.
On the day of discharge, you will need someone to drive you home.
During the first 1 to 2 weeks you may need assistance with activities such as:
o Transportation
o Grocery shopping
o Meal preparation
o Care of your home
o Care of your children and/or pets
If you do not have someone who can provide this assistance, talk with the social worker from
your primary care clinic. They may be able to recommend resources.
Time-Off Work for Recovery
It is recommended that you take 2-4 weeks off work for recovery, regardless of which procedure you are
having. This allows for time to recovery from your surgery physically, adjust to new eating patterns,
begin exercising and basically spend some time taking care of yourself. This is going to be a time of
adjustment and it’s in your best interest to take the time to heal and recover without the stress of work to
worry about.
We are happy to complete FMLA forms, other time off request forms or write letters for time off and return to
work requests; however it saves time and energy if we know what you are asking for in advance. Please
complete the FMLA Prep-Sheet and release of information, found in the back pocket of your notebook, and
fax these along with your FMLA forms to 425-502-3570. If there are questions about time requests, please
call or email the bariatric clinic, 425-502-3454.
26
Get ready for eating differently
Remove inappropriate food types from your home and go shopping prior to your surgery, for
foods to be used after surgery.
Practice new eating behaviors before your surgery. Eating slowly and chewing your food well,
reducing portion sizes, and stopping when you first feel full are the only ways you will be able to
eat without causing problems following surgery.
Keep a record of the foods/fluids that you eat/drink each day. This will be expected following
surgery, start this habit before surgery. See section 10 for food journaling recommendations.
Get a set of measuring cups and spoons, a food or postal scale, smaller plates and utensils to
assist in tracking food portions.
Your diet will begin as clear liquids in the hospital, full liquids once you are home, soft/puree diet
at about 2-3 weeks post op. You will need a blender or food processor to prepare the proper
consistency.
**** Important ****
Many patients with morbid obesity may have one or more eating disorders which, if not addressed
appropriately can complicate their post-operative safety and success. It is important to think about how
you use food as a way of dealing with stress, anxiety, depression, boredom, or in any way as a coping
mechanism. It is then very important that you identify and use other ways of coping, such as exercise or
support groups.
During the pre-op psych-social assessment, eating disorders or eating behaviors may be revealed and
may require further intervention. It will be a requirement to follow through with any recommendations
made.
Loss weight prior to surgery
Weight loss before surgery shrinks the liver which makes the surgery safer and lowers the
chance of needing to convert to an open operation. It also gets you prepared to be an active
participant in your weight loss success.
Please see the weight loss requirement (see section 2).
27
Prepare Advance Directives
If you are unable to make decisions, your doctor will talk with your family members or significant
others or refer to written instructions you have prepared, to try to find out what treatment you
would want or would be in your best interest.
It is recommended that you complete your advance directives prior to any surgical procedure. A
copy of the Consumer Guide to Advance Directives has been included with this booklet.
Update any Advance Directives you may already have prepared.
If you are unsure if you already have your Advance Directive documents on file, contact the
Kaiser Permanente Registry at 206-326-3290.
Your primary care clinic Social Worker can answer any questions about preparing Advance
Directives.
Completed advance directives can be taken to the business office of your primary care clinic to
be scanned into your electronic medical record.
NSAID Use
The use of aspirin, ibuprofen, naproxen, or other Non-Steroidal Anti-Inflammatory Drugs
(NSAID’s) will greatly increase your risk of stomach ulcers after bariatric surgery (much more so
with the RNY)
If you currently take any of these products routinely, please talk with your primary doctor or
prescribing doctor (if they are recommended by a doctor), about an alternative that you can take
after your surgery.
28
Birth Control
Prior to surgery
If you are a woman of child bearing years, you will need to be on some form of reliable birth
control before and after surgery.
Birth control pills must be stopped at least 30 days prior to surgery and are not a reliable source
of birth control following surgery, do to hormonal changes. They also increase the risk of blood
clot during the operative and immediate post-operative period, which can be very serious. We
want to do everything possible to avoid blood clots.
If you are interested in the placement of an IUD, please see your OB/GYN to discuss prior to
your surgery.
After surgery
Pregnancy is not recommended for at least 18-24 months following bariatric surgery.
If you were infertile or had trouble conceiving prior to surgery, this may change quickly following
surgery, with even minimal weight loss.
Smoking
If you smoke, stop
There is a nearly 100% ulcer-formation rate in those smoking or with tobacco exposure after
surgery. These ulcers can result in perforation, stricture, bleeding or, all of the above.
Surgery will not be performed on anyone who currently smokes. You must be completely smoke
free for at least 3 months prior to surgery.
Quit for Life® is a Kaiser program to help anyone trying to stop smoking. If this applies to you,
please ask for more information on how to join the program.
If you resume smoking after surgery, the chances of developing ulcers, bleeding and/or intestinal
perforation increases dramatically.
29
Sleep Apnea
What is obstructive sleep apnea?
• Caused by upper airway collapse during sleep
• While awake: muscles hold upper airway open
• During sleep, airway muscles relax, resulting in airway narrowing
• Mild narrowing snoring
• Moderate narrowing reduced airflow (“hypopnea”)
• Severe collapse absent airflow (“apnea”)
How does obstructive sleep apnea affect your health?
• Consequences of sleep fragmentation
– Unrefreshed sleep
– excessive daytime sleepiness lead to motor vehicle accidents
• Cardiovascular consequences of OSAS
– increased risk of hypertension
– Probable increased risk of heart disease and stroke
• Other consequences of OSAS
– Night time reflux, morning headaches, gout attacks, frequent urination, leg swelling,
impotence
Why it is important to treat obstructive sleep apnea?
1. Treatment of obstructive sleep apnea can improve overnight sleep quality, daytime alertness and
overall functional status. It may improve blood pressure, cholesterol and blood sugar measurements
and it may reduce the risk of heart problems.
2. Automatically adjusting positive airway pressure machines (APAP) stent open your airway to prevent
the collapse allowing you to breathe normally.
3. Since anesthesia and pain medications sedate you that relaxes your airway more so; this in turn can
worsen your sleep apnea. So it is very important to bring your APAP/CPAP or BiPAP to the hospital
to use post-operatively.
Kaiser Permanente Outpatient Sleep Apnea Services contact number is 1-800-348-6382
30
kp.org/wa
kp.org/wa allows you to:
Refill Prescriptions
Make Appointments and Cancel Appointments
View Upcoming Appointments
Review Lab / Radiology Results
Securely email your doctor, ARNP/PA, dietitian and nurse
o You will not be able to initiate an email until you have been seen in the clinic by the
bariatric surgeon. Prior to that time, you can ‘reply’ to RN’s email to you. After your pre-
op appointment, you can email to the ‘office of’ Dr. Landers or Dr. Gupta.
View your Medical Records
Check your Benefits
Create your Health Profile
If you don’t already have an account, here’s how to get started:
Go to kp.org/wa and click “Register now”
Enter your Member ID # (the number on your membership card), your last name, and your birth
date
Click the submit button
You will get a “Thank You” screen where you will get a temporary password.
In a few days, you’ll receive a verification code in the mail. Once you receive it, just log on and enter
code, then you’re ready to access the convenience of kp.org/wa.
The Secure Patient Messaging is a fabulous way to communicate without phone tag. You will receive a
response within 1 working day. Note: This e-mail is only checked during business hours (Mon-Fri).
For more urgent questions or concerns, please call our Bariatric Clinic (425-502-3454) or Consulting
Nurse (1-800-297-6877) if after-hours.
31
Hotels
If you live a distance away and want to stay in an area hotel, there are several to choose from that are
very close, two that offer discounts to patients.
Discounts
Hotel 116 (Recommended)
Less than a block from Kaiser Permanente and Overlake
Offers Shuttle
625 116
th
Ave NE
Bellevue
425-455-9444
Red Lion
About 4 blocks from Kaiser Permanente and Overlake
Offers a shuttle to and from Overlake
11311 Main Street
Bellevue
425-455-5240
Other Hotels
Courtyard
11010 NE 8
th
St
Bellevue
425-454-5888
Silver Cloud
10621 NE 12
th
St
Bellevue
425-637-7000
Bellevue Lodge
11011 NE 8
th
St
Bellevue
866-539-0036
32

33
General Surgery ˗ at Overlake Hospital ˗ Instructions
The Medical Assistant will review this page with you on the day of your pre-op appointment.
An Overlake Hospital Nurse will contact you, about one week prior to your surgery, to do a pre-
registration.
Overlake Admitting/Check-In: will contact you the day before your surgery to tell you your check
in time.
One of the Bariatric RN’s will call or email with a surgery date, a day or two after your consult.
She will let you know when to do the things below.
__________ Pre-Surgery Physical (schedule with your PCP)
__________ Labs
__________ EKG (if ordered by surgeon)
__________ Other
If your primary care provider is not located at a Kaiser Permanente Medical Center, we will provide you
with a list of what you need, for you to take to your PCP at the time of you pre-surgery physical. You
will also need our fax number.
Please bring a current list of medications to all appointments
handout in your notebook
Avoid Aspirin and Ibuprofen products for one week prior to surgery (Naproxen, Motrin,
Aleve, Advil, Excedrin, Midol). Tylenol based products (Acetaminophen) are fine to take.
Your surgeon will give you instructions for stopping and/or taking certain meds before surgery.
Follow the prescribed Liquid Diet the DAY BEFORE surgery
See next page
Do not eat or drink anything after midnight (including mints & gum) unless otherwise instructed.
You need someone to drive you home, you will not be allowed to drive yourself home or use
public transportation.
Have someone stay with you for at least the first 24 hours after you return home.

34
DAY BEFORE SURGERY DIET
Follow the diet prescribed by your surgeon the day before surgery
You can drink as many of the listed liquids you need to stay full throughout the day.
No solid food; nothing blended
Do not eat or drink after midnight the night before your surgery.
Full Liquid Diet
Allowed:
Protein shakes
Protein water
Soup (liquid only)
Broth/Bouillon
Nonfat plain yogurt
Herbal tea
Clear juices: apple, cranberry, white grape
Non-dairy popsicles
Sugar-free gelatin
Water
Not Allowed:
Orange juice
Milk
Ice cream
Milk-based soups
35
Preparing for your Surgery
It is very important that you follow these instructions. Ask – if you have any questions!!!
30 days Prior to Surgery
Pre-Op history and physical within 30 days of your surgery date
Confirmation email/letter will provide specific instructions (if your surgery is within 30 days of your
pre-op consults, you may not need another one – follow the instructions provided)
There are blood tests that need to be done within 30 days of surgery
o These will be ordered for you and you will be instructed when to do them
You may also need an updated EKG. If this applies to you, we will let you know
STOP hormones (including birth control pills) 30 days prior to your surgery
2 Weeks Prior to Surgery
Stop taking all herbal supplements
o We know that some herbal supplements can increase bleeding risk or interfere with pain
medications / anesthesia, but many have not been tested.
1 – 2 Weeks Prior to Surgery
You will receive a call from Overlake Hospital for a pre-registration
If you do not receive this call within one week of surgery, you may call them at 425-688-5378
7 Days Prior to Surgery
Stop taking Aspirin and other anti-inflammatory medications (NSAID’s)
o i.e. Ibuprofen, Advil, Motrin, Naproxen, Aleve
Tylenol is fine to take
1 Day Prior to Surgery
Start clear/full liquid diet (liquids only all day the day before surgery
o See previous page for a list of clear / full liquid diet suggestions
Nothing to eat or drink after midnight or the morning of surgery
Follow medication instructions that you have been given by your surgeon
You will receive a call from Overlake Hospital with your check-in time
o Or you can call them any time after 9 am 425-688-5378
o If your surgery is on Monday you will receive this call on Friday (this also applies if your
surgery is Tuesday and Monday is a holiday).
36
The Day of Surgery
DO NOT eat or drink anything – other than medications you have been instructed to take, with
just a small sip of water.
Shower or bath the night before or the morning of surgery
o Bacteria on your skin can cause infection. Thoroughly wash between skin folds
o Do not apply lotion, creams, powders or oils
Do not wear make-up, face creams or hair products
Remove all jewelry (including wedding rings and body piercings)
Wear loose fitting clothes
Take medications as directed by your surgeon
o Make sure that you know which medications to take and not to take
o Taking a medication that you shouldn’t have could get your surgery canceled
Do not take vitamins, supplements or non-prescription medications
Do not bring medications to the hospital
Do bring inhalers, eye drops and nasal sprays, if you use these
Bring your APAP, CPAP or BiPAP machine, is you use one
o This is a must!!
In you have a pacemaker, bring the ID card
Bring your Kaiser medical card & picture ID
Do not bring large sums of money or valuables
Bring your advance directives, if they are not in your electronic medical record
Arrive at the given time and place (Overlake will provide this information)
Report to Overlake Hospital at the check-in time that you have been given.
o Your surgery date may or may not show up on kp.org/wa as an appointment.
Do not go by the time that you will see in kp.org/wa appointments, for the day of
surgery. The correct check-in time is the time that you are given by Overlake Hospital.
o It is very important that you show up by the given time.
Overlake Hospital will tell you where to park and where to report on the morning of surgery. You
may request a parking pass at the time of check-in at Overlake.
You must have a driver arranged to take you home on discharge
o You will not be released on your own or to public transportation
37
Arriving at Overlake Hospital
You have used the information in this guide to prepare for your surgery. The following information is
focused on the next phase of your care; your actual operation and the first days of your recovery.
Learning what to expect from your health care team and what you can do as you work with them can
give you:
Confidence
A feeling of control as you recover
Will help you achieve a successful outcome
The day of surgery is a busy one, filled with many new places and activities. The following information
will help you know what to do and what to expect on this important day.
Overlake Hospital is just north of the Bellevue Kaiser facility.
Traffic can be difficult at any time of day, coming from any direction. Please allow enough travel
time.
Overlake Hospital Admission
Answer questions and complete the hospital admission paperwork.
Be directed to the pre-operative area.
In the Peri-Operative Area you will
Confirm information from your preoperative paperwork
Have your vital signs taken and recorded
Have your weight recorded
Have your oxygen saturation measured by a pulse oximeter
Have an Intravenous line (IV) started
Receive an anticoagulation medication
Given an opportunity to ask any other questions with a nurse or your surgeon
Be encouraged to try to relax and feel comfortable
Meet with the Anesthesiologist
Just before you go to the operating room you will
Empty your bladder
Take off items such as underwear, any prosthetics, hairpin, and any metal jewelry including
rings. Hands can swell during surgery making it necessary to cut rings off. Jewelry should
be given to family or friends for safekeeping
Have visitors wait in the Surgical Waiting Area. The surgeon will speak with your family in
this area, after the procedure, while you are recovering in the Post Anesthesia Care Unit
(PACU)
Go by stretcher to an area outside the Operating Room, known as the Holding Area
Immediately before surgery in the Holding Area you will
Confirm your consent for surgery
May receive antibiotic medication through your IV
38
During surgery in the Operating Room (OR) you will
Be placed on the operating bed and secured with safety straps similar to seat belts
Have a SCD’s placed on your legs. These inflate and deflate simulating the act of walking
and stimulate the circulation of the feet and legs to help prevent blood clots from forming.
Never be left alone. The surgeon, anesthesia provider (Anesthesiologist or CRNA), and
other surgical assistants will be with you. They will be wearing surgical clothes, including
hats and masks and you may not be able to recognize them immediately
After surgery in the Post Anesthesia Care Unit (PACU)
A nurse will take your vital signs frequently
You may:
o Hear a lot of noise and activity
o Have an altered feeling of the passage of time
o Feel as if it takes a lot of energy for you to talk
o Not have any visitors
You may have:
o A foley catheter in your bladder to drain urine. If you do have a foley catheter, it will be
removed the day after your surgery. You will not need to urinate while the catheter is in
place.
o A small plastic tube (nasal cannula) with oxygen flowing into your nose. This will be used
through the first night after surgery. A pulse oximeter will be attached to your finger or toe
to measure the amount of oxygen circulating in your blood.
o A dressing(s) covering your incision(s), which have been closed by staples.
o Receive pain medicine. See Pain Control for more information about pain relief options.
o Be transferred to your hospital room after your anesthesia has begun to wear off and your
vital signs are stable.
39
In your hospital room after your surgery you will
You may be given ice chips and possibly sips of water on the day of surgery
The day following your surgery you will be started on clear liquids, as instructed by your surgeon
Have the head of your bed raised 30-45 degrees at all times, to increase the amount of oxygen in
your blood and to prevent reflux
Have your vital signs taken and recorded frequently
Be weighed daily
Have blood tests, as needed
Continue to receive oxygen, as needed
Use an incentive spirometer to take deep breaths to help reduce your risk of pneumonia, as
directed by your nurse
Receive pain medication, as needed to keep you comfortable. Refer to the Pain section, for
more information about pain control
Receive medications by IV to prevent infection, nausea, and excess stomach acid
Continue to use the SCD’s to help prevent blood clots from forming. The device is worn
continuously while in bed, during your hospital stay. Do not remove them yourself. Notify the
nursing staff, who will assist you when you get out of bed
Be encouraged to get up and walk, as able on the day of surgery and at least 3-6 times each day
thereafter
You will start to take small amounts of water, and remain on clear liquids while in the hospital.
Your IV will be disconnected from the tubing and capped with a saline lock, as you tolerate your
liquid diet. Refer to the nutrition section, for more information on diet and recovery
40
Pain
Some level of pain is to be expected
Postoperative pain is to be expected following a surgical procedure
With your help, your pain is managed to keep you comfortable
If your pain is not relieved, it is important to tell the nurse or doctor
Knowing what to expect and what to do about it, helps you prepare for the pain you experience
How you respond to pain is unique to you. You are the only one who really knows how it feels.
Your emotions also determine your feeling of pain
The pain you experience will diminish as you continue to heal
Pain control assists your recovery by
Providing comfort
Improves your ability to be active which helps to prevent complications such as blood clots and
pneumonia
You will play an important role in achieving good pain control. The following suggestions will assist your
health care team as they care for you and your pain
Request pain medicine when you begin to hurt
Rate or measure your pain using the scale below. This helps to describe what you feel when
talking about your pain with your nurse or doctor
No pain Mild Pain Moderate Pain Severe Pain Most Severe
I---------------------------------------------I--------------------------------------------I
0 1 2 3 4 5 6 7 8 9 10
Ask what to expect after taking pain medication
Tell your nurse or doctor if the pain does not improve after taking pain medication
Talk with your nurse or doctor about concerns you may have about taking pain medications
41
Types of Pain Control
Patient Controlled Analgesia (PCA):
You control your pain medication through your Intravenous Line (IV). A pump connected to your
IV gives you a prescribed dose of pain medication. You will be taught how to use the pump by
the nursing staff
Intravenous (IV) Pain Medication:
The nurse gives a prescribed dose of pain medication through your IV line
Pain Liquids or Pills:
The nurse gives a prescribed dose of pain medication in liquid or pill form. It takes about 30-40
minutes for the oral medication to start to work. As with all other analgesics, planning when to
take your medication allows you to achieve maximum comfort. Pills should be no larger than the
size of an aspirin or cut in half, if necessary. You will be sent home with narcotic pain
medication.
Pain Management:
Though pain from laparoscopic bariatric surgery is typically less than one might expect, it is
important to remember that everyone experiences pain differently. Please let your surgical team
or nurse know if you are experiencing pain, despite pain medication. This applies to when you
are home after surgery as well. Some patients use no pain medication at all once they are
home; others need to request a refill of their pain medication. Remember – you are an individual
with individual needs. Once home, call the bariatric clinic with any questions.
42
Blood Clots
After any major surgery there is a chance of developing a blood clot
A blood clot can happen when the blood flow through the legs is slowed as happens after
surgery, when you remain in bed for prolonged periods, or when you sit for long trips in cars or
airplanes
Most blood clot forms in the leg, however they may occur in any other part of the body. A blood
clot that develops in, or moves to the lungs is called an embolism. This can be life threatening
Blood Clot Prevention
The methods used to prevent blood clots for Bariatric Surgery are:
Fragmin, an anticoagulation medication, given by injection when first admitted to the hospital and
once a day until discharge form the hospital
SCD device is place on both legs. These inflate and deflate, stimulating the walking motion to
encourage circulation of the feet and legs to help prevent a clot from forming. SCD’s are worn
continuously while you are in bed. Do not remove them yourself. Notify the nursing staff if you
need to get out of bed
Ambulation, getting out of bed and walking at least three times a day, encourages circulation and
prevents blood from pooling in the legs
43
Leaving the Hospital
Patients will leave the hospital typically on the 2nd day after your surgery. Though you may go
home on the first day and on a rare occasion a longer stay may be necessary
You will need someone to drive you home from the hospital
Before you leave the hospital
The Surgeon or PA will:
o Make a plan for your medical needs, providing information about your incision, diet
limitations, medications, activity restrictions, follow-up appointments and what to watch
for. You will receive written discharge instructions in regards to medications and follow
up
The Nurse will:
o Review the instructions that your surgeon has given
o You are given a written copy of all these instructions
The Pharmacist will:
o Review your medications and make sure there are no drug interactions
You will:
o Make sure your questions have been answered
o Know what your discharge instructions are
o Know any medication changes that have been made
o Know when your post op appointment is scheduled for
o Have you driver available at the time of discharge
44

45
Obesity is a chronic disease that requires ongoing effort and permeant lifestyle changes. Bariatric
surgery is not a cure nor is it to be considered a “one and done” approach to treating obesity. Weight
loss surgery is a simply a tool to help you achieve a healthier weight and lifestyle.
In order to have a successful long-term outcome, it is necessary to make a number of permanent
lifestyle changes. You will need to change your eating habits, behaviors, mindset, stress management
strategies, and physical activity. While the nutrition plan is one of the most important parts of this
journey but it is not the only component to success. Establishing healthy self-care habits is the
key.
“A journey of a thousand miles begins with a single step.” ~Lao Tzu
Start Now!
•
Weight loss and optimal health is more than diet and exercise; it’s an accumulation of habits
that are integrated into your daily life.
•
The bariatric team expects you to start making small lifestyle changes now in preparation
for the surgery. Waiting for the pre op consults with the surgeon and dietitian to get
started sends the message you are not committed to the process.
•
The surgery only changes the size of your stomach; you have to do the rest to get the
results you want long term.
•
As you work through your Bariatric check list, begin to establish the healthy habits that will
make you successful.
•
The sooner you start, the more prepared you will be for the surgery, recovery, and for the
rest of your life.
•
Certain things will change once you have surgery; such as food intake, separating fluids from
meals, but the fundamentals are the same: healthy habits create a healthy body and life.
BARIATRIC NUTRITION &
LIFESTYLE PLAN

46
Building a Healthy Foundation
Fuel your body
•
Kick start your metabolism by eating breakfast within 1-2 hours after waking up.
•
Establish regular meal times throughout the day; never skipping meals or going more than
4 - 5 waking hours without eating.
•
Eating breakfast primes your metabolism to maintain stable
blood sugar levels after subsequent meals.
•
Studies indicate prolonged fasting might lead to a bigger than
normal increase in ghrelin, known as “hunger hormones.” This
encourages you to overeat at your next meal and leading to
peaks and crashes in your glucose and energy.
•
Choose protein and complex carbohydrates to get your day going.
For example: cottage cheese or yogurt with berries, a protein
shake and banana, veggie omelet.
Plan your meals
•
We live in a “high” society. Restaurants and grocery stores are packed with high fat, high
carb, high sugar and high salt foods.
•
When you don’t plan and prep your meals it’s easy to choose the fast, higher
fats/sugar/salt/carb foods when you need to eat.
•
Create a list of different meals you enjoy for each meal. (i.e. breakfast foods: protein and
fruit smoothie, cottage cheese and fruit, or egg and veggie scramble).
•
Having a few “go to” food items makes shopping and planning much easier to eat healthy
and less likely to eat out.
Protein
•
Protein is the cornerstone of your diet after surgery but not all proteins are created
equal.
•
High fat meats, such as pork sausage, salami, prime rib, bacon, and cheese can be substituted
for leaner, healthier options: fish, chicken, lean pork, lean red meat, low-fat dairy products,
eggs, and soy products.
•
Plant-based proteins (i.e. nuts, seeds, legumes, grains) do not contain all the essential amino
acids that are found in animal based proteins. These proteins also tend to be high fat (typically
healthy for your heart, but not your waistline), high carbohydrate and high calorie.
•
Start to substitute leaner proteins for the higher fat proteins. For example: substitute chicken
for beef when making tacos, eat lean ham in place of pork sausage.
•
Start to buy different protein shakes and powders to find ones you like. Drink them for
breakfast or as a quick snack.

47
Fruits & vegetables - 5+ a day
•
Vegetables and fruits are packed full of nutrients, are low calorie
and very filling.
•
Aim for 5+ servings a day (ratio of 3 vegetables & 2 fruits).
•
Start with 1 fruit and 1 veggie a day.
•
Gradually increase until consistently eating 5+ servings per day.
Serving sizes:
o One cup of fruit or vegetable - non-starchy veggies encouraged
o One piece of fruit (5 - 6 oz.)
o 3 cups of leafy raw vegetables: cabbage, spinach, lettuce
o ½ cup of legumes (black beans, garbanzo beans, lentils, etc.)*
Note: Legumes and beans are nutrient dense and higher calories per cup than
other vegetables. (Average cup: 200 - 300 calories and 10 - 20 grams of protein).
o Not recommended: dried fruit or juice
o Vegetables average 50 calories/cup
o Fruits average 100 calories/cup or piece
Fluids
Getting Started:
o Buy fresh, frozen and canned. Keep a variety on hand.
o Fresh and frozen vegetables and fruits are more nutritious than canned but canned
is still better than eating fast food. Keep a few cans of veggies you like in your
pantry.
o Use fresh garlic, herbs, spices and flavored vinegars to season your veggies. (i.e.
fresh ginger, curry, salt-free seasoning blends or balsamic vinegar)
•
Aim for 64 oz. of non-caloric fluids a day; water is preferred.
•
Post-surgery, you will be drinking sugar-free, non-carbonated,
herbal beverages so start exploring options now.
•
Buy an infused water bottle. Try different combinations such as
strawberries and kiwi.
•
There are many options available; here are a few suggestions:
o Try flavoring water with slice of cucumber or
citrus; lemon, lime or orange.
o Mio Liquid Water Enhancer (sucralose)
o Sweet Drops Liquid Stevia
o Water Drops (stevia)
o Propel Zero or Vitamin Water Zero
o Crystal Light Pure

48
Artificial sweeteners
•
NO NutraSweet/aspartame or Sweet & Low/saccharine products.
•
NutraSweet, also known as Equal or “the blue packet.” Aspartame is in A LOT of products.
For example: Crystal Light, diet soft drinks, sugar free Jell-O, puddings, popsicles, etc.
Sweet & Low are the “pink packets.”
•
If you are consuming products that contain aspartame, start to wean off of them and
incorporating new alternatives.
•
Try using Stevia, Truvia and Monk fruit products.
•
Try different brands and types of sweeteners to find one that you like and can tolerate.
•
Splenda (sucralose) is okay to use and is in many of the protein shakes.
•
Just like any other healthy habits, moderation is key.
Vitamins/Supplements
•
Start taking the vitamins and supplements daily to get into the habit.
•
You can take tablet form of the supplement prior to surgery. For the first 2 months
after surgery, liquid or chewable supplements are recommended.
•
These vitamins & supplements are specific to the bariatric surgery and you will be
taking them for the rest of your life.
•
Do NOT take the multivitamin with iron and calcium at the same time;
separate by 2 hours. Iron inhibits the absorption of calcium.
•
DO NOT TAKE ANY supplements in gummy form. Gummies do not have all the
vitamins and minerals you need, are not well absorbed & can get stuck.
•
See Tab 7 for more information and a list of recommended vitamins and
supplement brands.
Vitamins/Minerals Gastric Bypass Sleeve Gastrectomy
Multivitamin with iron: (chewable
or liquid)
1 svg/day 1 svg/day
Calcium Citrate with Vitamin D3
(chewable or liquid)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
Probiotic 1 svg daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA

49
Food Records
•
Start keeping food journal/records to increase your awareness of your food habits and track
the health habits necessary for success.
•
Food records increase your awareness around your eating habits. While it can be
uncomfortable writing down the “bad foods” you’ve eaten (i.e. chips, cookies, bread, ice
cream), it will give insight into your deep-seated eating habits so you can make plans in
how to change them. Food records are feedback, not failure.
•
You can buy a special food diary, a simple notebook, an online or phone app; choose the
type that works best for you.
•
Food records are a tool for you to learn what foods work best in your body and with your
lifestyle.
•
Keeping food records will also help the dietitian and bariatric team assess your
diet/nutrition and make recommendations if you have any challenges.
The Essentials Advanced
time of day hunger and fullness levels: before & after meal
food item(s) and amount (oz., Tbsp., cup) feelings/mood (happy, bored, depressed)
protein grams who you dine with (alone, coworker, family)
calories location of meal (work desk, in front of TV, car)
fluids – type & ounces post op: challenges, nausea, vomiting, or pain
list of vitamins & supplements taken food intolerances
exercise – type and minutes foods well tolerated & filling
Websites/Phone Apps:
www.baritastic.com
www.supertracker.usda.gov
www.CalorieKing.com
www.MyFitnessPal.com
www.FitDay.com
www.LoseIt.com

50
Portions are important
•
Start to become aware of how much you eat by weighing and
measuring your protein/meals.
•
Weigh and measure your food before eating your meal.
•
Start learning portions sizes now to be prepared after surgery.
•
A deck of cards is approximately 3 ounce of chicken or meat.
•
Put all extra food away before eating.
•
Use small dishes, glasses and child-size utensils. This will
make your portions look bigger and slow down your eating.
Eat mindfully
•
The practice of mindful eating helps raise your awareness of your thoughts, actions,
feelings, and motivations of why and what you eat.
•
A habit is a routine of behavior that is repeated regularly and tends to occur
subconsciously.
•
Many of the habits that drive food choices and overeating are these unconscious
behaviors that have been repeated for years; they are automatic and you may act on
them without even realizing it.
•
Eating mindfully raises your awareness so you can make changes.
•
This practice of eating slowly and mindfully is very important before and after you have
surgery.
Mindful eating includes:
•
Recognizing your body’s hunger and fullness signals.
•
Being aware of your emotional cues.
•
Identifying your non-hunger triggers for eating.
•
Learning to meet your other needs in healthy, effective ways
other than eating.
•
Fueling your body with foods that energizes you, nourishes
your body, and provides you satiety and satisfaction.

51
Mindful eating is eating with intention and attention.
Try some of these tips to eat mindfully and heighten your awareness:
•
Make a guideline to sit whenever you are eating (car not included).
•
Eat without distraction (TV, computer, phone or iPad) choosing a spot at home and work just for
eating, most likely the kitchen, dining room, or breakroom.
•
Savor each bite. Pay attention to flavors, textures, and consistency.
•
Notice any emotions/feelings you are experiencing.
•
Make eating a mindful and enjoyable activity. Set a placemat, use nice dishes, slow down and
savor the food.
•
Post op practice: when eating a meal, start with protein first and then vegetables.
•
Eat slowly, making meals last 20 minutes. Check in with your hunger level at 20 minutes and
decide if you are still hungry or full and ready to stop eating.
•
Take small dime-sized bites and chew food thoroughly.
•
Set your utensils down in between bites.
•
Make a sign that says “EAT SLOWLY” as a reminder.
•
Resign from the “clean plate club.”
Mindful eating exercise: Hunger/Fullness Scale
•
Many chronic dieters have learned to ignore their body’s hunger and fullness cues.
•
Diets have taught them to chew gum or drink a diet soda to help stave off hunger.
•
They are in the habit of cleaning their plate regardless of their fullness level.
•
Food may have become a coping strategy for a stressful day, to avoid conflict, or a way to numb
uncomfortable feelings.
•
At first, it may be difficult to determine your hunger cues and stop when you are full. Be patient.
•
Before a meal or snack, check in with your body and determine your hunger level.
•
Close your eyes, place your hand on your stomach, and take a few deep breaths.
•
Pay attention and listen to the cues your body is giving you.
•
Remember that taste buds are on your tongue and not your stomach; physical hunger is very
different than “head hunger.”

52
The Hunger-Fullness Scale
1 2 3 4 5 6 7 8 9 10
Use this scale (1-10) to help you identify your initial hunger when you begin to eat. This rating system is
purely subjective and will help you get in touch with your body’s inner signals.
Visualize your stomach getting emptier and hungrier as you go down on the scale to 1, completely
empty.
At 1, starving, completely empty, feeling weak/dizzy.
At 2, very hungry, irritable, low energy, stomach growling loudly.
At 3, pretty hunger; stomach is beginning to growl.
At 4, beginning to feel hungry.
At 5, satisfied, neither hungry nor full.
At 6, slightly full/pleasantly full.
At 7, slightly uncomfortable.
At 8, feeling stuffed.
At 9, very uncomfortable, stomach aches.
At 10, so full you feel sick, nausea.
Every time you start to eat check your hunger level. Ideally it should be a 3 or 4 level. If you
are at a 3 or lower, you’re over hungry and at risk for overeating.
•
Take the time to find discover what hunger and fullness feels like for you.
•
Fullness can range from the mere absence of hunger to physically suffering from stuffing too
much food in.
•
You won’t hear your body’s signals if you are multitasking at your desk or distracted by the TV,
phone or while driving.
•
Before, during and after you eat, rate your physical hunger and fullness.
•
Practice using this scale as often as possible.
•
Spend time getting to know the scale and use it shift your eating behavior.

53
Body awareness
We live in a culture that allows the mind to make all the decisions; usually at the expense of the
physical body. Pushing too hard at work, multitasking, and overcommitting are the norm. It’s time to
let your body be heard.
Check in with your body throughout the day to see what you need. Your body continually gives you
signals of what it needs. Tune in, listen, and learn what the signals are telling you.
•
Do you need a stretch break?
•
Is it time for a trip to the restroom?
•
Are you thirsty?
•
Need to rest your eyes from the computer screen?
•
Too cold? Too warm?
•
Need a hug?
•
Does a coworker leave you feeling drained or uplifted?
•
Are you hungry and ready for a meal?
•
Need to take a walk or be physically active?
•
Tired and ready for bed?
•
How do you feel?
Take the time to honor your body’s needs in healthy and constructive ways.
Mental mindset
•
The journey toward weight loss, weight maintenance and better health takes time, effort
and self-compassion. Surgery is not a quick fix.
•
Establish the mindset: strive for progress, not perfection. You will have challenges
and difficult times; it’s normal and it’s a learning process.
•
When things don’t go as planned, don’t beat yourself up; adopt the motto “its feedback, not
failure.”
•
Setting a small, achievable goal each day and reaching it will do better in the long run than
attempting to do things perfectly and coming up short.
•
Start slow, make course corrections when needed and keep going!
54
Photos and measurements
• Take photos & measurements now. You will be losing weight prior to surgery to meet your 5%
weight goal so start now to track your progress.
• The scale weighs everything: fat, muscle, water, organs, etc., and will not always display the
success you are achieving.
• By taking measurements and photos you will have additional evidence of your success to
keep you motivated throughout this journey.
• Take photos (front & side) and measurements (chest, waist & hips) every month.
• The first month, choose one outfit you want to keep from your start weight. This will be your
“before” outfit.
• Every month after surgery, take 2 photos. In the first photo wear the “before” outfit. In the
second photo wear clothes that fits properly and shows your weight loss. In just a few months
post op, you will see the before outfit get bigger and bigger while the second photo will show
the physical transformation occurring.
• Print these photos and tape them to your mirror to look at daily. This will help your mind catch up
with your body. Often patients look in the mirror and don’t see their true body image.
Clothes
•
Go through your clothes; sorting and grouping the different sizes.
•
Keep the next smaller size ready. You will lose quickly and sometimes clothes can be too big in
a matter of a week or two.
•
When clothes get too big for you to wear, donate them; you don’t want the mindset of having
a closet full of bigger clothes “just in case” you gain back weight.
•
Instead, focus on implementing the healthy habits that will maintain your weight loss for life and
imagine all the new, smaller sized clothes you will wear.

55
Prep your home
With your family’s help, clean out the pantry, freezer,
and refrigerator of food challenges. Stock with healthy
options: fruits, vegetables, lean proteins and protein shakes.
•
Place a bowl of fruit on the counter and cut up veggies in a clear
container in the fridge.
•
Keep the foods that tempt you out of the house.
•
If family members want tempting foods in the house, designate a specific area for them,
out of sight and accessibility.
•
Use smaller plates for your meals.
•
When serving meals, keep pots or serving platters on the stove – not on the table.
•
Store leftovers immediately after meals or immediately throw them in the trash.
•
Designate space on the kitchen counter and cupboard just for your things.
•
Start collecting the protein shakes and powders, sugar free syrups, extracts, flavored waters
and drops, herbs, spices and food journal needed after surgery.
•
Once you’ve had surgery, keep the blender, protein shakes, scale, and other things you will
need, right on the counter, for you to see and use easily.
•
Make sure your home is your haven - free from tempting foods.
Change your food shopping habits
•
Make a shopping list.
•
Place lean proteins and fruits and vegetables at the top of the list.
•
Avoid grocery shopping on an empty stomach; it will save your waistline and wallet.
•
Shop the supermarket perimeter. Most whole foods are found along the walls of the store and
it decreases temptation.
•
By avoiding the inner isles, you can avoid the highly processed and tempting foods.
•
Buy only the items that are necessary for you and your family.
•
Avoid buying food items for other people that you may eat. If the thought, “But it’s for the kids”
pops into your head, take a moment and ask
yourself if you would eat it too if it was in the house.
If the answer is yes, put it back on the shelf.
•
For vegetables and fruits, buy canned, fresh and frozen.
While canned is not as nutritionally dense as fresh or
frozen, it is easy to have on hand and better than fast
foods choices.
•
Buy canned or fresh packed its own juice, no added
sugar or syrup.

56
Things to buy
Purchase the items you will need for the pre and post-surgery diets.
•
Blender
•
Ice cube tray – to freeze small portions of pureed foods.
•
Small dishes and utensils (child-sized).
•
Measuring cups, measuring spoons and a food scale. These items
are needed to determine the exact portion sizes of the food you eat and drink.
•
Crockpot – to prepare moist proteins, i.e. chicken or pork loin.
•
Food journal or food record app – to track your protein, calories and all other habits
needed to lose the weight and be healthy.
•
The vitamins & supplements required for Bariatric surgery (see section 7 for more
information). Buy both solid/tablet form to take now and liquid or chewable form for the
first 2 months post op.
•
High Protein, low sugar beverages and powders. Be aware your taste preferences
might change after surgery so you may not want to buy protein shakes a case at a
time.
•
Buy a variety of flavors and brands of protein shakes/powders to ensure you have
options after surgery.
•
Sugar-free syrups made with sucralose (i.e. DaVinci and Torani brands) will make your
vanilla and chocolate protein shakes more appetizing (i.e. vanilla shake with SF raspberry,
caramel, or coconut. The chocolate shake with SF mint, coffee, or amaretto). Cash & Carry
have a wide selection for a lower price.
•
A supply of sugar-free, non-carbonated, non-caffeinated beverages. Herbal tea, Propel
water, Sweet Leaf stevia drops, etc.
•
Herb and spice blends – these help to make your protein meals more flavorful and
interesting during the post op diet progression. (i.e. Italian blend, Creole seasoning,
curry powder, etc.). No hot sauces or cayenne pepper for the first two months after
surgery. Your pouch needs time to heal.

57
Physical Activity
When planning for bariatric surgery, it’s easy to focus only on the diet
and overlook exercise. In reality, exercise is just as important as your
diet for your long term success. There are many benefits you will reap
when you exercise regularly but the most important as you proceed
with this surgery is you will lose more weight and have an easier time
maintaining it.
For many, the thought of exercise conjures up images of the gym,
every day for an hour, sweating and huffing and puffing; followed by soreness and fatigue caused
by being too aggressive right away. Stop! It doesn’t have to be that way. Instead, start slow so
you don’t get discouraged or injured. Think small, do-able steps.
10 minute rule
•
Begin with 10+ minutes a day of some type of activity.
•
Knowing you only have to do 10 minutes can make getting started much easier.
•
If you want to continue after 10 minutes, go for it!
•
If you are done at 10 minutes, congratulations, you met your goal.
•
Walking is the easiest and most accessible form of activity for most people.
•
Wear good shoes. Buy shoes that feel good right away, without need to “break them in.”
•
Activate your lifestyle: park farther away, take the stairs, clean the house, mow the lawn,
and take stretch breaks at your desk. It all adds up.
•
Joint pain is not healthy pain. If the exercise causes pain, modify the exercise to alleviate
the pain or stop.
•
If you have physical limitations in your lower body, try performing your strength
exercises from a seated position.
•
Try “Sit and Be Fit” videos or a mini exercise bike petal system for upper body.

58
Note: Some patients may find it difficult to exercise prior to surgery due to health conditions such
as shortness of breath upon exertion, knee or back pain, and heart conditions.
Always check with your primary care physician before starting an exercise routine.
Benefits of Exercise:
•
Increased life expectancy
•
Burns calories
•
Reduces fat while building muscle
•
Weight management
•
Lower blood pressure
•
Improves mood and self-esteem
•
Improved blood sugar control
•
Improved insulin control
•
Helps control hunger
•
Stronger bones and muscles
•
Improved sleep
•
Increased energy
•
Improved balance
•
Reduced cholesterol
•
Relieves stress
Strength Training & Flexibility
For long term success you will need to incorporate strength training and stretching/balance into your
routine.
•
Strength training is essential to losing weight after surgery; it helps you build muscle, burn
more calories, and improve balance. With your doctor’s permission, you can begin strength
training at least 3 times a week.
•
Stretching activities that stretch and lengthen muscles can help you prevent back pain, injuries,
and balance problems. Activities such as yoga combine stretching and relaxation and also
improve balance; a great way to relax and unwind from a stressful day.

59
Sleep
Most people don’t realize that a lack of sleep, especially on a regular basis, has long-term health
consequences.
Chronic lack of sleep can lead to:
•
diabetes
•
obesity
•
high blood pressure
•
heart disease
•
early mortality
Sleep plays an essential role in good health and well-being throughout your life.
•
Getting enough quality sleep can help protect your physical and mental health, your quality
of life, and safety.
•
Sleep affects almost everything in your body: immune system, stress hormones,
appetite, blood pressure, and cardiovascular health to name a few.
•
Get enough sleep. Aim for 7 - 8 hours a night. Some people will need more.
Benefits of sleep:
•
Better weight control
•
Manage blood sugars
•
Boost immune system
•
Improved mood
•
Boosts creativity and focus
•
Lower risk of injury
•
Clearer thinking
•
Better memory
•
Quicker reflexes
•
Less pain
A few ideas for better sleep hygiene:
•
Avoid alcohol, caffeine, or nicotine. They disrupt sleep.
•
Exercise early in the day to help you fall asleep faster and sleep more soundly.
•
Avoid difficult conversations or arguments before bed.
•
Turn down the lights an hour before bedtime. This signals your body it’s time to rest.
•
Establish a relaxing pre-sleep routine to help with the transition to sleep time. Read a book,
meditate, or take a bath or shower to wind down.
•
Power down. Light from the TV, cell phone, tablets can prevent you from falling asleep.
•
Keep your bedroom, dark, cool and quiet for a better slumber.
•
If you have sleep apnea, use your C-pap machine.

60
Stress Management
• Our bodies are hard-wired to react to perceived danger and stressful situations.
• Threats of predators or other aggressors are rare today but the insidious stressors of work
responsibilities, commuting, keeping up on home chores, caring for a family, and making ends
meet can take their toll.

61
Negative effects of stress on your health on mind, body, emotions and behavior:
•
Overeating
•
High fat/high calorie food choices
•
Drinking too much alcohol
•
Lack of exercise
•
Headaches
•
Fatigue
•
Tight muscles
•
Insomnia
•
Nightmares
•
Restlessness
•
Worrying
•
Indecision
•
Negativity
•
Impaired judgement
•
Apathy
•
Depression
•
Irritability alienation
•
Loss of confidence
All of these consequences can derail your weight-loss efforts. Integrating daily stress management
habits can counteract the negative effects of stress and bring positive outcomes like increased
productivity, better health and more happiness in general.
Here are a few ideas to get you started:
•
Take 3 - 5 long, slow deep breathes
•
Hug your spouse, kids or pet
•
Walk away for a stressful situation
and cool down for 5 - 10 minutes
•
Call a friend for support
•
Adult coloring books
•
Long hot shower or bath
•
Blow bubbles
•
Take a 10 minute nap
•
Gardening
•
Go for a walk
•
Smell a rose, hug a loved one or smile at
your neighbor
•
Read a good book
•
Try meditation or prayer to break the
negative cycle
Hobby
Meditation
Nature
Exercise
Time
Manage-
ment
Music
Laughing
Stress
Management

62
Support
•
The treatment of obesity is a lifelong process that requires continued support. Having a strong
support network will help keep you on track when old maladaptive behaviors pop up.
•
Be mindful who you want to know about your surgery. Some people may not agree with
your decision and make unfavorable comments. The people you choose not to tell is
just as important as the people you choose to tell.
•
Determine the type of support/help you prefer.
•
Let your family and friends know how they can support your efforts.
•
Ask for the support and help you need and be willing to receive it.
A few ideas:
o Keep all of your appointments with the bariatric medical team.
o Line up a few walking buddies and schedule regular walking dates.
o Have your spouse watch the kids so you have time to exercise.
o Ask family members keep tempting foods out of the house or hidden.
o Tell people who do not agree with your decision to be supportive by remaining silent
about your decision.
o Let well-meaning friends know that you enjoy compliments but would rather not hear
about bariatric failure stories.
o Receive encouraging comments on the habits you are establishing such as
walking, drinking water or keeping food records.
o Ask spouse to cook healthier foods for you.
o Have a loved one come to the Bariatric support groups and medical appointments
with you so they have a better understanding of your process.
63
Nutrition Support with the Bariatric Dietitian
The Bariatric dietitian is here to provide the education and support you will need to optimize your nutrition
and maximize your weight loss. The surgery alters your anatomy, making your nutritional needs very
different from before surgery. You will need to establish and maintain eating habits that will be new to you.
The dietitian will assist you in creating a plan to meet your needs.
Pre op appointment: review the diet stages pre and post- surgery, give ideas to make the diets as
enjoyable as possible, create a plan, and answer all of your questions.
• Post op appointment: 7 - 10 days after surgery, review your
progress, plan for the upcoming diet stages, and answer your
questions.
• 2 month appointment: review your progress, tweak your
• plans to maximize your weight loss and meet your nutritional needs, and answer your questions.
• 6 month appointment: review your progress, make a plan to meet your ongoing
nutritional needs, and answer your questions.
• Ongoing support: access to the Bariatric dietitian through phone at the Kaiser Permanente
member website kp.org/wa; My Chart.
Preparing for your bariatric appointments
Your bariatric team is here to support you through this process. At every visit or phone call you will be
asked a series of questions to help assess your progress. Keeping food records and having them totaled
and ready will help expedite this process. The better prepared you are with the answers to questions, the
more time you will have to ask questions and receive the care you need.
Have this information ready to go for all your appointments.
Bring all of your questions, concerns, or comments!
•
Any nausea, vomiting or other problems?
•
Keeping food records?
•
Daily average of protein grams?
•
Protein sources (i.e. protein shake, yogurt, chicken, eggs, cottage cheese)?
•
Daily average of calories?
•
Daily average of fluids? Types of fluids?
•
Separating your fluids from meals? (post op Stage 3 and beyond) and number of minutes
before &/or after meal?
•
List of your daily vitamins & supplements. Chewable/liquid or regular?
•
Are you exercising? What type, how much?
•
Are you staying full?
•
Any problems with grazing?
•
What questions do you have today?

64
Bariatric surgery is only the “starting line” of this treatment. The diet you follow after surgery
and for the rest of your life will affect your ability to manage your weight. The diets before
surgery and after are very different and move through many stages.
Before Surgery:
•
Pre-op Diet (2-4 weeks)
•
Day before surgery diet
After Surgery:
•
Stage 1 Clear liquid diet (in hospital only)
•
Stage 2 Full liquid diet (2 weeks for Bypass, 4 weeks for Sleeve)
•
Stage 3 Puree diet (3 weeks)
•
Stage 4 Soft diet (2 weeks)
•
Stage 5 Regular bariatric diet (high protein, carbs from vegetables, fruits & legumes)
Diet Progression
Progression
Diet
Duration
Dates
Pre-op 3+2+5
2 weeks (BMI <50)
4 weeks (BMI >50)
Day
before
Surgery
Full Liquid or
Surgeon Instructions
1 day
1 day
Surgery Day No food or drink 1 day
Stage One
Clear Liquid
(in hospital only)
2 days
Stage Two
Full Liquid
(when discharged)
2 weeks (Bypass)
4 weeks (Sleeve)
Stage Three Pureed 3 weeks
Stage Four Soft 2 weeks
Stage Five Regular Bariatric Ongoing
BARIATRIC DIET
PROGRESSION

65
The purpose of the pre-op diet is for your safety and help to:
•
Shrink the liver. The liver sits on top of your stomach. When you gain weight, the liver gets
larger. The pre-operative weight loss diet helps to shrink the liver and gives the surgeon
greater visibility and more space to work.
•
Make the operation safer; reduce the risk of major complication such as leaks, infection,
and the need for readmission to the hospital or the need to re-operate.
•
Prevent the “last supper syndrome” and weight gain. Many people spend days or even
weeks overeating all their favorite foods believing that having weight loss surgery is the end
of eating as they know it. Don’t worry, food won’t go away forever, you will just eat differently.
Your eating will change dramatically and you will likely prefer foods that are healthier as you
are losing weight. You will focus on quality rather than quantity and you may still have some
of the same foods but in different portions and different preparation.
•
Meet your 5% goal weight. We highly recommend you are close to or have reached your
5% goal weight at the time of your pre op consults with the surgeon and dietitian.
Note: some patients may be required to lose more weight per the surgeon’s instructions.
•
Establish as many healthy habits prior to surgery as possible. After surgery you are
learning how to eat and drink in a completely new way. The more habits you have
integrated into your life (i.e. food records, taking bariatric vitamins, exercising, etc.) the
easier your transition post op will be.
•
Reduce decision anxiety. By following the pre-op diet, you will reduce decision anxiety
around food since you will have a specific meal plan. You can start to focus on positive
behaviors related to eating and using other coping methods.
When to start the Pre-Operative Diet:
If your BMI is less than 50, start the diet 2 weeks before your surgery date.
If your BMI is greater than 50, start the diet 4 weeks before your surgery date.
Please make sure to read this part carefully and follow these instructions. You will be reviewing this diet
during your first visit with the dietitian.
Please bring this binder with you for ALL visits.
PRE-OP DIET
Preparing for Surgery

66
PRE-OP DIET
3+2+5 Daily Food Plan - these are your only food
options:
3+ Protein shakes
2+ Low calorie entrees
5+ Servings of fruits & vegetables
This food plan is designed to provide a structured diet that will simplify your food/meal choices,
provide balanced nutrition, and keep you fueled and full throughout the day.
Recommended Meal Replacement Products
Shakes (a few examples)
Premier Protein Shake
Bariatric Advantage
Pure Protein
Entrees
Lean Cuisine® entrees
Healthy Choice® entrees
Weight Watchers® Smart Ones entrees
Atkins® entrees
*Most entrees average 200-400 calories.
Fruit and Vegetables
A serving is:
One cup of fruit or vegetable - non-starchy veggies encouraged
One piece of fruit (about 5 - 6 oz.)
3 cups of leafy raw vegetables: cabbage, spinach, lettuce
½ cup of legumes (black beans, garbanzo beans, lentils, etc.)
Note: Legumes and beans are nutrient dense and naturally higher in calories per cup than other
vegetables. Average cup: 200 - 300 calories and 10 - 20 grams of protein.
o You can eat fresh, frozen and canned veggies and fruits.
o Fresh and frozen vegetables and fruits are more nutritious than canned but canned is
still better than eating fast food.
o Keep a few cans of fruits and veggies you like in your pantry.
o Buy canned fruit packed in its own juice; no heavy syrup or sugar added.
o Use herbs, spices and flavored vinegars to season your veggies. (i.e. fresh ginger,
curry, salt-free seasoning blends or balsamic vinegar)
*Aim for the ratio: 3 vegetables & 2 fruit servings per day
o Most vegetables average 50 calories/cup
o Most fruits average 100 calories/cup or piece
Note: No juice or dried fruit.

67
Sample day:
Breakfast: protein shake
Snack: 1 piece fruit
Lunch: low calorie entrée + 1 - 2 cups veggies
Snack: protein shake
Dinner: low calorie entrée + 1 - 2 cups veggies
Snack: protein shake with1 cup frozen fruit
•
This diet plan will provide a minimum of 1200 calories and 90+ grams of protein per day when
you eat at least 3 protein shakes, 2 low calorie entrees and 5 servings of fruits & vegetables.
•
You do not need to go hungry; you can always have another shake, more fruits & vegetables
or even an extra entrée(s). An extra protein shake is better than grabbing for chips or going
through a fast food drive through.
Men: may need to eat more to stay full; averaging 1400-1800 calories per day.
Women: may need fewer calories; averaging 1000-1400 calories per day.
•
f you cannot eat everything on the pre op diet (3+2+5); it’s okay. As long as you are eating 3
meals a day, eating breakfast within 2 hours of waking up, never going longer than 5 waking
hours without eating, and are staying full, you don’t have to get all the servings in. Stop eating
when you are full. This is great practice for after surgery.
•
Eat at regular times throughout the day; never go more than 4 - 5 waking hours without
eating. Fueling your body thoughout the day increases your energy and allows you body to
lose weight.
•
When to start the pre op diet: you will be on the pre op diet for either 2 or 4 weeks, depending
on your BMI. Once you have your surgery date you can calculate the dates you need to be on
the diet with an added day for the “day before surgery diet.”
•
Reaching your 5% with a modified pre op diet: Many patients like to start a modified version
of this diet right away to help reach their 5% weight goal. You can start now by have a protein
shake for breakfast rather than skipping, eat more veggies and fruits for snacks, and having a
low calorie entree for lunch.

68
Food records
•
Start keeping records if you haven’t already.
•
This is an essential part of your success and the Bariatric team will ask about your food,
fluid, vitamin intake, and exercise, etc.
The Essentials Advanced
time of day hunger and fullness levels: before & after meal
food item(s) and amount (oz., Tbsp., cup) feelings/mood (happy, bored, depressed)
protein grams
who you dine with (alone, coworker, family)
calories location of meal (work desk, in front of TV, car)
fluids - type & ounces post op: challenges, nausea, vomiting, or pain
list of vitamins & supplements taken food intolerances
exercise - type and minutes foods well tolerated & filling
Vitamins/Supplements
•
Start taking the required supplements if you haven’t already.
•
Regular vitamins are permitted after surgery but most patients find taking either liquid or
chewable for the first 2 months after surgery more comfortable.
Separate the multivitamin with iron and calcium citrate by 2 hours.
NO GUMMY SUPPLEMENTS OF ANY KIND.
Vitamins/Minerals Gastric Bypass
Sleeve
Gastrectomy
Multivitamin with iron: (chewable
or liquid)
1 svg/day 1 svg/day
Calcium Citrate with Vitamin D3
(chewable or liquid)
500 - 600 mg svg,
3x/day
(1500 - 2000 mg day)
500 - 600 mg svg,
3x/day
(1500 - 2000 mg day)
Probiotic 1 svg daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA

69
Fluids
Aim for 64 ounces of non-caloric fluids a day. Water is preferred.
•
Post-surgery, you will be drinking sugar-free, non-carbonated, non-caffeinated beverages so
start exploring options now.
•
Try flavoring water with slice of cucumber or citrus; lemon, lime or orange.
•
Carbonated drinks, coffee, tea (both decaf and regular) and other caffeinated beverages are
not permitted after surgery, so you may want to wean off of them now.
Fluids after surgery:
•
No carbonated beverages; that is a permanent change.
•
No coffee or tea (decaf include) for the first 2 months after surgery.
•
In Stage 2 - Full Liquid, you will start to separate your clear fluids from your full liquid meals.
•
In Stage 3 - Pureed you will now need separate your fluids and wait 60 minutes after
your meals and snacks to drink clear fluids again. Separating fluids from meals is a
lifetime habit.
•
Drinking with your meals can wash food through too quickly causing dumping, take away the
feeling of being full and lead to overeating. For others, drinking may fill them up and prevent
them from getting enough protein or cause pain and vomiting.
•
Practice separating your fluids from your meals. Wait 60 minutes after your meal before
you drink liquids again.
Exercise
•
Start being active if you haven’t already.
•
Aim for doing some type of physical activity for 10+ minutes a day.
•
Work on consistency and looking for ways to incorporate more activity into your life.
•
Gradually increase over time.
•
Developing an exercise routine is vital to maximizing your weight loss and keeping it off!

70
Dr. Gupta
Full Liquid Diet
Dr. Landers
Clear Liquid Diet - Bowel Prep
Allowed:
Protein shakes (from pre-op diet)
Whey or soy powdered drinks
Nonfat plain yogurt (sweeten with stevia or
sugar-free syrups)
Soup (liquid only soups)
Vegetable Juice
Broth, Bouillon, bone broth
Herbal tea
Not Allowed:
Fruit juices
Ice cream
Allowed:
Clear soup/broth/bouillon
Herbal tea
Clear juices: apple, cranberry, white grape
Nondairy popsicles
Sugar free gelatin
Water
Not Allowed:
Orange juice
Milk
Ice cream
Milk based soups
You can drink as many of the listed beverages
or protein shakes you need to stay full
throughout the day.
NO SOLID FOODS OF ANY KIND;
NOTHING BLENDED
Laxative:
Suprep 1 bottle at 8:00 am.
1 bottle at 8:00 pm
Fluids:
Be sure to drink plenty of clear fluids to avoid
dehydration from the laxative.
You may continue to drink clear fluids until
midnight the night before surgery.
REMEMBER: DO NOT eat or drink after midnight the night before your surgery.
DAY BEFORE SURGERY DIET

71
Nothing to eat or drink the morning of surgery; except enough water to swallow the medications
you’ve been instructed to take. If you eat or drink anything the morning of surgery, it will be cancelled.
•
This means no food, beverages, mints, or gum. You can brush your teeth, rinse and spit.
•
Know which medications to take and which to stop.
•
You will not be eating or drinking the day of surgery, though you may be given ice chips after
surgery.
Goal
The goal of the clear liquid diet is to provide liquids that are easily digested (broken down) and
do not put a strain on your new stomach or intestines.
• The clear liquid diet does not provide all the nutrients, vitamins, minerals, or calories that your
body needs.
• A clear liquid diet is made up of clear liquids and foods that are liquid at room temperature.
• Clear liquids include: water, clear broth, sugar-free Jell-O and sugar-free beverages, herbal
tea.
On Day 2, while in the hospital, you will be instructed to sip slowly and gradually increase your fluids:
1oz every hour for 4 hours
2oz every hour for 4 hours
3oz every hour for 4 hours
4oz every hour for 4 hours
Overlake Hospital offers sugar free Jell-O and beverages made with NutraSweet (aspartame). Your
bariatric team does not recommend this artificial sweetener; however if you want it while you are in the
hospital that’s okay. If you do not wish to have this, simply refuse it and ask for something else.
DAY 1
DAY of SURGERY
DAY 2 - in hospital
STAGE 1 CLEAR LIQUID

72
You will go home on the third day if all goes well. You will most likely be able to drink 1 oz. every 15
minutes. The most important thing is you practice drinking slowly to avoid pain or dumping.
Discharge from the hospital is usually between 11:00 am – 1:00 pm.
Once home you start the full liquid diet.
Your home should set up and be ready for you:
· Protein shakes and powders – a variety of brands and flavors.
· High protein soups
· Broths, liquid only soups and low fat cream soups
· Yogurts – nonfat plain Greek yogurt and other SF, nonfat flavors with no fruit at the bottom
· Bariatric chewable or liquid supplements (multivitamin, calcium citrate, probiotic,
· and Vitamin B12 (bypass only)
· Sugar free syrups and PB2
· Herb and spice blends
· Small dishes and spoons
· Shake bottles
· Food record – app or journal
Post Op Dietary Goals
The post op diet progresses through 5 stages over about 2 months’ time. This progression is designed
for your health and safety. The diet progression is a medically prescribed diet will help you:
· Maximize your protein intake to assist wound healing and preserving as much muscle
mass as possible.
· Minimize occurrences of dumping syndrome or physical complications.
· Make the diet as enjoyable as possible.
Dumping Syndrome
· Dumping syndrome is the result of the rapid emptying of foods or beverages into the small intestine.
· Dumping is an expected consequence to what you ate or drank (high fat or sugar) and how
you did it (too fast, too much).
· When high concentrations of sugar or fat hit the small intestine, it causes an influx of fluid into the
small bowel. This can lead to dumping.
· This is less likely to happen with the sleeve, but it certainly can, when eating inappropriately.
DAY 3 - discharged home
Clear Liquids to Full Liquid

73
Symptoms
· Diarrhea
· Nausea
· Vomiting
· Pain
· Abdominal cramps
· Bloating
· Epigastric fullness
· Sweating
· Headache
· Flushing
· Lightheadedness
· Palpitations (rapid heart rate)
· A strong desire to lie down
Preventing Dumping Syndrome
· Avoid foods that are high in sugar &/or saturated fats.
· Do not drink with your meals, use a straw, or drink carbonated beverages.
· Don’t eat full fat dairy products. Low fat dairy is typically fine.
· Avoid ice cream, cookies, juices, rice, pasta, bread, crackers, pizza, and similar foods.
· Avoid high fat meats, like hot dogs, burgers, pork sausage, bacon, pepperoni, etc.
No
Straws!

74
The start date of the full liquid diet is the day you are discharged home (not day of surgery).
Duration: Bypass = 2 weeks
Sleeve = 4 weeks
GOALS
This is a prescribed nutrition plan to allow the staple line in your stomach to heal without being
stretched. Follow the diet guidelines to avoid side effects and complications.
• Protein: minimum 40 - 50+ grams/day; more if tolerated. Your first priority will always be to get
in your protein.
• Calories: average 300 - 400+ calories/day; more at times, depending on the person &
procedure.
• Number of meals: 4 - 6 meals. The protein shakes, yogurt, & soups (with protein powder
added) are your meals. You will be eating and drinking throughout the day. Most meals average
2 - 4 oz.
• Length of meal: Meals should take a full 20 minutes to finish; no more than 30 minutes.
• Mindfulness: eat or drink very slowly; taking small, dime-sized bites or sips. Listen to your
body to determine the amount you can consume in the 20 - 30 minute period; checking in often
to determine your last sip/bite “threshold.”
• Total fluids: minimum 40 - 50+ ounces/day; more if tolerated. Aim for 4-6 ounces per hour to
meet this goal. No coffee/tea; including decaf or green tea for first 2 months; it’s too acidic. No
straws: this is a lifetime habit. Sip throughout the day & avoid gulping.
Fluids include: water, herbal tea, broth, stevia or Mio drops, sugar-free flavored water (i.e.
Vitamin Water Zero or Crystal Light Pure. You may need to vary fluid temperatures. Protein
shakes can count toward your total fluids during this stage only (Stage 2- Full Liquid).
• Separate Fluids from Meals: separate clear fluids (i.e. water, broth) from your full liquid meals
(protein shakes, yogurt, soup with protein powder). You may drink clear fluids again right after
your meals. Waiting 60 minutes before drinking fluids again does not begin until Stage 3.
Stage 2 - FULL LIQUID
(once discharged home)

75
FULL LIQUID GOALS – continued
• Food Records: keep daily records! Though your meals/nutrition intake is repetitive during this
stage, keep food records to reinforce this habit of writing down your food and fluids. This is
essential to long term success!
Records include: time of day, food, amount (oz., cup, Tbsp.), protein grams, calories, fluids
(type & amount), exercise (type & minutes), and any challenges, symptoms or questions.
• Vitamins/Supplements: liquid or chewable for the first 2 months after surgery are easiest to
take. Separate the multivitamin with iron and calcium citrate by 2 hours.
NO GUMMY SUPPLEMENTS OF ANY KIND.
Vitamins/Minerals Gastric Bypass
Sleeve
Gastrectomy
Multivitamin with iron
(chewable or liquid)
1 svg/day 1 svg/day
Calcium Citrate with Vitamin D3
(chewable or liquid)
500 - 600 mg svg,
3x/day
(1500 - 2000 mg day)
500 - 600 mg svg,
3x/day
(1500 - 2000 mg day)
Probiotic 1 svg daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA
· Exercise: you will take gentle, short walks even while you are in the hospital. Once home, for the
first 2 weeks, no more than 10 minutes per session and no than 20-30 minutes per day.
· Start slow, move often; walk around every 1-2 hours. Remember you just had major surgery and
can tire and fatigue easily. When exercising, listen to your body. If you feel as if you are pushing
yourself, stop!
· After 2 weeks, incrementally increases every week until you are doing 30 - 45 minutes per day,
5 - 7 days a week.
· Do not lift weights or swim until your surgeon gives you clearance.

76
Full Liquid Food Options
Protein Shakes & Powders:
Many patients taste preferences change after surgery.
Have several different brands and flavors on hand in case
this happens to you.
Buy a variety of protein shakes and powders to determine
the ones you like best.
Chocolate, vanilla, unflavored protein powder, and chicken
soup can be flavored to your liking.
After surgery, your nutritional needs have been changed so
you will need to
read the labels to ensure you are meeting your protein
requirements.
Inadequate protein shakes can lead to high calories, low
protein intake as well as dumping syndrome if the sugar
content is too high.
Yogurt: no chunks, no added sugar, no added fruit.
•
Non-fat, plain Greek yogurt (i.e. Fage, Oikos).
•
Stir in flavored protein powders (i.e. chocolate) SF syrups (i.e.
DaVinci), stevia flavored drops (i.e. Sweet Leaf) to add variety
of flavors.
•
Buy several different flavors to increase variety.
Soups and Broths with unflavored protein powder added.
High protein soups: beef, chicken, or tomato protein soup
Liquid only soups (i.e. tomato, squash, carrot)
Low-fat cream soups (i.e. chicken, mushroom, broccoli) strained
There are many unflavored protein powders available. Make sure
to keep temperature under 140 degrees.
Broth, bouillon, or consommé, or bone broth are clear liquids. You
can add protein powder or NF plain Greek yogurt to make them into
a meal/protein source.
No high fat cream soups, no chunks, and no broth-based soups
with noodles, rice, grains.
No chili, bean or lentil soups (these are allowed in Stage 3, pureed).
IMPORTANT: Follow the diet guidelines your bariatric dietitian has provided you. You will find a
lot of information about post op bariatric diets available on the internet and through friends and
family but they may not be in alignment with what your bariatric surgeon, dietitian, and team
want you to follow. When in doubt, contact the dietitian and ask first.

77
Formula for high protein shakes and powders:
•
150 - 180 calories or less
•
20+ grams of protein
•
< 7 grams of sugar
•
No aspartame (NutraSweet). Sucralose (Splenda) is okay.
AVOID: high calories & sugar, low protein BEST: high protein, low calories & sugar
BEST: high protein, low calories & sugar
BETTER: but protein is low
NUTRITION FACTS
Serving Size: 3 scoops (60g)
Servings per Container: 9
Amount Per Serving
Calories 240
Calories from Fat 70
% Daily Value
Total Fat 7g 11%
Saturated Fat 1g 5%
Trans Fat 0g
Cholesterol 0mg 0%
Sodium 310mg 13%
Potassium 460mg 13%
Total Carbohydrate 33g 11%
Dietary Fiber 8g 32%
Sugar 18g
Protein 15g 30%
Nutrition Facts
Serving Size 1 Rounded Scoop (31.5g)
Servings per Container 30
Amount Per Serving
Calories 120 Calories from Fat 15
% Daily Value
Total Fat 1.5g 2%
Saturated Fat 1g _5%
Trans Fat 0g
Cholesterol 0mg 0%
Sodium 330mg 4%
Total Carbohydrate 2g 1%
Sugars 0g
Protein 25g 60%
NUTRITION FACTS
Serving Size: 1 bottle (11.5 oz.)
Servings per Container: 4
Amount Per Serving
Calories 180 Calories from Fat 70
% Daily Value
Total Fat 8g 12%
Saturated Fat 1g 5%
Trans
Fat 0g
Cholesterol 10mg 3%
Sodium 300mg 13%
Potassium 310mg 9%
Total Carbohydrate 14g 5%
Dietary Fiber 3g 12%
Sugar 6g
Protein 15g 30%
Nutrition Facts
Serving Size 1 Shake (11 fl oz.)
Servings per Container
Amount Per Serving
Calories 160 Calories from Fat 25
% Daily Value
Total Fat 3g
5%
Saturated Fat 0g
5%
Trans
Fat 0g
Cholesterol 25mg 8%
Sodium 270mg 11%
Potassium 310mg 9%
Total Carbohydrate 4g 1%
Dietary Fiber 1g 4%
Sugar 1g
Protein 30g 60%

78
Protein Drinks & Powders Brands
Note: the calories, grams of protein and sugar may be slightly different depending on the flavor of each
protein shake or powder. Make sure to read the label.
Brand
Calorie
s
Protei
n
grams
Suga
r
gram
Where to buy
Premier Protein
160 30 1
Amazon, Costco, Target
Pure Protein
170 35 1
Amazon, Walmart, Walgreens
Optimum Nutrition
120 24 2
Amazon, Costco, GNC,
Vitamin Shoppe
EAS 100% Pure Whey
Protein Powder
160 30 2
Amazon, Walmart, Target
Muscle Milk Lite
100 20 0
Amazon, Sam’s Club
Bob's Red Mill All Natural
Whey Protein Concentrate
80 15 1
Amazon, local grocery stores
Quest Nutrition Protein
Powder
100 20 0
Amazon, GNC
Lactose-Free (whey protein isolate)
Brand
Calorie
s
Protei
n
grams
Suga
r
gram
Where to buy
Bariatric Advantage
160 27 0.5
BariatricAdvantage.com
Unjury
100 21 3
Unjury.com
Beneprotein (1 scoop)
120 24 2
Amazon, Walmart
Isopure Zero Carb
Powder (1 scoop)
160 30 2
Amazon, GNC, Vitamin Shoppe
Isopure Zero Carb
Ready-to-Drink
100 20 0
Amazon, GNC, Vitamin Shoppe
Syntrax Nectar
80 15 1
Amazon, Vitamin Shoppe

79
Soy Protein Powders
Brand
Calories
Protei
n
gram
Sugar
grams
Where to buy
Bob's Red Mill Gluten Free
Soy Protein Powder
80 17 0
Amazon, local grocery stores
Trader Darwin's Soy
Protein Powder
110 23 0
Amazon, Trader Joes
Jarrow Formulas Iso-
Rich Soy
110 25 0
Amazon, GNC, Vitacost
Egg white Protein Powders
Brand
Calorie
s
Protein
grams
Sugar
grams
Where to buy
MRM Egg White Protein
Powder
110 25 0
Amazon, Vitamin Shoppe
Jay Robb - Egg White
Protein Powder
115 24 0
Amazon, Vitamin Shoppe,
jayrobb.com
Now Foods Egg white
Protein
100 20 1.5
Amazon, iherb.com
PaleoPro Protein Powder
127 23 0
Amazon
Plant-based, Organic Protein Options
Brand
Calorie
s
Protein
grams
Sugar
grams
Where to buy
Nutiva Organic Hemp
Protein Powder
90 15 1
Amazon, Costco, Target,
Vitamin Shoppe
Bob’s Red Mill Hemp
Protein Powder
120 14 1
Amazon, local grocery stores
Bob's Red Mill Protein &
Fiber Nutritional Booster
160 20 1
Amazon, local grocery stores
Bob's Red Mill Vanilla
Protein Powder
Nutritional Booster
180
20
3
Amazon, local grocery stores
Orgain Organic Protein
150 21 1
Amazon, Costco, Target
Unjury Planted True
120 20 3
Unjury.com
Note: plant based protein powders have a tendency to be a bit chalky or grainy. Make sure the return
policy before buying, in case you do not like it.

80
Enhancing the Full Liquid Diet
1. Your tastes may change after surgery so have a variety of different brands of shakes &
powders on hand to ensure you have several to choose from after surgery.
2. Buy “base” flavors that can be flavored to increase variety: of vanilla, chocolate, unflavored
protein powders and chicken soup.
3. Buy different flavors of sugar free syrups to add to your protein shakes and nonfat, plain
yogurt. Sugar free DaVinci and Torani brands are both sweetened with sucralose (Splenda)
and Cash & Carry stores have a wide selection for a lower price than regular grocery stores.
4. Stock up on herbs and spices to flavor broths and low fat cream soups. There are many blends
already for you to use: Italian, taco, Creole seasonings. Mild curry powder, thyme, basil,
rosemary, cumin, etc.
For the first 2 months avoid any spicy seasonings like cayenne pepper, Tabasco or hot
sauce; it’s too hard on the pouch.
For protein shakes and powders:
o Vanilla + SF caramel
o Vanilla + SF white chocolate mocha
o Vanilla + SF orange = “creamsicle”
o Vanilla + SF pumpkin spice
o Chocolate + SF raspberry
o Chocolate + SF coconut
o Chocolate + PB 2 = “chocolate peanut butter cup”
o Chocolate + SF peppermint
For soups or broths:
o NF plain Greek yogurt + strained low-fat cream of chicken soup + taco seasoning
o NF plain Greek yogurt + butternut squash soup + mild curry powder
o Unflavored protein powder + chicken broth + Creole seasoning
o Unflavored protein powder + strained low-fat cream of mushroom soup
o High protein chicken soup + thyme and rosemary
Be very careful with soups available in the deli section at grocery stores; many are high fat and
sugar. Be sure to read the label before buying to determine if it meets you needs.
Remember: the post op diet progression (Stages 1 – 5) lasts approximately 2 months.
During this time it’s important to adhere to the prescribed diets (full liquid, pureed, and soft
foods) to ensure proper nutrition, promote healing, and reduce chances of dumping
syndrome or complications.

81
Yogurt
Yogurt is a very healthy protein option depending on the individual and type of yogurt you eat.
There are many yogurts with high protein and low sugar and there is just as many with high sugar
and low protein. You will need to read the labels carefully to determine if the yogurt meets your
nutritional needs.
Yogurt label reading guideline:
• Look for high protein, low sugar, and low calorie.
• Keep sugar grams <7 grams to avoid dumping.
• Try buying plain, nonfat yogurts and adding flavored protein powder or sugar free syrups to
flavor them.
Recommended Yogurts
Yogurt
Calories
Protein
Sugar
Dannon Oikos Nonfat Plain Greek
80 15 6
Chobani Nonfat Greek
80 15 4
Stonyfield Organic Greek, Nonfat, Plain
80 15 6
Siggi’s 0% Nonfat Plain
80 15 4
Fage Total 0% Plain Greek
100 18 7
Nancy’s Nonfat Plain Greek
120 22 7
Carb Master (Kroeger) -
average all flavors
80 12 3
Dannon Activia Greek Light Vanilla
Nonfat
80 13 6
Yoplait Greek 100 Vanilla
100 13 6
Dannon Light & Fit Nonfat Greek -
average all flavors
120 15 7
Dannon Oikos Triple Zero -
average all flavors
120 15 7

82
Separate your fluids from your meals but you do not have to wait 60 minutes before drinking again.
Meals include protein shakes, yogurt, and soups or broths with protein powder added.
Time
Food or beverage
(20 minutes for meals)
Protein
grams
Calorie
s
Time
(minutes)
Notes
8:00 am 3 oz. Premier protein shake
1 calcium citrate chewy bite
8
44
15
22
1 svg. calcium
8:25 am 10 oz. water
0 0 60
10:00 am
3 oz Fage Total Fat 0% plain
Greek yogurt, w/SF peach
syrup
9 50 18
Walked around block 5
minutes
10:30 am
6 oz. Propel Lemon water
0 0 50
12:00 pm
4 oz. Unjury Chicken soup
protein shake with curry powder
(1/2 packet)
1 calcium citrate chewy bite
11
0
45
15
Tasted good.
1 svg. calcium
12:40 pm
8 oz. water with lime juice
0 0 1 hour Walked around house
2:10 pm 4 oz Vitamin Water Zero -
orange
0 0 30
3:00 pm 4 oz vanilla protein shake with
SF raspberry flavored syrup
2 chewable multivitamin w/iron
1 chewable probiotic
1 Vitamin B12. 500 mcg
11
0
60
35
45 Napped 30 minutes
1 svg Multivitamin
1 svg probiotic
1 svg Vit B12
5:15 pm ¼ cup cream of mushroom
soup (strained) with ¼ scoop
Unjury unflavored protein
powder
1 c
alcium citrate chewy bite
1
5
40
25
15
18
Walked around house
1 svg. calcium
7:00 pm 8 oz. lemon zinger tea
0 0 30
Totals Total fluids: 52 oz.
Exercised: 10 minutes
Vits/Supps: all in
45
grams
344
calories
Meals: ~20
minutes
Stage 2 - FULL LIQUID
SAMPLE Meal Plan

83
TIPS
If foods feels ‘stuck” do not try to push it down by swallowing fluids
as drinking fluids will cause more discomfort and possibly
regurgitation. Instead get up and walk around.
Consuming smaller servings of protein at each meal is metabolically more
effective than all at once.
Make sure to measure the amount of protein shakes and fluids you are taking in to ensure you
are properly hydrated and receiving enough protein grams.
Plan ahead and have the protein drinks ready to drink.
Use a thermos or chill your glasses in the freezer to keep your protein drinks cool while you
are drinking them.
Water: some patients find that water tastes “funny,” have a metallic taste, or even be painful to
drink. This is usually temporary but can be remedied by adding in some flavoring (i.e. squeeze of
lemon, stevia, or Mio drops).
Often patients are sensitive to the temperature of fluids after surgery; hot or cold may be
less tolerable. If this happens, experiment with the temperature of your fluids until you find
what works best for you.
It is very important to stay hydrated; sip fluids throughout the day. If you are well
hydrated, your urine should be light yellow.
Set a timer throughout the day to help you remember to have a meal.
Set a time for 20 minutes at meal time to keep you from drinking too fast.
AVOID
Do not force yourself to finish fluids if you feel full.
Sugar-free Jell-O, puddings and popsicles contain aspartame (NutraSweet) are not
recommended. It you choose to eat them, they DO NOT count as a meal since they have
no or little nutritional value
Avoid gulping, straws, or drinking too fast; it introduces air into your system and may
cause gas pains.
Fruit or vegetables juices.
Milk, soy milk, almond milk, coconut milk, etc. They contain little to no protein.
Carbonated beverages, caffeine, sweet beverages, sugar.
Oatmeal or cream of wheat
Ice cream, sorbets, or frozen desserts of any kind.
84
Duration: 3 weeks
GOALS
Transition from full liquid to pureed to allow your stomach to adjust to semi-solid solid
protein/food. Follow the prescribed diet to help prevent dumping syndrome or blocking your
stomach pouch opening.
Protein: 40 - 50+ grams/day; more if tolerated.
Carbohydrates: after a few days of becoming comfortable with proteins you can tolerate, fruits and
vegetables can be introduced. No stringy, fibrous or raw vegetables. Also avoid fruits with skins,
seeds or membranes that could potentially “get stuck.”
Calories: average 300 - 500+ calories/day. If you take in more protein grams, your calories will
increase accordingly.
Number of meals: 3 + 1-2 snacks as needed. Establish regular meal times and never go longer
than 4 - 5 waking hours without eating. Even if you are not hungry you should take a few bites of
food to stay on your eating schedule.
Length of meals: meals should take a full 20 - 30 minutes to finish. Continue to drink/eat slowly
with dime-sized bites and sips.
Mindfulness: eat or drink very slowly; taking small, dime-sized bites or sips. Listen to your body
to determine the amount you can consume in the 20 - 30 minute period; checking in often to
determine your last sip/bite “threshold.”
Total fluids: 40 - 50+ oz. /day; more if tolerated. Aim for 4-6 ounces per hour to meet this goal.
Continue drinking water, herbal tea, broth, flavored waters, etc. Sip throughout the day and avoid
gulping. Protein shakes no longer count toward your total fluids.
Separate fluids from meals: stop drinking 15 minutes prior to your meal or snack, spend 20 - 30
minutes on your meal and wait 60 minutes after your meal before resuming fluids.
Separating fluids from meals & snacks is a lifetime habit.
Food records: continue tracking time of day, food, amount (oz., cup, Tbsp.), protein grams, calories,
total amount and type of fluids, list of vitamins, exercise (type and minutes), and any challenges,
symptoms or questions.
(continued on next page)
STAGE 3 - PUREED DIET

85
Vitamins/Supplements: daily vitamins & supplements (liquid or chewable) Separate the
multivitamin with iron and calcium citrate by 2 hours.
NO GUMMY SUPPLEMENTS OF ANY KIND.
Vitamins /
Minerals
Gastric Bypass Sleeve Gastrectomy
Multivitamin with iron
(chewable or liquid)
1 svg/day 1 svg/day
Calcium Citrate with Vitamin
D3 (chewable or liquid)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
Probiotic 1 svg daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA
Exercise: 20 minutes of daily activity; incrementally increases every week until you are doing
30 - 45 minutes per day, 5 - 7 days a week. When exercising, listen to your body. If you feel as if
you are pushing yourself, stop!

86
ALL FOODS MUST BE PUREED.
• ALL FOODS need to be pureed to the consistency of applesauce; smooth with no chunks
• Your stomach is still healing and solids foods can cause dumping syndrome or pain.
• Start slowly; with about 1/4 - 1/3 cup of food.
• Listen to your body and stop when full.
• Remember to take dime-sized bites and sips to prevent eating too fast or too much.
• If you take a few bites of food and it doesn’t feel right, stop eating. Your pouch may not
be ready for it yet.
Meat, Fish, Poultry
•
Chicken - dark meat is better tolerated (no skin)
•
Shrimp, scallops or fish
•
Canned chicken, tuna or salmon packed in water
•
Deli meat of turkey, lean ham or lean roast beef
•
PB2 - powdered peanut butter (local grocery store or Amazon)
•
Tofu
Eggs, Cheese, Dairy
•
Nonfat or low-fat Yogurts: sugar-free, plain Greek yogurt or regular yogurt
•
Eggs, egg whites or egg beaters
•
Cottage cheese, non-fat or low- fat
•
Ricotta Cheese, non-fat or low-fat
•
Laughing Cow cheese wedges (no hard cheese during this stage)
Soups (with protein added)
•
Low-fat cream soups made with skim milk
•
Black bean, lentil, split pea
•
Mild chili
•
Tomato, butternut squash, carrot
•
Chicken or beef flavored protein powders/soups
Fruits/Vegetables: 1 - 2 dime sized bites.
•
Fruits: no skins, membranes or seeds.
•
Vegetables: no raw, fibrous, stringy or leafy green vegetables for the first two months post
op; they are too hard on your pouch.
•
Vegetables must be cooked & pureed.
Pureed Meal Ideas
• Use broth, milk or water to puree with your meats/proteins.
• Pulse the food in the blender until desired consistency of applesauce is achieved.
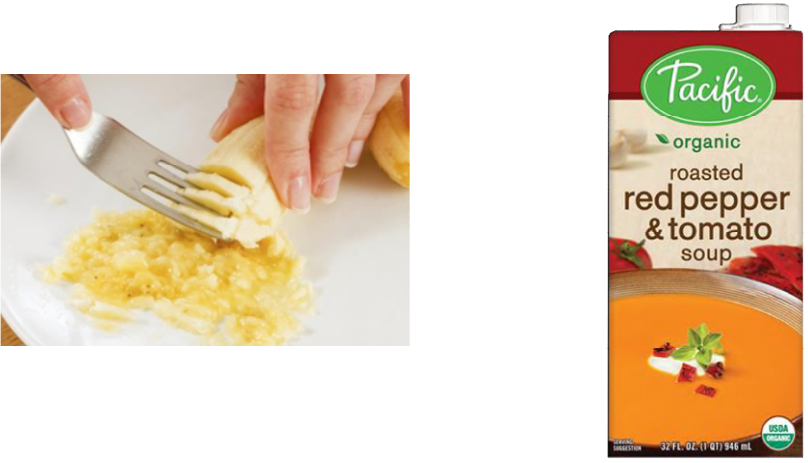
87
Meat, Fish, Poultry
• Chicken thigh with seasoning (Taco, Italian, chili powder)
• Canned tuna mixed with cottage cheese and dill weed
• Shrimp with cocktail sauce
• Chicken thigh with PB2, cilantro, and coconut water (Thai chicken)
Eggs, Cheese, Dairy
• Soft scrambled eggs with pico de gallo (liquid only)
• Laughing cow cheese with deli ham & gourmet mustard
• Nonfat plain Greek yogurt with mashed peaches (no skin)
• Cottage cheese/bleu cheese recipe and chicken
• Fat free refried beans with cottage cheese
Soups (with protein added)
• Wendy’s chili with cottage cheese
• Butternut squash soup with non-fat plain Greek yogurt and Creole seasoning
• Low fat mushroom soup with unflavored protein powder
• Soups and legumes are primarily a carbohydrate source. Make sure to puree them with
unflavored protein powder, cottage cheese, or tofu to ensure you are taking in protein.
• No broth-based soups or soups with noodles, rice, or other grains.
Fruits/Vegetables
• Mashed melons, bananas, pears, peaches, nectarines (no skin)
• Cooked & pureed sweet potatoes, butternut squash, carrots, broccoli, cauliflower.

88
Cottage Cheese Recipes (Stage 3 and Beyond)
Blue cheese dip/dressing
• 1 pint nonfat or low fat (1%) cottage cheese
• 1 ½ oz. blue cheese
• 1-3 cloves of garlic- to taste
• Splash of Worcestershire sauce - to taste
• Salt & pepper – to taste
• Nonfat milk
Place all of ingredients in blender or food processor.
Add enough milk to your desired consistency.
It can be used as dip, sauce or dressing.
For ¼ cup*
65 calories
8 protein grams
*based on 1% fat cottage cheese
Ranch dip/dressing
• 1 pint nonfat or low fat (1%) cottage cheese
• 1 packet Uncle Dan’s Ranch
• Nonfat milk
Place all of ingredients in blender or food processor.
Add enough milk to your desired consistency. It can be used as dip, sauce or dressing.
For ¼ cup*
45 calories
7 protein grams
*based on 1% fat cottage cheese
* If using Hidden Valley seasoning packet it is 65 calories for ¼ cup.
Note: you could also substitute the cottage cheese with nonfat plain Greek yogurt, light ricotta cheese
or tofu; though cottage cheese will provide the best calorie to protein ratio and cheesy flavor.

89
•
Stop drinking fluids 15 minutes before your meal/snack and wait 60 minutes after to resume drinking.
•
Protein shakes no longer count toward your total fluids intake.
Time
Food or Beverage
(20 minutes for meals)
Protein
grams
Calorie
s
Time
(minutes)
Notes
7:30 am 1 large scrambled egg with liquid
from pico de gallo
1 bite peach, no skin
1 calcium citrate chewy bite,
500 mg
6
0
-
71
3
15
22
1 svg calcium
9:00 am 8 oz. peppermint tea 0 0 30
10:00 am 12 oz. water - Mio drops 0 0 50
11:20 am
¼ c. tomato soup with
¼ c. cottage cheese
1 calcium citrate chewy bite,
500 mg
1
7
-
45
10
15
20
Walked 10 minutes
1 svg calcium
1:00 pm 16 oz. water 0 0 2 hours
3:00 pm 4.5 oz. chocolate protein shake
over ice
1 multivitamin with iron
1 chewable probiotic
1 vitamin B12, 500 mcg
15
-
-
-
80
35
0
0
15
1 svg Multivitamin
1 svg probiotic
1 svg Vit B12
4:30 pm 12 oz. licorice spice tea 0 0 Walked 10 minutes
6:00 pm 2 oz. chicken thigh
2 tbsp. sweet potatoes
splash of chicken broth
1 calcium citrate chewy bite,
500 mg
14
0
96
10
15
23
1 svg calcium
7:20 pm 6 oz. water with lemon 0 0 20
Totals Total fluids: 54 oz.
Exercised: 20 minutes
Vits/Supps: all in
43
grams
395
calories
Meal time
20
minutes
Stage 3 - PUREED
SAMPLE Meal Plan

90
TIPS
• If foods feels ‘stuck” do not try to push it down by swallowing
fluids as drinking fluids will cause more discomfort and possibly
regurgitation. Instead get up and walk around.
• Eat slowly; use 10 minutes per ounce as a guideline & a full 20
minutes to complete a meal. Practice mindful eating. Breathe after every
bite.
• Puree meats/proteins with broth, milk or water in blender; pulse until the
consistency of applesauce is achieved.
• Add non-fat powdered milk or acceptable protein powders to your foods to boost protein amount.
• Use herbs and spices to flavor the proteins/meats.
• Try one new food at a time.
• Eating or drinking too fast can cause nausea, vomiting, or pain.
• Stop eating if you experience any nausea or vomiting.
• If you feel nauseated or experience gas or bloating after eating, then you are not ready for this
food. Wait a few days before trying this food again.
• Listen to your body. Stop when you feel full.
• Portions may need to be adjusted depending on your individual tolerance. 2-3 bites of food may
be all that you can tolerate initially.
• Gradually increase quantity as tolerated.
• Be very careful with soups available in the deli section at grocery stores; many are high fat and
sugar. Be sure to read the label before buying to determine if it meets you needs.
• Eat animal proteins/meats as your main protein sources; and protein shakes and powders to
supplement your daily intake.
• You will most likely only be able to eat 1-2 bites of fruits and vegetables since you are eating
your protein first. You will be able to eat more in time.
• If you are feeling constipated, making sure you are drinking enough water and walking helps. If
you need more help, try Miralax, a stool softener or add some Benefiber to your foods. Section 8
has more information on constipation.
AVOID
• No baby food; it does not meet the nutritional needs of adults.
• No hard cheese.
• Avoid pasta, rice, bread, crackers, pastries, ice cream, candy and other similar foods.
• Extreme temperatures may cause dumping syndrome.
• Do not chew gum or suck on hard candy. If swallowed, it can obstruct your outlet.
Helpful
Tips

91
Duration: 2 weeks
GOALS
The Stage 4 Soft Foods diet begins approximately 5-7 weeks post-surgery; depending on your
procedure. While your foods no longer need to be pureed, you still want to focus on moist and tender
foods. Make a special effort to ensure that you chew all foods thoroughly. At this point, you’re starting to
move toward a more regular diet that should include a variety of foods and good sources of protein at
every meal.
Soft solids are gradually re-introduced to your system and will be more filling. Start to move away from
soft, mushy foods and liquid protein, as these types of foods will be less filling over time.
• Protein: 50 - 60+ grams/day; more if tolerated. Always eat protein first and at every meal.
• Calories: 400 - 600+ calories/day. Choose high protein sources first, followed by vegetables,
fruits, and legumes.
• Number of meals: 3 + 1-2 snack(s). Eat at regular meal times. Never go longer than 4 - 5
waking hours without eating.
• Length of meals: continue to eat slowly. Meals should take a full 20 -30 minutes to finish. Slow,
mindful eating helps you determine your last bite threshold, avoid overeating and dumping.
• Mindfulness: eat or drink very slowly; taking small, dime-sized bites or sips. Listen to your
body to determine the amount you can consume in the 20 - 30 minute period; checking in often
to determine your last sip/bite “threshold.” This is a critical time to be mindful as your food looks
normal again (not liquid or pureed). It’s easy to fall into old habits of eating too fast when foods
look normal.
• Total fluids: 56 - 64+ oz. /day. Non-caloric, non-carbonated, non-caffeinated beverages.
STAGE 4 – SOFT FOOD

92
• Separate fluids from meals: stop drinking 15 minutes prior to your meal or snack, spend 20-30
minutes on your meal and wait 60 minutes after your meal before resuming fluids. Separating
fluids from meals/snacks is a lifetime habit
• Food Records: track time of day, food, amount, protein grams/ounces, calories, total and types
of fluids, list of vitamins, exercise (activity, minutes), and any challenges or symptoms.
• Vitamins/Supplements: continue with liquid or chewable; take daily. Separate the multivitamin
with iron and calcium citrate by 2 hours. NO GUMMY SUPPLEMENTS OF ANY KIND.
Vitamins/Minerals Gastric Bypass
Sleeve
Gastrectomy
Multivitamin with iron:
(chewable or liquid)
1 svg/day 1 svg/day
Calcium Citrate with Vitamin D3
(chewable or liquid)
500 - 600 mg svg,
3x/day
(1500 - 2000 mg day)
500 - 600 mg svg,
3x/day
(1500 - 2000 mg day)
Probiotic 1 svg daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA
• Exercise: daily physical activity. Aim for 20-30 minutes a day. Increase as tolerated.
Slow down
Eat with care

93
Meats
•
Meats should be soft and moist enough to swallow without “sticking.”
•
Marinated meats, boiled meats and the dark meat of chicken
tend to be well tolerated.
•
Fibrous meats such as dry turkey, chicken breast, or steak can be
difficult to digest.
•
Microwaving and grilling dries out meats, making them difficult
to tolerate.
•
Meats can dry out in the refrigerator so add some water or
chicken broth before microwaving to make the meat juicier.
•
A crock pot can be very helpful in keeping meats moist.
•
Do not fry your meats; it adds calories, can make foods hard to digest, and cause
dumping.
•
Weigh food on a scale to ensure you are getting adequate protein. If you do not own a food
scale, cook a piece of protein the size of a deck of cards.
Fruits and vegetables
• Vegetables need to be soft and well-cooked in the first 4-6 weeks.
• Avoid fibrous vegetables such as celery, cucumbers, corn, pea pods.
• No raw vegetables or salads while progressing through the 5 stages (the first 2-3 months post
op).
• Frozen fruits and canned fruits (packed in their own juice and drained) are well tolerated
as well as thawed frozen fruit.
• Avoid membranes of oranges, tangerines and grapefruit.
• Avoid cores, skins and seeds of fruits, such as apples, grapes, berries, and tomatoes.
TIPS
•
If foods feels ‘stuck” do not try to push it down by swallowing fluids
as drinking fluids will cause more discomfort and possibly
regurgitation. Instead get up and walk around.
•
Stop eating as soon as you know the next bite is too much.
•
Meats: You no longer need to puree your meat, but you should still trim any
visible fat and remove all of the skin from poultry. You should continue to
bake, broil, or steam your meats.
•
Cheese: have soft cheeses.
•
Introduce one food at a time to determine if tolerated.
•
Try new proteins on the weekends or in the evenings when you are home, just in case it’s not well
tolerated yet.
•
If you are unable to eat enough of the protein requirements, you can supplement with protein
shakes or powders. You may find that the protein shakes will be less filling over time.
•
Not everyone will be able to eat all of the recommended foods, especially at first.
•
Learn your body’s fullness cues and do not overstuff your pouch or sleeve.
•
If you are not hungry, you still need to fuel your body: take a few bites of protein to stay on
schedule.
•
Baby warmer trays or warming plates can be used to keep food warm while you are (slowly) eating
your meal.
Helpful
Tips

94
•
If dining out and the entrée is the typical portion, plan on bringing most of the meal home in a “to-go”
container.
•
Continue your food records. Write down all of the food you eat and the fluid you drink. Food records
are critical to ensure that you are eating enough protein.
•
It’s important to eat the recommended dietary protein your body needs.
•
Do not skip meals. Stay on an eating schedule; never going longer than 4 - 5 waking hours without
food.
AVOID:
• All processed carbohydrates, baked products, and grains, starchy foods such as breads,
noodles, crackers, rice, cakes and bagels. They expand in your stomach and may cause pain
or blockage. They can also be easy to overeat
• No potted meats. They are high in fat and low in protein.
• Fatty and fried foods, dry foods, high sugar, grains and refined carbs (bread, crackers, rice,
cookies, etc.). They can cause dumping and have you relapse into unhealthy eating habits from
the past.
• Popcorn and nuts.
• Grazing or nibbling. This will lead to weight gain.
• Do not eat coconut flakes/bits – they can easily create a blockage.
• Trying any new proteins or foods at work, restaurants, or outings. Unknown food preparations
are risky. It may lead to dumping.
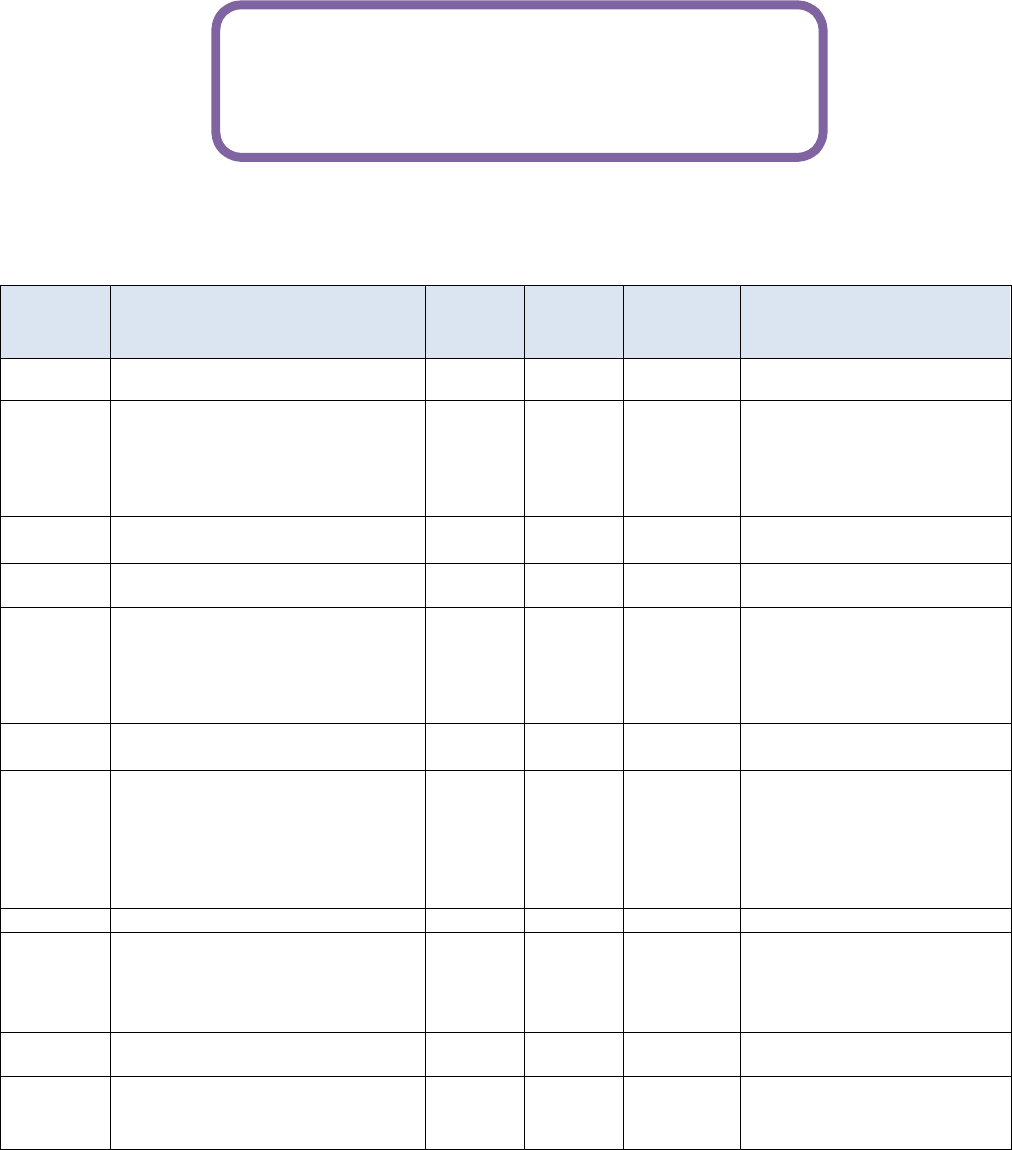
95
• Remember to separate your fluids from your meals & snacks. Stop drinking 15 minutes prior
to meal and then wait 60 minutes after meal before drinking again.
• Protein shakes no longer count toward your total fluids intake.
Time
Food or beverage
(20 minutes for meals)
Protein
grams
Calorie
s
Time
(minutes)
Notes
6:10 am 4 oz. water 0 0 20
7:15 am ½ large egg
1 chicken sausage link (sweet
Italian)
1 calcium citrate chewy bite
3
11
35
100
15
22 Couldn’t finish egg, liked
the chicken sausage
1 svg. calcium
8:30 am 8 oz. chamomile tea with lemon
& stevia
0 0 60 walked on break 10
minutes
10:00 am
16.9 oz. Propel water 0 0 45
11:30 am
2 oz. deli turkey
1 oz LF string cheese
1 Tbsp mustard
1 calcium citrate chewy bite
10
7
0
60
85
10
15
18
walked at lunch 15
minutes
1 svg. calcium
1:00 pm 16 oz. water with stevia water
drops
0 0 1 hour
3:30 pm ½ protein shake (4.5 oz)
2 chewable multivitamin w/iron
1 chewable probiotic
1 Vitamin B12, 500 mcg
15
80
35
15
1 svg. multivitamin
1 sv.g probiotic
1 svg. Vit B12
5:15 pm 10 oz. water 0 0 30
6:00 pm 2 oz. garlic chicken
½ cup mushrooms
1 calcium citrate chewy bite
14
1.5
96
22
15
25
1 svg. calcium
7:20 pm 4 oz. water 0 0 30
Totals
Total fluids: 59 oz.
Exercised: 15 minutes
Vits/Supps: all in
63.5
grams
455
calories
Meals: 20
minutes
Stage 4 - SOFT FOOD
SAMPLE Meal Plan

96
Duration: Lifetime
GOALS
Months 2 – 6: learn what proteins and complex carbohydrates you can tolerate; continuing to try new
foods. Reinforce new eating and drinking habits. Create new foods, meals and menus that reflect foods
you tolerate well and enjoy. Reinforce the healthy habits needed to lose the weight and keep it off.
Month 6 – lifetime: you should be hitting your stride with your new eating and health habits. If your
weight loss has stalled, make sure you are keep food records and following the program guidelines.
• Bariatric diet: is much like the Paleo diet. Always eat lean proteins first and then complex
carbohydrates coming from veggies, fruits and legumes.
• Protein: 60 - 80+ grams/day. Protein first - always! Continue to slowly introduce new, lean
proteins into your diet to allow your stomach to adjust, provide variety, and overall enjoyment.
• Calories: 500 - 800+ calories/day for as long as you can. Over time your calories will increase
naturally as you heal and are able to tolerate a wider variety of foods and eat larger amounts.
• Be aware that weight loss often stops when calories consistently exceed 1000-1200 for women
and 1400-1600 for men. Stay <1000, and even better, under 800 calories per day with your
protein grams a minimum of 60+/day for continued weight loss, for as long as you can.
• Number of calories to maintain weight: the caloric intake you can consume and maintain your
weight will depend on many variables but a key factor is the amount and types of exercise you
integrate into your daily life.
• Number of meals: 3 + 1-2 snack(s), as needed. Eat at regular meal times. Never go longer than
4 - 5 waking hours without eating. Eat away from distraction (desk, TV). Planning and preparing
your meals is essential to ensure you meet your nutritional needs and avoid problem foods.
• Length of meals: meals should take a full 20 minutes to finish but no more than 30 minutes.
• Mindfulness: eat or drink very slowly. You may be able to take slightly bigger bites and sips at
this point but always be mindful when eating or drinking. Listen to your body to determine your last
sip/bite “threshold.”
• Total fluids: 64+ oz. /day. Non-caloric, non-carbonated, non-caffeinated beverages. No straws.
Caffeine: you may introduce coffee/tea back in your diet; limit to one cup a day. Decaf is
preferred. Avoid high fat/sugar creamers. You may be able to take bigger sips but avoid gulping.
• Separate Fluids from Meals: you may drink up to your meals now but always separate your
Stage 5 – BARIATRIC
Long Term

97
fluids from your meals/snacks and wait 60 minutes after eating before resuming fluids.
• Food Records: keep daily. Records keep you on track and help you find the foods that work best
in your body. Remember that success leaves clues. Discover your secrets to success.
Food records:
o Determine if you are meeting your nutritional needs.
o Pin point the proteins/foods your new stomach tolerates well and the ones that cause
problems/distress.
o Show you how certain foods affect your energy level, fullness, and even moods.
o Identify emotional or situational triggers.
o Stay out of denial. Stop fooling yourself with the idea that “If I don’t write it down, it didn’t
happen.” Your body always counts calories.
o Create menus and meal plans. When stuck in a “food rut” you can review your records and
find some favorites you’ve forgotten.
o Give you immediate feedback on how your choices help or hinder your progress.
o Identify and celebrate your milestones.
The Essentials Advanced
time of day hunger and fullness levels: before & after meal
food item(s) and amount (oz., Tbsp., cup) mood/feelings (happy, bored, depressed)
protein grams location of meal (work desk, in front of TV, car)
calories who you dine with (alone, coworker, family)
fluids – type & ounces post op: challenges, nausea, vomiting, or pain
list of vitamins & supplements taken food intolerances
exercise - type and minutes foods well tolerated, filling, & satisfying
Websites/Phone Apps:
www.baritastic.com
www.supertracker.usda.gov
www.CalorieKing.com
www.MyFitnessPal.com
www.FitDay.com
www.LoseIt.com
www.SparkPeople.com

98
• Vitamins and Supplements: take daily. If you are comfortable, you can switch to regular tablet
vitamins though be aware of dosages. Calcium citrate is always 2 large pills for one dose.
Separate the multivitamin with iron and calcium citrate by 2 hours. NO GUMMY
SUPPLEMENTS OF ANY KIND.
Taking the bariatric supplements daily is a lifetime commitment to ensure optimal heath and
prevent any deficiencies.
Vitamins/Minerals Gastric Bypass Sleeve Gastrectomy
Multivitamin with iron (chewable
or liquid)
1 svg/day 1 svg/day
Calcium Citrate with Vitamin D3
(chewable or liquid)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
Probiotic 1 svgs daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA
Exercise: 30 - 45 minutes a day, 5 - 7 days a week and work up to a total of 300 minutes of exercise per
week. After 2 months post op, add in strength training, at least 90 minutes per week. Additionally,
stretching and balance training helps improve performance of everyday activities and assists with posture,
minimizing stress and maximizes the strength of all joint movements.
o Strength training helps to preserve and build muscle mass. The more muscle you have,
the more calories you burn.
o Stretching keeps you limber and can help prevent injuries.
TIPS
•
The bariatric diet is much like a paleo diet: lean meats with complex carbohydrates (i.e. vegetables,
fruits & legumes) that provide volume, satiety, and gradually empty from your stomach.
•
Integrate and reinforce the healthy habits that will keep healthy and maintaining your weight.
•
Vegetables: You should now focus on eating high-fiber vegetables. Avoid vegetables like beets,
carrots, and onions.
•
Fruits: you should focus on eating more of those fruits, including avocados, berries, cantaloupe, and
citrus fruits.
•
Make a list of the proteins and fruits and vegetables you tolerate well and post it to refer to often.
•
Create a menu of meals that you enjoy to make meal planning and shopping easier for you.
•
The first 3 months post op were a time for healing, allowing your new stomach to adjust to foods and
establishing new eating/drinking habits required of a bariatric patent.
•
From 3 – 6 months after surgery, you are reinforcing the healthy habits needed to lose the weight
and keep it off.
•
Remember that obesity treatment is a lifelong process. The habits you build and maintain will
determine your level of success.

99
Time Food or beverage
(20 minutes for meals)
Protein
grams
Calorie
s
Time
(minutes)
Challenges/Notes
7:30 am ¾ c. cottage cheese
2 Tbsp. blueberries
1 calcium citrate chewy bite
21
0
145
10
15
18
1 svg calcium
8:50 am 12 oz decaf coffee with
Splenda
0 0 30
11:00
am
16.9 oz. Vitamin Water Zero 0 0 75
12:00
pm
3 oz. salmon
1 cup spinach
¼ cup cucumber & tomato
2 Tbsp balsamic vinegar
1 calcium citrate chewy bite
21
1
1
0
123
7
17
28
15
25
Walked 20 minutes at
lunch
1 svg calcium
1:30 pm 16.9 oz. bottle Vitamin Water
Zero
0 0 1 hour
3:30 pm 1 oz string cheese
5 grapes
2 chewable Multivitamin
w/iron
1 chewable Probiotic
500 mcg Vitamin B12
7
0
90
15
35
17
1 svg. multivitamin
1 sv.g probiotic
1 svg. Vit B12
5:00 pm 12 oz water infused with
pineapple & mint
0 0 40
6:00 pm 3 oz. herbed pork loin
2 oz sweet potato
1 calcium citrate chewy bite
24
0
120
55
15
25
1 svg calcium
7:30 pm 4 oz. water with Mio drops 0 0 30 Strength training, 30
minutes
Totals Total fluids: 62 oz.
Exercised: 50 minutes
Vits/Supps: all in
75
grams
690
calorie
s
Meals:
21
minutes
Stage 5 – Ongoing Bariatric
Diet - SAMPLE Meal Plan

100
Protein 101
Why Protein is Important
• Protein was named after a Greek work proteios, meaning “of prime importance.”
• It is undeniably the most important nutrient in the bariatric diet.
• Protein is a part of every cell in your in body and these proteins are continually being broken down
and replenished.
• Since the body doesn’t store protein for later use, eating enough high quality protein is required,
otherwise the body will suffer.
• When protein intake is insufficient, the body breaks down lean body mass to offset for poor
nutrition intake.
• While loss of lean body mass is inevitable after weight loss surgery due to low calorie intake, you
can minimize this by taking in sufficient high-quality protein daily.
Principle Roles of Protein in the Body
•
Protein assists in proper wound healing after bariatric surgery.
o It helps to build and repair body tissues including skin, muscle and major organs.
•
Protein helps your body burn fat instead of muscle for a
healthier weight loss.
o After bariatric surgery, your calorie intake is reduced
drastically.
o Unfortunately, the human body tends to preserve fat
stores while using lean muscle mass as energy before it
taps into fat stores for energy.
o When you take in sufficient protein every day, you will
spare and preserve your muscle tissue, which forces your
metabolism to utilize fat for its energy.
o This is often referred to as "protein sparing."
•
Protein supports your metabolism so you lose weight faster.
o The more muscle you have on your body, the higher your metabolism and the more
fat calories your body will burn, even while at rest.

101
•
Protein helps keep you fuller, longer.
o Clinical studies show that high-protein diets increase satiety and decrease hunger
compared with high-fat or high-carbohydrate diets.
o Right after surgery, the majority of patients will not be hungry and may have to be
reminded to eat on a regular schedule.
o Over time, hunger & appetite can return.
o Building a habit of eating protein first will keep you full for longer periods of time,
helping you resist the snacking/grazing temptation between meals.
•
Protein helps keep your hair, skin, and nails healthy.
•
Protein helps form hormones, enzymes, and immune system antibodies to help your
body function properly.
Protein Goals
• Protein needs vary with each individual based on their age,
sex, lean muscle mass, daily exercise, and overall health.
• Immediately after surgery the protein goal will range from
40 - 60 grams per day as you are adjusting to a small stomach and a new way of eating.
• Once you have transitioned to regular food, the goal is 60 - 80 grams of high quality protein daily.
Protein Shakes & Powders
• Protein shake and powders are heavily utilized in the immediate months post op to promote
wound healing and minimize loss of lean muscle mass.
• Liquid protein supplements such as shakes and powders are the easiest to take in right after
surgery. After the first 2-3 months you will incorporate traditional proteins and foods into your
diet.
• Many patients continue to use protein shake as a convenient source of protein and nutrition.
• They are great for a quick and easy breakfast, snack, or as a backup plan when running late and
have no time for a regular meal.
Liquid vs. Solid Proteins
• As you move into Stage 4 and beyond, you will incorporate more
solid proteins into your diet.
• Seek out sources with more “staying power,” that will keep you fuller
for longer periods of time. Liquid or soft forms, such as protein
shakes, yogurt, or cottage cheese, may not keep you satiated the
way a piece of chicken or eggs will.
102
For example:
o 4 ½ ounces of chicken and a Premier protein shake
both have 30 grams of protein.
o Yet the chicken will keep you fuller for a longer period of time than the liquid protein shake.
• These liquid and softer proteins are still great sources of protein; simply notice if they continue
to provide you with the fullness/satiety you want.
• You may need to add protein powder or other foods such as fruit to help fill you up.
Spacing of Your Proteins
• Since the body cannot absorb more than about 30 grams at once, you
will need to take in protein throughout the day, across multiple meals
or healthy snacks.
• Foods that are high in protein should always be eaten first during
meals, in case you feel full quickly and can’t finish your meal.
Proceed with Caution
• For many patients, beef, pork, lamb, and chicken breast can be particularly difficult to
digest; though chicken thigh is generally well tolerated.
• You may want to wait to introduce these proteins until at least 3 months after surgery.
• Try new proteins on the weekend or evenings in case they have a negative result.
• Be sure to choose tender cuts and avoid the higher fat (therefore higher calorie) selections.
Complete vs. Incomplete Proteins
• Proteins and amino acids are used for almost every metabolic process in the body.
• Amino acids are the building blocks of protein.
• For optimal health, there are nine essential amino acids we need from dietary sources.
• However, not all proteins are alike. As a bariatric patient your primary goal is to get high quality
protein sources in to meet your nutritional needs.
• Many people get confused as to what types of proteins they should eat and what is considered a
good protein source.
Complete proteins
Animal-based proteins are known as complete proteins because they contain all nine of the
essential amino acids your body needs to function properly.
• Beef
• Poultry
• Pork
• Seafood & Fish
• Eggs
• Dairy

103
Incomplete proteins
Plant-based proteins are considered to be incomplete proteins, as they lack one or more of the
essential amino acids that your body needs.
• Beans (i.e. pinto, kidney, garbanzo)
• Lentils & split pea
• Nuts & seeds
• Grains & rice
• Vegetables
Complimentary proteins
Plant-based proteins provide some of the amino acids but they need to be combined with other foods
(i.e. beans with rice, whole wheat toast with peanut butter) to make a complete protein; known as
complimentary proteins.
• After bariatric surgery this is not a good option. Here’s why: plant source proteins are naturally
higher in carbohydrates or fat and calories while lower in protein than their animal protein
counter parts.
For example:
Food Amount
Calorie
s
Protein
grams
Beans & Rice 1 cup 360 12
Peanut butter 1 level Tbsp. 95 4
Nonfat refried beans
1 cup 180 12
Walnuts 1 cup 840 20
Chicken 1 cup 230 30
• The bariatric diet is similar to a Paleo diet, consisting of mainly protein with carbohydrates coming
from vegetables and fruits and legumes.
• Carbohydrates such as rice, breads, crackers, noodles, and cereal need to be avoided post op.
• These carbs are not well tolerated after surgery as they can swell up in your stomach and can
cause pain and dumping syndrome.
• Also, the calories from these carbohydrates can add up quickly, push out protein rich foods, and
for many patients, make it easy to slip back into old unhealthy grazing habits.
• Therefore food combining to create a complete protein is not the best option.
• Eat complex carbohydrates such as vegetables, fruits, and legumes to maximize nutrition and
satiety.

104
Vegetarians
• Following a vegetarian diet is possible after bariatric surgery, though it does take more
effort and usually is accompanied with a higher caloric intake.
• Plant-based proteins, other than soy, need to be combined with other sources to meet
your nutritional needs and are naturally higher in carbohydrate and calories, and not
always well tolerated.
Soy
• This legume is the exception to the plant-based protein rule.
• Soy contains all the essential amino acids necessary for
proper nutrition and comes in a wide variety of products,
such as tofu, tempeh, and soybeans.
• Soybeans are 250 calories and 22 grams of protein per cup.
Lupini beans
• These legumes are one the highest sources of plant
proteins available, only second to soybeans, with
most of the essential amino acids.
• These beans have a firm texture and are typically
soaked in brine for a great salty snack.
• Lupini beans are 200 calories and 26 grams of
protein per cup.
Foods Commonly Perceived as High Protein
• Legumes, nuts and seeds are often viewed as high quality proteins but they are comprised
mainly of carbohydrate or fat and lacking certain amino acids to make a complete protein.
• While legumes contain a small amount of protein, it’s best to view them as “bonus protein grams”
but not a main source.
• Dairy products are an excellent source of protein when you select the low-fat or nonfat versions,
such as cottage cheese and yogurt.
• Cheese is high in saturated fat, known to raise your “bad” cholesterol.
• Use cheese moderately as a way to add flavor, rather than a main protein source.
• Eating legumes, nuts, seeds and dairy products can be a part of a healthy diet; providing flavor,
texture, and a variety of nutrients with a few extra protein grams. Eat them mindfully.

105
Legumes:
•
Legumes include beans, peas and lentils. They are an
excellent source of complex carbohydrates and provide a
wide range of essential nutrients including dietary fiber,
minerals, vitamins, and some protein.
•
Nutritional composition: 27% protein, 70% carbohydrates, and 3% fat.
•
Average per cup: 240 calories per cup and 15 grams of protein.
•
To meet your protein needs post op, you can use soy products or add a protein-rich
powder to nonfat refried beans, lentil or bean soups.
•
Think of legumes as a great complex carbs with “bonus” grams of protein.
Nuts & Seeds:
•
Nuts and seeds are rich sources of energy/calories, heart-healthy fats, fiber, plant
protein, vitamins & minerals, and phytochemicals.
•
Nutritional composition: 13% protein, 15% carbohydrate, 72% fat.
•
Average per cup: 800 calories and 25 grams of protein.
•
While nuts and seeds are healthy for your heart, they can be detrimental
to your weight as the calories can add quickly.
•
Use nuts and seeds to enhance the flavor and texture
a meal. Eat sparingly.
Dairy:
•
Cheese is a rich source of many nutrients such as calcium, phosphorus, zinc, vitamin A and
vitamin B12.
•
Nutritional composition: 23% protein, 6 % carbohydrate, and 70% fat.
•
Average cheese per ounce is 100 calories, 7 grams protein & 6 grams saturated fat.
•
Select the nonfat or low-fat dairy options.
Choosing Your Proteins
• The calories from the protein sources vary greatly, depending on the fat and carbohydrate
content.

106
• When choosing protein, look for sources high in protein grams and low in calories to
maximize nutrition and keep calories low for weight loss and maintenance.
• A guideline to make this selection easier is: a minimum of 10 grams of protein for every
100 calories. The higher the protein grams and lower the calories, the better.
• This formula will help you assess the quality of the protein source quickly to determine if it is
a low, medium or high quality protein source.
For example:
Food Amount Calories Protein Grams Quality
Protein shake 1 shake 160 30 high
Chicken 1 ounce 50 9 high
Cottage cheese - 1% 1 cup 160 28 high
Halibut 1 ounce 40 8 high
String cheese 1 ounce 80 8 medium
Ribeye 1 ounce 80 8 medium
Chicken sausage 1 ounce 50 5 medium
Mozzarella cheese 1 ounce 85 6 medium-low
Almonds 1 ounce 165 6 low
Peanut butter 1 level tablespoon 95 4 low
Black beans 1 cup 220 15 low
Cheddar cheese 1 ounce 115 7 low

107
Daily Caloric Intake
· The 10% guideline also applies to your daily calories.
· For every 100 calories you eat, a minimum 10 grams should be coming from lean, high quality
protein sources; up to the 60 grams/day.
· This guideline is designed to keep you focused in receiving enough protein each day while keeping
your calories low to maximize your weight loss.
· Weight loss may slow down or stop once daily calories are 1000 or more per day depending on the
individual.
For example:
Average Calories per Day Average Protein Grams per Day
High Protein to
Low Calorie ratio?
520 62 yes
925 48 no
810 65 yes
600 31 no
1250 83 yes
Protein Needs
• Your protein needs will vary with each individual though the general goal is 60 - 80 grams of high
quality protein daily.
• Protein needs to be spread out throughout the day with your meals and snack(s).
• Add up the protein: 15 - 20 grams per meal/snack x 4 meals = 60 to 80 grams of protein/day
For example:
Meal
Food
Amount
Calories
Protein Grams
Breakfast
1% cottage cheese and
pineapple
¾ cup
2 oz
.
120
14
21
0
Lunch
Deli ham &
LF string cheese
3 oz.
1 oz.
90
70
15
8
Snack
PB2 and
½ apple
2 Tbsp.
4 oz
.
45
60
5
0
Dinner
Chicken thigh
Broccoli
3 oz.
½ cup
180
25
22
2
Total
605
73

108
Tracking Protein Intake
Food records
•
Keeping a food journal is essential to track your progress and ensure you are meeting your
required protein needs.
•
Records will also help you track which foods are best tolerated and which proteins to avoid.
•
Food records include: the time, food, amount, calories, and protein grams, any intolerances,
and hunger/fullness levels.
•
It’s also helpful to note your mood/feelings, location, and who you are eating with.
•
Keeping a food journal allows you to review your progress and assess the best proteins,
foods, and amounts to keep you fueled, full and satisfied.
Weigh and measure
• Weigh and measure your proteins on a kitchen scale often to ensure
accuracy of your protein intake.
• Many patients overestimate their daily protein grams when they rely on
“eye-balling” their protein quantity.
• Using a scale and keeping food records are critical tools for success.
If you find you are getting hungry quickly after a meal, there are several factors
that may explain this:
• The carbs you are eating are quickly utilized burned up, leaving your hungrier faster.
• The protein source was in a liquid or soft form (i.e. protein shake or yogurt).
• You didn’t eat enough protein grams at the meal (i.e. 1 oz. chicken vs. 3 oz. chicken)
• You didn’t eat enough quantity of protein with complex carbs to last very long.
• You’ve gone too long between meals and need to refuel your body.
Tips:
Eat proteins first and choose high quality protein sources.
Have the majority of your carbohydrates come from vegetables and fruits.
Eat at regular meal times, do not skip meals.
Track the meals that provide you the most satiety and enjoyment.
Continue to expand the variety of proteins and foods you eat to increase nutrition and
enhance enjoyment.

109
Protein Meal and Snack Ideas (Stage 5 and Beyond)
• To keep meals simple and your protein intake high, create a list of 2 - 4 menu ideas for each
meal that you enjoy, are high protein, and well tolerated.
• This approach provides structure, standard items on your grocery list and enough variety to
provide proper nutrition and optimum enjoyment.
Breakfast:
•
Cottage cheese or yogurt with fruit
•
Egg & veggie scramble
•
Protein shake
•
Egg bites - eggs, veggies, low-fat cheese and turkey bacon,
ham or chicken sausage baked up in muffin tins for a quick and easy breakfast.
•
Chicken sausage (Flavors: garlic herb, sweet Italian, Andouille, pesto, hot Italian, etc.)
•
Veggie-loaded breakfast casserole: eggs, spinach, mushrooms, onion, bell peppers,
cheese. Add a chicken sausage for extra flavor & protein.
•
Ham, egg and cheese roll ups – with spinach and tomato.
Lunch:
•
Deli meat (ham, chicken, turkey, or lean roast beef) wrapped around string cheese. Dip in
gourmet mustard.
•
Soups- a flavorful way to get in your protein with lots of
vegetables (i.e. Chicken Fiesta soup, Indian Stew, Chunky
Turkey Vegetable soup).
•
Small green salad topped with shredded chicken, shrimp or hard-
boiled egg.
•
Leftovers from dinner of lean meat and veggies.
•
Mini meatloaf – bake in a muffin tin for just-right-sized meals.
•
Garlic parmesan chicken thighs.
•
Beef & Broccoli Stir fry with Cauliflower Rice
•
Buffalo chicken salad: chicken, Cajun hot sauce, baby spinach,
cherry tomatoes, onions, cilantro cottage cheese ranch dressing.

110
Dinner:
•
Chicken sausage & mushroom pizza bowls - with marinara, low fat mozzarella cheese
and Italian seasoning blend.
•
Ground turkey taco wraps - with pinto or black beans, low fat cheese, tomatoes, onion,
cilantro and iceberg lettuce.
•
Baked salmon with avocado salsa and broccoli.
•
Grilled halibut with garlic cilantro sauce and asparagus.
•
Stuffed bell peppers - lean ground turkey or beef, black
beans, spices and topped with low-fat cheese and green
onions.
•
Meat & veggie spaghetti sauce over zucchini or spaghetti
squash.
•
Buffalo Chicken Zucchini Boats: chicken, Monterey jack cheese, cottage cheese ranch
dressing, zucchini, and hot sauce. Optional garnish: sliced red onion, fresh cilantro,
avocado slices.
•
Ground Beef Enchilada Zucchini Boats: ground beef, taco seasoning, onion, zucchini,
enchilada sauce, cheese, & cilantro.
Dessert:
•
High protein pudding: nonfat plain Greek yogurt, chocolate
protein powder, stevia drops, milk. If you want the consistency
of ice cream, freeze it for minimum of 1 hour.
•
Low fat ricotta cheese whipped with stevia and fruit. Freeze for
a minimum of one hour.
•
Apple slices dipped in PB2.
Finding recipes
•
There are many online resources to find new high protein recipes and ideas.
•
Searching for bariatric friendly or Paleo recipes on bariatric support sites, Google, or Pinterest
can be a great starting place.
•
Remember that not all recipes labeled as bariatric-friendly will be appropriate for you to make or
eat.
•
Be sure you choose ones that are in alignment with your bariatric team’s recommended dietary
guidelines.

111
Protein Chart
This list of protein sources is based on average
calories per ounce, cup, or level tablespoon.
Both calories and protein grams were rounded
up or down for ease of use.
BEEF
DAIRY - low fat options
Food
Calories
per cup
Protein
grams
Cottage cheese
1% 160 28
2% 200 28
4% 220 26
Greek yogurt: NF, plain 135 25
Yogurt: NF, plain 120 14
DELI
Food
Calories
per oz.
Protein
grams
Bologna 90 3
Canadian bacon 30 5
Chicken 30 5
Corned Beef 30 5
Ham 30 5
Liverwurst 90 4
Pancetta 100 4
Pastrami 40 6
Pepperoni 150 6
Prosciutto 55 7
Roast beef 30 5
Salami
70 4
Turkey 30 5
Food
Calories
per oz.
Protein
grams
Bologna
90
3
Beef jerky
80
15
Beef Top
Round
50
9
Brisket 90 7
Flank
55
8
Ground beef (93% lean)
40
6
(85% lean)
70
8
(80% lean)
70 7
Hot dog
90
3
Pastrami
40
6
Pot Roast
90
9
Prime Rib 70 5
Ribeye
70
7
Ribs
100
6
Roast Beef
50
8
Salami - soft 75 4
Salami
-
hard
110
6
Shank
60
10
Skirt steak
65
7
Summer Sausage
100
5
T
-
bone
50
7
Top Loin (NY Strip)
65
6

112
FISH & SEAFOOD
Food
Calories
per oz.
Protein
grams
Ahi 30 7
Bass 35 6
Catfish 30 5
Clams 40 7
Cod 30 7
Crab 20 5
Halibut 40 8
Lobster 25 2
Mussels 50 7
Oysters 25 3
Salmon 45 6
Smoked
salmon jerky
90 15
Scallops 30 7
Shrimp 30 6
Tilapia 35 7
Tuna fish
(can or pouch)
35 7
POULTRY
POULTRY – continued
Food
Calories
per oz.
Protein
grams
Turkey
breast 40 9
drumstick 45 8
thigh 50 5
wing 50 9
ground 65 6
turkey bacon 65 6
turkey jerky 100 19
Duck 55 6
Goose 65 8
Goose liver pate 130 3
Pheasant 70 9
PORK
Food
Calories
per oz.
Protei
n
grams
Chicken
breast 50 9
drumstick 50 8
thigh 60 7
wing 60 9
ground 55 6
Chicken sausage 50 5
Egg (large) 70 6
Cornish game hen 40 11
Food
Calories
per oz.
Protein
grams
Bacon
150
11
Blood sausage
105
4
Bologna 70 4
Bratwurst
90
5
Canadian bacon
50
7
Chorizo
130
7
Ground pork
80
7
Ham steak
35
5
Pancetta 100 4
Pepperoni
150
6
Pork chops
55
9
Pork liverwurst
90
4
Pork loin 60 8
Pork roast
55
8
Pork ribs
75
8
Pork sausage –
bulk, link or patty
100 6
Pork & beef salami 95 4
Prosciutto
55
7

113
SOY
Food
Calories
per cup
Protein
grams
soy beans -
dry roasted
520 56
Soybeans- shelled
250 22
Tofu – firm 175 21
Tofu - soft 150 16
Tempeh 350 31
DAIRY & PLANT-BASED PROTEINS
Plant-based and higher fat dairy proteins
are typically higher calorie and lower in
protein.
Choose wisely.
CHEESE
CHEESE – continued
Foo
d
Calories
per oz.
Protein
grams
Mozzarella - whole milk 85 6
Parmesan 120 11
Pepper Jack 100 7
Provolone 100 7
Ricotta - light 25 2
Ricotta - part skim 40 3
Ricotta - whole 50 3
Swiss 105 7
LEGUMES
Food
Calories
per oz.
Protein
grams
American 90 5
Asiago 100 6
Bleu 100 6
Cheddar 115 7
Chevre 60 4
Cream cheese - regular 100 2
Cream cheese - low fat 65 3
Cream cheese - fat free 25 4
Feta 75 4
Gouda 100 7
Havarti 110 7
Laughing Cow – regular 70 3
Laughing Cow – light 45 3
Mascarpone 125 2
Monterey Jack 100 7
Food
Calories
per cup
Protein
grams
Beans
Adzuki 295 17
Black 220 15
Cannellini 180 14
Fava 180 14
Garbanzo
210 11
Great Northern 300 19
Lima 190 12
Lupini beans 200 26
Navy 295 20
Pinto 205 12
NF refried beans
260 18
Red kidney 220 16
Peas
Black-eyed 185 11
Split peas 230 16
Lentils 230 18
Soybeans 250 22

114
NUTS & SEEDS
NUT BUTTERS
Food
Calories per
level Tbsp.
Protein
grams
Almond 100 4
Brazil 95 2
Cashew 100 2
Flax 95 2
Hazelnut 90 2
Hemp seed 90 5
Macadamia 90 0
PB2 (2Tbsp) 45 5
Peanut 95 4
Pecan 125 2
Pistachio 85 3
Pumpkin seed 75 3
Sesame seed 90 3
Soynut 95 4
Sunflower seed 90 3
Walnut 100 3
Food
Calories
per cup
Protein
grams
Nuts
Almonds 825 30
Brazil 870 19
Cashew 905 27
Hazelnut 840 16
Macadamia 920 8
Peanuts 850 35
Pecans 800 12
Pine nuts 800 16
pistachios 680 24
walnuts 800 20
Seeds
Chia 960 48
Flax 745 32
Hemp 905 53
Poppy 735 26
Pumpkin 680 36
Sesame 820 26
Sunflower 760 32

115
Soy
• Soy is in rich in vitamins, minerals, calcium, iron, fiber,
phytochemicals and protein.
• Studies have found soy can help prevent and improve some
of today’s top health issues such as heart disease, high blood pressure, osteoporosis, certain
cancers; and menopausal symptoms like hot flashes, night sweats, and insomnia.
• Soy foods are popular with vegetarians and vegans who often rely on them for their main source
of protein; as soy contains all of the essential amino acids.
• Soy is very versatile and can be eaten as whole beans (edamame) or processed as tofu, tempeh,
soy yogurt, miso, soy milk and other soy-based products.
Product Amount Calorie
s
Protein Grams
Soy beans: shelled 1 cup 250 22
Soy nuts: dry roasted 1 cup 520 56
Soy cheese 1 oz. 70 7
Soy milk 1 cup 90 6
Soy powdered
protein: unflavored
¼ cup 70 17
Soy yogurt 1 cup 140 6
Tempeh 1 oz. 60 6
Tofu: firm 1 oz. 30 3
soft 1 oz. 20 2
silken 1 oz. 15 1.5
Types of Tofu
• Firm: is dense and can be cubed and stir-fried, grilled, scrambled, pickled, smoked,
baked, barbecued or served in soups. Firm tofu is higher in protein, fats and calcium than
other types of tofu.
• Soft: is better suited for recipes in which tofu needs to be blended.
• Silken: has a creamy structure and is also used in blended dishes.

116
Lupini Beans
• Lupini beans are large, flat, round, yellowish seeds in the legume family, native to Italy.
• They are traditionally eaten as a pickled snack food, in the Mediterranean basin and
Latin America.
• Lupini are commonly sold in jars; brined like pickles or olives.
• They have a thick outer skin that needs to be torn to get to the bean; though you can eat the
skins too.
• Highly skilled lupini eaters learn to split the skin by rubbing the bean between forefinger and
thumb; popping it directly into their mouth.
• They are a nutritious snack when you want something salty and “crunchy” to eat.
Lupini bean facts:
•
One of the highest sources of plant proteins available after soybeans
•
The bean skin consists mainly of cellulose (insoluble bran fiber)
•
Rich in antioxidants and amino acids, especially arginine
•
Have a low glycemic index; great for diabetics
•
Easy to digest and high bioavailability
•
High in vitamins, especially B complex, and minerals
•
Low in fat, cholesterol, and is gluten free
•
Probiotic food, promoting the growth and nurturing of “good” gut bacteria
Nutritional composition:
•
45% protein
•
34% carbohydrates
•
21% fat

117
Cooking Lupini Beans
These delicious beans are a healthy protein snack but they do require a bit of patience to
prepare.
1. Pick over beans to remove any debris.
2. Put the beans in the pot of water and soak overnight for 24 hours. Be sure that the water
covers the beans totally. After twelve hours, check on the beans to make certain they’re
completely immersed and add more water if required.
3. After the 24 hour period of soaking, drain the water and refill with fresh water covering the
beans completely.
4. Bring the beans into a boil as well as simmer for 1 ½ hours. Add more water if needed.
5. Drain, rinse well, and cover with salted water (about one tablespoon per quart of water).
6. Allow them to cool and then refrigerate.
7. Repeat this process twice a day for 7 days or until the soaking brine is no longer bitter.
8. Store the beans in air-tight container within the fridge. They’ll keep for about 6+ weeks.
Where to Buy
Dried: Amazon, Nuts.com
Prepared: Amazon, Walmart.com, Luckyvitamin.com

118
How will I know when I am full?
•
Your tiny stomach won’t be able to hold much, so initially you may only be able to tolerate
2 - 3 teaspoons of food at one time.
•
You may have trouble knowing when you are comfortably full. Take dime-sized bites or sips
so if you eat too much it’s a very small amount and less likely to cause distress.
•
Meals should take the full 20 minutes to complete (but no longer than 30). Eating
slowly allows you the time to determine your “last bite/sip threshold.”
•
Nausea may be your first indication of fullness. Don’t let this alarm you.
•
You may feel pressure in the center of your stomach or pain in the shoulder area or upper
chest when you are full.
•
It will take time for your body to adjust to the stomach’s smaller size and return to a
normal “full” feeling.
•
Eat mindfully, with intention and attention (awareness).
What is the Honeymoon period?
· The time period you have no hunger. The length of time this occurs varies widely; between
weeks, months to years.
· Often patients decide to skip meals because they are not hungry or have no appetite. They
deprive themselves of their nutritional needs.
· You will need to plan you meals to fuel your body throughout the day to meet your nutrition
goals and have a successful weight loss.
If I get upset and want to eat, what will I do?
· Managing stress is important to your overall health and well-being.
· Try different ways to handle your stress by talking with someone, exercising, reading
or enjoying a hobby.
· Integrate healthy stress management daily habits, keeping your stress lower on a daily
basis helps keep the stress under control.
· You may consider talking with a mental health professional if you feel you need
additional assistance in dealing with stress or leaning how to constructively meet your
emotional needs.
FAQ - Frequently Asked
Questions

119
What about carbs?
There is no definitive recommendation for daily grams of carbohydrate (aka “carbs”) after bariatric surgery.
It’s more important to focus on the type of carbohydrate rather than the quantity of grams.
Complex carbohydrates:
· Vegetables
· Fruits
· legumes
Complex carbs provide vital
nutrients and are digested slowly; supplying a steady release of
glucose in your blood stream.
When combined with protein, you will stay fuller, longer. Complex
carbs from vegetables, fruits and legumes (i.e. i.e. black beans,
lentils, and split pea) are chalked full of vitamins, minerals, fiber
and small amounts of protein.
These foods are also naturally low in carbs, usually 5-15 grams per
serving.
Processed and simple carbohydrates: avoid excessive
carbohydrate intake of these foods.
· Bread
· Pasta
· Rice
· Crackers
· Tortilla
· Cereals
· Cookies
· Candy
· Cake
· Pastries
· Fruit juices
· Other sweets
These carbs potentially cause dumping syndrome or can cause a blockage.
If the carb is tolerated, then you can fall into old eating habits, slowing down weight loss and
potential weight gain.
Every person has their “crack” food item in regards to carbs. The food that they turn to when
stressed or need some comfort or a reward. The carb they crave. The carb they easily overindulge in
and fight to resist.
When you are contemplating have a processed carbohydrate, the question you have to ask yourself
is “Will eating this food (carb) help me or lead me down a slippery slope?”

120
For example, if you know you have a weakness for bread (aka it’s your “crack”), then don’t eat it!
Trying to convince yourself “just this once” is the type of thinking that got you to the bariatric program
in the first place. Be honest with yourself. “Just once” easily turns into every few weeks, then every
week, and eventually all the time.
On the other hand, if bread is not your carb of choose, having a slice of bread for a half sandwich
now and then might be just fine for you (if you can tolerate it without dumping). Only you can
determine if the carb/food you want to eat will ultimately help you toward your weight/health goals or
sabotage you.
What will I eat when I go to a restaurant?
• Restaurant eating will be a very different experience for you after the surgery.
• Ask the server to prepare your food in a low-fat manner.
• Be prepared to bring much of your meal home in a “doggie bag”.
Dining out tips:
•
Bring your Bariatric restaurant card (given to you at your 2 month visit) with you so you can
order off the smaller menu.
•
Look online to preview the menu. Be assertive in asking for special orders.
•
Focus on protein first and then vegetables.
•
Try ordering 1 dinner and splitting it with someone else or 1 - 2 appetizers instead of a full
meal.
•
Ask that your food be broiled or baked with no added butter, oil, or fat.
•
Ask that bread, rolls, or chips not be brought to the table.
•
Concentrate on talking and listening to conversation.
•
No alcohol for the first year, then only in very small amounts.
•
The children’s menu is not always the answer for smaller portions as they are often laden
with fat calories so learning how to meet your dietary needs is essential.

121
How can I have fun at parties or weddings if I can’t eat a lot?
· Focus on the social aspect of the event, making a point to engage in conversation.
· Position yourself away from the food table and catch up with friends or get on the dance
floor.
· Scan the buffet in advance and make a plan as to what food you can eat.
· If the meal is served, call the facility ahead of time and ask what they will be serving and
make a request that will meet your needs.
· Try eating 1 or 2 healthy appetizers and/or a smaller portion of the meal.
· Your dietitian can provide you with tips to make parties and events more enjoyable and
healthy.
When can I drink alcohol after surgery?
· Alcohol is not recommended after bariatric surgery for a minimum of one year and then only
in moderation.
· Alcohol provides calories with minimal nutrition; working against your weight loss goal.
· Alcohol absorbs more quickly after surgery and the alcohol will be more potent.
· For some patients, alcohol use can increase and lead to alcohol dependence.
· Alcohol can lead to developing an ulcer.
· For all of these reasons, it is recommended to avoid alcohol after
bariatric surgery.
122
Do I really need to go to all my bariatric follow up appointments?
YES! Your anatomy has changed; therefore your medical and nutritional needs have changed.
Long-term follow up with your bariatric team requires attention to several aspects of care.
· Make sure you are adjusting to your procedure.
· Assess your nutrition intake to safely maximize weight loss and prevent weight gain.
· Discuss weight loss progress.
· Evaluate potential complications resulting from improper behavior or from surgical
complications.
· Monitor status of your comorbidities.
· Adjust medications, if needed.
· Check laboratory values.
· Answer any questions or concerns you may have.
· The follow-up visits may be the surgeon, a physician assistant, a nurse, or the dietitian.
· It is important that you follow this long term care so that any problems or concerns that
develop over time can be addressed by your team.
· The team is here to educate, guide, support, and motivate you continuously, so you can
achieve a healthy weight after surgery.
123
124
Vitamins & Medications after Bariatric Surgery
Short Term:
Omeprazole:
• 20 mg a day for 3 months for gastric bypass and possible vertical
sleeve gastrectomy patients (may not need it)
• This medication decreases the production of stomach acid allowing better
healing of your stomach pouch
Ursodiol: No Longer Prescribing
Long Term:
Vitamin B12: For gastric bypass patients only
• 500 micrograms a day. Take one per day.
Calcium Citrate with Vitamin D:
• 1500 - 2000 mg per day.
• Take in 500 - 600 mg calcium citrate with 400 IU vitamin D dosage, 3 - 4
times a day, depending on the brand.
• Many patients require Vitamin D, in addition to what they receive with their
calcium. Dose will depend on blood test results.
Multiple Vitamins with minerals and iron added:
• Take one per day.
Iron Supplements:
• Separate Iron supplement is prescribed to pre-menopausal women and
as needed for others.
• Take iron as prescribed by your surgeon.
• Do not take iron and calcium at the same time (separate by 2 hours).
• Vitamin C (250mg) is needed for absorption of some iron supplements.
Probiotics:
Described in this section.
125
Why we take a Vitamin/Mineral Supplement Every Day
• Bariatric surgery dramatically alters your body's ability to absorb vitamins, minerals and
nutrients from the smaller amounts of food you'll be eating.
• The resulting vitamin and mineral deficiencies can have serious medical implications.
• As a bariatric surgery patient, it is absolutely essential that you take a good quality
multiple vitamin and mineral product daily, for the rest of your life.
• You will also need to take additional calcium, Vitamin B-12 and perhaps Iron
supplements. These supplements are necessary to prevent vitamin and mineral
deficiencies after bariatric surgery.
The following are deficiency symptoms of some of the most important vitamins and minerals.
If you often forget to take your supplements, you will be at a higher risk of developing these
conditions. Your doctor will request that you have vitamin and mineral levels checked
periodically.
Folate (Folic Acid, Folacin)
• Poor growth
• Blood disorders
• Anemia
• Elevated blood levels of homocysteine (a blood chemical linked to the clogging
of arteries).
• GI tract disturbances
Vitamin B-12 (Cobalamin)
• Degeneration of cerebral white matter, optic nerves, spinal cord and peripheral nerves.
Symptoms include numbness, tingling, and burning of the feet as well as stiffness and
generalized weakness of the legs.
• Anemia
• It may take 5 - 6 years for deficiency symptoms to appear after natural sources of
the vitamin are restricted.
Calcium
• Bone deformities (osteoporosis, osteomalacia and rickets)
• Tetany – extremely low levels of calcium in the blood may increase the irritability of
nerve fibers and nerve centers, resulting in muscle spasms such as leg cramps
(tetany).
• Hypertension (high blood pressure).
• Muscle spasms
• Personality changes
• Nausea and vomiting
Iron
•
Malfunction of a variety of body systems
•
Fatigue, irritability
•
As iron deficiency anemia becomes more severe, defects develop in the structure
and function of the tongue, nails, mouth and stomach. Skin may appear pale, and the
inside of the lower eyelids pink instead of red. Fingernails become thin and flat, and
eventually spoon-shaped nails develop. The tongue may burn, and/or appear red,
smooth and waxy.
•
Extreme cases of untreated anemia can eventually result in heart failure.

126
Potassium
•
Nausea, feeling anxious, drowsy or weak.
•
Irregular heart beat
Magnesium
•
Tremors
•
Muscle spasms
•
Personality changes
•
Nausea and vomiting
Vitamins/Supplements Requirements
• The American Society for Metabolic and Bariatric Surgery (ASMBS) daily
recommendations has specific recommendations for vitamins and need to be taken
every day for the rest of your life to prevent deficiencies.
• Consistently taking the supplements daily is a critical part to your overall health.
• For the first few months you may not be able to swallow larger pills. Most patients find it
easier to take a chewable or liquid for calcium citrate and multivitamins.
• Chewable and liquid supplements usually contain sugar for flavor, which can result in
dumping (especially with liquids) and added calories. Read the label carefully.
Vitamins/Minerals Gastric Bypass Sleeve Gastrectomy
Multivitamin with iron 1 svg/day 1 svg/day
Calcium Citrate with Vitamin D3
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
500 - 600 mg svg, 3x/day
(1500 - 2000 mg day)
Probiotic 1 svg daily 1 svg daily
Vitamin B12
1 svg/day
(500 micrograms)
NA
Multivitamin (MVI) with iron = 200% of daily value* Begin on day 1 after hospital discharge
Take 1 serving of multivitamins daily for a lifetime.

127
TIPS
• Take a complete multivitamin with at least 18 mg iron, 400 mcg folic acid, and
containing selenium and zinc in each serving.
• Specialized bariatric brands tend to be high quality, better absorbed and better tasting.
• Specialized bariatric formulations are available but not all contain iron so read the label
carefully.
• Serving size will depend on individual products.
• Chewable and liquid vitamins are best absorbed.
• For the first 2 months after surgery, take a chewable multivitamin (there is no liquid form
that contains iron).
• Progress to whole tablet/capsule as tolerated; if you decide to switch to a pill form after
2 months, soft gels or capsules may be better absorbed than tablets.
• May improve gastrointestinal tolerance and absorption when taken close to food intake
(except with dairy).
• May separate dosage.
• Every brand has several, very similar variations of a multivitamin with iron. Make sure to
read the label!
• Multivitamin containing iron needs to be separated by at least 2 hours from
calcium supplements for maximum absorption.
AVOID
• Avoid time-released supplements.
• Avoid enteric coating.
• Avoid children’s formulas that are incomplete.
• Do not take MVI in gummy form. Gummies don’t have all the vitamins & minerals
required.
• Do not take “all in one” multivitamins and calcium citrate supplements.
• Do not use patch vitamins. There is no way to know to know the rate of absorption
so we do not recommend this form of vitamins.
• There are no multivitamins with iron in liquid form. If you use a liquid multivitamin,
you will need to take an additional iron supplement.

128
Recommended Multivitamins with iron
• The chart is a list of multivitamins with iron supplements that meet the (ASMBS) daily
recommendations for bariatric patients.
• The chart includes the brand name, serving size on the label, calories (if any), iron mg,
folic acid mcg, and dosage.
• The last column indicates the amount you need to take to meet your daily minimum
requirement. All the brands listed contain selenium and zinc in each serving.
Multivitamin with Iron Recommendations
Chewable or Soft Gel (first 2 months post op)
Brand Serving size
Iron
(mg)
Folic acid
(mcg)
Daily Minimum
Required Amount
Bariatric Advantage
Advanced Multi EA Chewable
Tablets
2 tablets
(20 calories)
45 800
2 tablets daily
(20 calories)
Celebrate Multi-Complete 36
Chewable with Iron
2 tablets
(15 calories)
36 800
2 tablets daily
(15 calories)
Celebrate Multi-Complete 18
Chewable with Iron
1 tablet
(10 calories)
18 800
1 tablet daily
(10 calories)
Opurity Bypass & Sleeve
Optimized - Chewable
1 tablet
(10 calories)
18 800
1 tablet daily
(10 calories)
Multivitamin without Iron Recommendations (separate iron supplement required)
Chewable (first 2 months post op)
Brand Serving size
Folic acid
(mcg)
Daily Minimum
Required Amount
Bariatric Advantage Multi
Chewy Bites
2 chewies
(35 calories)
800
2 chewies daily
(35 calories)
Bariatric Advantage Essential
Chewable Multi
2 tablets
(10 calories)
800
2 tablets daily
(10 calories)
BariMelts Multivitamins
Fast melting tablets
2 tablets 800
2 tablets daily
(10 calories)
Celebrate Multivitamin
Chewable
2 tablets
(10-15 calories)
800
2 tablets daily
(10-15 calories)
NOTE:
• If you choose a mutlitvitmain that does not contain iron, you will need to take a
separate iron supplement to meet your bariatric needs.
• Iron supplements: described later in this section.
• Some multivitamins are not included in this chart due to sugar content (grams) &/or high
calories or lacking nutrients. Make sure to read the labels before purchasing.

129
Multivitamin with Iron Recommendations -
Tablet or Capsule (for before surgery and 2 - 3+ months post op)
Brand Serving size
Iron
(mg)
Folic acid
(mcg)
Daily Minimum
Required Amount
Bariatric Advantage Ultra
Multi with Iron
3 capsules 45 800 3 capsules daily
Opurity Complete Bariatric
Optimized Multivitamin
Multimineral Supplement
2 capsules 18 800 2 capsules daily
Opurity Every-Day Multi 1 tablet 18 400 1 tablet daily
Pro Care Health 1 capsule 18 800 1 capsule daily
TwinLabs Daily One with Iron 1 capsule 10 400 2 capsules daily

130
Calcium
Calcium is a mineral that is vital for life. It aids in building bones, clotting our blood, makes our
nerves send messages and muscles contract. Approximately 99% of the calcium in our bodies
is in our bones and teeth. We lose calcium every day through our hair, nails, skin, sweat, urine
and feces. Our bodies cannot produce new calcium. That’s why it’s important to try to get the
calcium we need. If we don’t get enough calcium for our body’s needs, it is taken from our
bones.
Finding the right calcium supplement can be confusing. Often people misread a supplement
label and don’t get the amount or type they need.
• Every bottle is different since every calcium manufacturer has its own serving size and
amount of calcium and Vitamin D3 it provides.
• Most calcium supplements have a serving size of two, so most people think they are
taking 1000 - 1200 mg a day when in fact, they are only taking 500 or 600 mg for that
serving.
• On top of that, serving sizes can range from three to six tablets. Pay close attention to
the label so you don’t take too little or too much.
Calcium Citrate = 1500 - 2000 mg/day - begin on day 1 after hospital discharge.
•
Choose a brand with calcium citrate & Vitamin D
3.
• Begin with chewable or liquid. Chewable and liquid vitamins are best absorbed.
• Chewy or wafer calcium citrate supplements are permitted
• Progress to whole tablet/capsule as tolerated; usually after 2 months.
• Split into 500 - 600 mg doses for optimum absorption; if you take more than 600 mg,
the remaining will be excreted in the urine.
• Be mindful of serving size on supplement label.
• Space doses evenly throughout day.
• Choose a brand that contains magnesium is recommended.
• Wait at least 2 hours taking multivitamin or iron supplement.
• Do not combine calcium with iron containing supplements to maximize absorption &
minimize gastrointestinal intolerance.
• Calcium citrate is not as dense as calcium carbonate and is often more easily absorbed.
That’s why calcium citrate is usually two pills in one dose while calcium carbonate is
usually one pill in a 600 mg dose. So look at the label to see what you're getting.
• Do not take calcium in gummy form. Gummies are not calcium citrate and are not the
best absorbed
• Do not take products that contain calcium carbonate; i.e. Caltrate®, Viactiv®,
Tums®,
OsCal®, calcium triphosphate, oyster shell, bone meal, etc.
CAUTION: most of the liquid or chewable are flavored and have calories. These calories can
add up fast when you have to take them 3 - 4 times a day.
For example:
o Bariatric Advantage 250 mg Calcium Chewy Bites: each chew is 250 mg calcium
citrate, 20 calories per chewy and 4 grams of sugar alcohol.
o You would need to take a total of 6 chews, consuming an extra 120 calories and
24 grams of sugar alcohol to meet your requirement of 1500+ mg a day.

131
Possible side effects of taking calcium:
Gas or constipation may occur. If increasing fluids does not solve the problem, try
another brand of calcium. It may require trial and error to find the right supplement for
you, but luckily there are many choices.
If you are having challenges with a new calcium supplement, start with a smaller amount
to better tolerate it. When switching supplements, try starting with 200 - 300 mg every
day for a week, and drink an extra 6 - 8 ounces of water with it. Then gradually add more
calcium each week.
Read the label carefully. The label will tell you:
Serving size (i.e. 4 tablets, 2 caplets, 1 chew, 1 Tbsp., 4 wafers, etc.)
Amount of calcium (mg) per serving (i.e. 240 mg, 500 mg, 1000 mg)
Calories per serving (usually in liquid or chewable forms)
Type of calcium (i.e. carbonate, citrate, gluconate, etc.)
Only choose calcium citrate

132
Calcium Citrate with Vitamin D3 Recommendations
• The chart is a list of recommended calcium citrate supplements.
• The last column indicates the serving size and doses throughout the day you need to
take to meet the minimum daily requirement recommended by the American Society for
Metabolic and Bariatric Surgery recommendations (ASMBS).
1500 - 2000 mg/day: 500 - 600 mg doses, 3 - 4 times a day.
Chewable or Liquid (first 2 months post op)
Brand
Serving
Size
Calcium
Citrate
Vitamin
D3
Daily Minimum
Required Amount
Bariatric Advantage 500 mg
Calcium Citrate Chewy Bites
1 chew
(15 cals/svg)
500 mg 500 IU
1 chew, 3x/day
(45 calories)
Bariatric Advantage Chewable
Calcium Citrate - 500 mg
1 chewable
tablet
(10 cals/svg)
500 mg 300 IU
1 tablet, 3x/day
(30 calories)
Bluebonnet Liquid Calcium
Citrate Magnesium and
Vitamin D3
1 Tbsp.
(5 cals/svg)
600 mg 400 IU
1 Tbsp., 3x/day
(15 calories)
Celebrate Calcium Citrate -
Chewable
1 tablet
(5 cals/svg)
500 mg 333 IU
1 tablet, 3x/day
(15 calories)
Celebrate Calcium Citrate Soft
Chews
1 piece
(15 cals/svg)
500 mg 500 IU
1 piece, 3x/day
(45 calories)
Opurity Calcium Citrate Plus
Chewable
4 tablets
(20 cals/svg)
1200 mg
800 IU
2 tablets, 3x/day
(60 calories)
Wellesse Liquid Calcium 1000
mg & Vitamin D3
2 Tbsp.
(15 cals/svg)
1000 mg
1000 IU
1 Tbsp., 3x/day
(22 calories)
Caplet or Tablet form (for before surgery and 2 - 3+ months post op)
Brand
Serving
Size
Calcium
Citrate
Vitamin
D3
Daily Minimum
Required Amount
Celebrate Calcium Citrate -
Tablets
6 tablets 1200 mg 1200 IU 3 tablets, 3x/day
Citracal Petites with Vitamin D3 2 tablets 400 mg 500 IU 3 tablets, 3x/day
Nova Nutritions Calcium Citrate
with D3
2 tablets 700 mg 400 IU 2 tablets, 3x/day
Puritan's Pride Calcium Citrate
+ Vitamin D3 Miniatures
2 tablets 400 mg 500 IU 3 tablets, 3x/day

133
Vitamin B
12
= 500 mcg/day (bypass only) - Begin on day 1 after hospital discharge
•
Available forms include sublingual tablets, liquid drops, mouth spray, or nasal gel/spray.
•
Required for bypass (RNY) patients only.
•
Some bariatric brand multivitamins contain 500 - 1000 mcg of Vitamin B12. Read the
labels.
Iron - take iron supplement if you choose a multivitamin without iron if additional iron is
prescribed by your doctor.
•
18–27 mg/d elemental. No enteric coating.
•
Begin with chewable or liquid; progress to tablet as tolerated.
•
Do not mix iron & calcium supplements, take at least 2 hours apart.
•
Avoid excessive intake of tea due to tannin interaction.
•
Vitamin C is often prescribed with iron as it may enhance absorption.
•
Iron is absorbed the best on an empty stomach but can cause stomach
cramps, nausea, and diarrhea in some people. You may need to take iron with
a small amount of food to avoid this problem.
•
When taking iron, avoid high fiber foods (i.e. whole grains, raw vegetables, & bran) or
foods or drinks with caffeine.
•
Milk, calcium and antacids should NOT be taken at the same time as iron
supplements. You should wait at least 2 hours after having these foods before
taking your iron supplements.
Iron Recommendations
Brand
Serving
Size
Iron
(mg)
Vit C
(mg)
Daily Minimum
Required Amount
Bariatric Advantage - 45 mg
Capsule (non- chewable)
1 capsule 22.5 200 2 capsules/day
Bariatric Advantage - 18
Chewable Iron
1 tablet 18 30 1 tablet/day
Bariatric Advantage – 60
Chewable Iron
1 tablet 60 250 1 tablet/day
Bariatric Advantage Iron
Chewy Bites
1 chewy bite 30 60 1 chewy/day
Celebrate Iron + C - 18 mg
Chewable
1 tablet
(5 calories)
18 36 1 tablet/day
Celebrate Iron + C - 60 mg
Chewable
1 tablet
(10 calories)
60 60 1 tablet/day
Celebrate Iron + C - 30 mg
Tablet (non- chewable)
1 tablet 30 60 1 tablet/day

134
Probiotics
• Probiotics are live microorganisms that provide health benefits.
• The human body harbors about 100 trillion bacteria, both good and bad. 80-90% of
these bacteria live in the digestive tract, mostly in the colon.
• Maintaining the correct balance of good and bad is necessary for optimal health. Things
like medications, diet, disease and your environment can upset the balance.
• An upset balance can result in symptoms.
• Probiotics supplements are considered safe and effective for preventing and treating
irregularity of the gastrointestinal tract, such as diarrhea, constipation, irritable bowel and
heart burn.
• Some studies have shown that probiotics can prevent H.pylori, vaginal candidiasis and
upper respiratory infections.
• Probiotics found in dairy products are typically small in quantity compared to that of a
supplement.
• We recommend that you take a probiotic supplement daily on a long term basis.
• Since there are a lot of supplements out there to choose from, we are providing you with
a list of some of the more comprehensive and better quality products, including where to
buy them, how much they cost and what bacteria they contain.
• Bowel habits are sure to change after surgery and constipation is a fairly common
problem. Taking a probiotic supplement daily and drinking adequate fluids will help to
prevent this. Diarrhea is not an expected complication after bariatric surgery.
• If you are experiencing diarrhea or other concerning digestive symptoms, to include
constipation that is not relieved by a daily probiotic, please call the bariatric clinic (425-
502-3454).
Recommended Probiotics
Brand
Notes
Align Probiotic Lactose, soy & gluten- free.
Bariatric Advantage Flora Advantage
Probiotic (Chewable)
Vegetarian and gluten-
free
BlueBiotics Daily Probiotic
No soy, gluten, or dairy,
100% vegetarian.
Celebrate BALANCE Probiotic
Vegetarian
Culturelle Digestive Health
No gluten, milk, soy, wheat
or preservatives.
Florastor Daily Probiotic Supplement
Vegetarian, gluten free, &
non-GMO.
Nutrition Now PB8
No gluten, eggs, peanuts,
tree nuts, soy or salt.
Renew Life Ultimate Flora Extra Care
Probiotic 150 Billion
Vegetable capsule, gluten
free. Contains traces of
dairy; may contain traces of
soy.
Trubiotics One a Day Probiotic Gluten & soy free.

135
Example Schedule for taking Vitamins & Supplements
Meal Vitamin & Supplements
Breakfast Calcium citrate with Vitamin D3, 500 - 600 mg
Snack
Multivitamin with iron
Iron (if additional iron prescribed by doctor)
Probiotic
Vitamin B 12, 500 mcg (Bypass only)
Lunch Calcium citrate with Vitamin D3, 500 - 600 mg
Snack Multivitamin with iron (if additional prescribed by doctor)
Dinner Calcium citrate with Vitamin D3, 500 - 600 mg
Where to buy vitamins and supplements:
Kaiser Permanente: carries the multivitamin (chewable and pill), calcium citrate with Vitamin
D3 (pill form) and Vitamin B12 (pill form).
Stores:
• Bartell Drugs
• Costco
• GNC
• Sam’s Club
• Super Supplements
• Trader Joes
• Walgreens
• Walmart
• Vitamin Shoppe
Online:
• Amazon.com
• BariatricAdvantage.com*
• CelebrateVitamins.com
• DrugStore.com
• iherb.com
• Puritan.com
• Unjury.com
• Walmart.com
Read the label to ensure the
correct formula and for low sugar
content.
* SPECIAL NOTE:
• Bariatric Advantage has a special offer for Kaiser Permeate patients.
• Receive Kaiser member pricing of roughly 20% discount & free shipping with
validation code: KAISER.
• Enter validation code on the left side of the page.
• Visit: BariatricAdvantage.com or call 1.800.898.6888
136
Post Op Concerns
What they are and how to prevent them
Many of the symptoms that can arise following surgery can be prevented. In the next couple of
pages, we will review some of the more common issues that patients can experience and steps
that you can take to help prevent them.
There are rare post-surgical concerns that can arise and are mechanical or structural in nature
that may require a surgical or endoscopic solution. There may also be medical issues that arise
and require treatment with medications. All of these are review as well.
It’s very important that you be journaling your food and fluid intake. See the Journaling in
section 10 for an explanation of how to journal affectively.
Following the guidelines that have been provided, in regards to eating and drinking, (to include
what you eat/drink, how much and how fast), can nearly always prevent symptoms that are not
the result of a mechanical/structural or medical issue.
However, it’s very important that you know what symptoms to watch for and when and who to
call with questions or for advice.
Always, always, always call if you have a question, concern or symptoms that do not resolve
quickly or are more urgent. We can help to determine the cause and/or seriousness of your
symptoms and provide you with advice. This is all new for you and we would not expect you to
not have questions and we encourage to you call, sooner rather than later.
Your symptoms may be something what we can help you to resolve by making some changes
to your diet or medications or we may advise that you see your primary care provider, come in
to see your bariatric surgeon or go to Urgent Care.
Bariatric Clinic 425-502-3454
Consulting Nurse if after hours 1-800-297-6877
137
Hydration / Dehydration
We recommend that you drink 56 ounces of fluid every day. The bare minimum is 32 ounces, to
prevent dehydration. In the full liquid phase, these numbers are in addition to the protein
drinks.
Low or no calorie fluids are best. Artificial sweeteners are not recommended. They are thought
to increase hunger.
It will be necessary to sip fluids all day long, with the exception of the 60 minutes after meals. In
the full liquid phase, you do not need to separate meals (protein drinks) and other fluids. Just
drink throughout the day, to ensure adequate hydration.
You may need to experiment with different temperatures and fluids to see what’s best tolerated.
Some patients don’t tolerate cold fluids, especially early on. Warm or room temperatures may
go down better. This applies to protein drinks as well.
As you lose weight, your body needs to rid of the waste products that weight loss creates.
Kidneys are vital for this process. In order for your kidneys to function properly, they need
plenty of fluids.
Dehydration can increase constipation, nausea and pain and can just all around make you feel
lousy.
Symptoms of dehydration can include:
Decreased urine output
Dry mouth
Dizziness / light headedness
Increased heart rate
Low blood pressure
Fatigue
Headache
Constipation
Once you get depleted, it can be very difficult to resolve dehydration on your own.
Always call the Bariatric Clinic 425-502-3454 (Consulting Nurse if after hours 1-800-297-6877) if
you are experiencing any of the above symptoms.
Our best advice is to do your best to get in the required amount of fluids each day.
138
Nausea / Vomiting
Contrary to popular belief, nausea and vomiting are not expected consequences of bariatric
surgery. There are numerous reasons that one might experience these symptoms following
surgery. The reason is often behavioral and can be resolved with some changes to either what
or how one is eating. On occasion your symptoms may require medication. Much less often,
the reason can be mechanical or structural, meaning that a procedure or surgery may be
required to resolve the symptoms.
Behavioral reasons that might result in nausea or vomiting include:
Eating the wrong foods
It’s very important to read labels. Some foods that seem as though they are very healthy
may have ingredients that are not tolerated. See dumping syndrome for further
information on foods that are less tolerated. It’s very important to read and understand
food labels and follow the recommendations in the nutrition section (section 6) for each
phase of the post op diet.
Eating too much
Your stomach pouch is about 30 cc. This is about the size of a shot glass or an egg.
Eating too much can result in foods to stack up and cause nausea and often vomiting.
Just one bite too much may set you over the edge. If you are experiencing nausea and
vomiting after meals, try reducing the size of your meal by a bite or two and see if your
symptoms resolve.
Eating too fast
You will need to take small bites, chew well and eat slowly. Concentrating only on your
meal (without distractions like TV or reading) will help you to eat slowly. Using small
utensils will remind you to take small bites. Meals should take about 15-20 minutes.
Not chewing well enough
It’s important to chew your food very well. At first you may want to use a timer or watch
the clock for all solid foods and chew each bite for at least 30 seconds. This will also
ensure that you are eating slowly.
Less frequently nausea and vomiting can be the result of a structural or medical problem.
Stricture
A stricture is a narrowing of the new connection that was created to connect your new
stomach pouch to your small intestine (RNY). If this is going to happen it is usually
between 3 weeks and 3 months post op. Symptoms are progressive and typically begin
with nausea, vomiting and a feeling that foods are stacking up, first with solid foods and
progressing to difficulty with soft foods and liquids. The treatment is dilatation during
endoscopy. If you develop the above symptoms, you need to call the Bariatric Clinic.
Ulcer
Stomach ulcers can develop in the pouch or at the new connection. The first symptoms
are usually nausea, vomiting and stomach pain. Sometimes the symptoms are
improved following a meal. Anti-inflammatory medications and smoking are the
most common causes of stomach ulcers. Call the Bariatric Clinic is you are
experiencing the above symptoms. Ulcers can be serious. Please don’t hesitate to call
the bariatric nurse with symptoms or concerns.
139
Constipation
Constipation is a very common complaint after surgery. It’s important to remember that bowel
habits will change following surgery. You are eating less food and different types of foods than
before surgery. Your body responds accordingly, producing fewer and smaller bowel
movements. The initial post op period can be challenging. You are without any food for a
couple of days, and then it’s just liquids. Add to that the narcotic pain medication that you are
given and you have a recipe for constipation. It’s best to be proactive, in the initial post op
period and beyond.
Fluids:
Follow the instructions for adequate hydration, getting at least 56 ounces of fluid each day.
Exercise:
Movement decreases the amount of time it takes for food to move through the large intestine
and stimulates the natural contractions of the intestinal muscles. This helps to efficiently move
the stool out. Walk 10-15 minutes several times a day to help keep the digestive track working
optimally.
Fiber:
Fiber supplements, such as Benefiber & Metamucil can be used, but only after you are drinking
64 oz. of fluid per day. You will get fiber from the fruits and vegetables you eat, once you are
beyond the full liquid phase.
Supplements to Prevent Constipation:
Probiotics
This supplement helps to regulate the digestive track.
Stool Softeners (such as DOSS)
Magnesium (200mg / day)
Smooth Move Tea
Fiber Supplements (once you are drinking >64 oz of fluid a day)
o Metamucil (sugar-free)
o Benefiber
o Efferpsyllium
o Fiber One
Supplements to Treat Constipation:
Milk of Magnesia
Miralax
140
Dumping Syndrome
With the RNY, your stomach no longer has a valve that releases stomach contents slowly into
the small bowel. Dumping syndrome is the result of the rapid emptying of foods high in sugar or
fat into the small intestine. When high concentrations of sugar or saturated fat hit the small
intestine, it causes an influx of fluid into the small bowel. This is less likely to happen with the
sleeve, but it certainly can, when eating inappropriately.
Symptoms can result within 10-30 minutes and can include:
Nausea
Diarrhea
Vomiting
Abdominal cramps
Bloating
Epigastric fullness
Sweating
Headache
Flushing
Lightheadedness
Palpitations (rapid heart rate)
A strong desire to lie down
Prevention
Simply avoid foods that are high in sugar or saturated fats and don’t drink with your meals.
Some patients may experience symptoms with full fat dairy products, though low fat dairy is
typically fine. Ice cream is typically not well tolerated.
High fat meats, like hot dogs may result in dumping.
Hypoglycemia
Reactive hypoglycemia or postprandial hypoglycemia (low blood sugar after meals) is a medical
term describing recurrent episodes of symptomatic hypoglycemia occurring 2-4 hours after a
high carbohydrate meal. The reason for this is that the body is producing more insulin than is
needed in response to a carbohydrate load.
Symptoms can vary and can include:
Increased or sudden hunger
Feeling shaky, dizzy or nervous
Pounding heartbeat
Drowsiness or feeling tired
Sweating (cold and clammy)
Numbness or tingling around the mouth
Headache and/or stomachache
Prevention
To prevent hypoglycemia, one should not eat carbohydrates without a protein. If you are
experiencing the above symptoms, try having a low fat dairy product, which contains a
combination of complex carbohydrates and protein. String cheese or low fat plain yogurts are
good choices.
141
When to Call
Call 911 for any unusual symptoms such as:
Chest pain
Severe shortness of breath
Severe dizziness
Severe headache
Call the Bariatric Nurse:
8:00 am – 4:00 pm Mon-Fri
425-502-3454
Toll-free 1-800-995-5658 Ext. 3450
Nausea, vomiting
Inability to eat or drink
Symptoms of dehydration
Constipation or diarrhea
Symptoms of wound infection
Any time you have a question or concern
o If you are concerned – it’s reason enough to call!
Consulting Nurse (after hours)
Toll-free 1-800-297-6877
If you experience any of the following:
Pain, tenderness, cramping, redness, tightness, or swelling in any part of your
leg or foot
Large amounts of drainage from your incision at anytime
Fever over 100.5 and/or shaking chills
Persistent nausea or vomiting
Severe diarrhea
3 to 4 day of constipation

142
Follow-Up Appointments & Lab Schedule
All follow up bariatric patients will follow the same schedule for
Follow-up labs:
Visit
Labs
Notes
Post-Op No Will also see the dietitian
2
-
3 Months
No
Will also see the dietitian
6 Months Yes (Fasting) Will also see the dietitian
12 Months
Yes (Fasting)
2 Years
Yes (Fasting)
3 Years Yes (Fasting)
4 Years
Yes (Fasting)
5 Years Yes (Fasting)
All Bariatric Patients:
Please do Fasting Labs at least 5 days prior to your appointment.
Labs are ordered in advance. There is no need to call for them to be ordered, simply go to
any Kaiser Lab for these to be done. If no order is in, please call 425-502-3454 (if you get
voice mail, please call 425-502-3450 - this phone is answered from 8 a.m. – 5 p.m.)
Appointment Line: 425-502-3450
Initial post op visit is typically with your surgeon. Remaining follow-up visits are typically with
one of our bariatric ARNP or PA’s.
All appointments are equally important – and are not just to review lab results.
Appointments with the surgeon, ARNP or PA are never done by phone. Two and 6 month
follow ups with the dietitian may be over the phone, if she is not available on the day of your
appointment with the provider.
The expectation is that patients commit to this follow appointment schedule. They are important
for your healthy recovery, they are important for us to know that you are doing well and they are
a requirement as a nationally accredited center for Bariatric Surgery.
Please call to make appointments a month or two in advance.
143
Labs needed:
Prior to all follow up appointments, except the initial post op and the 2 month visit
CBC
Comp. Metabolic Panel
PTH-intact
Lipoprotein Panel – (Fasting)
Vitamin B12
Vitamin A
Copper
Thiamin
25-hyroxy (Vitamin D)
Iron/TBIC (as needed)
HgbA1c – (if diabetic)
TSH
Prealbumin
Cooper
Zinc
If your primary care provider is not at a Kaiser Permanente Clinic (contracted)
provider:
You may do your labs with your own PCP
Please take this list of regularly ordered labs with you to that clinic/lab
Please do about 10 days prior to your appointment, if possible
Please remind provider that these need to be faxed to us, in advance your appointment:
Fax Number 425-502-3570
Your doctor may need to know the:
Diagnosis Code: Z98.84
144
Keys to Success after Bariatric Surgery
Use the TOOL you have been given
Listen to your body: When full – STOP eating
Follow the guidelines you are given
Follow the nutrition guidelines in section 6, for each phase of the diet
Do not go more than 5 waking hours without eating
Eat appropriate types
Protein first
Avoid refined carbohydrate foods
Healthy snack is ok
Separate foods and fluids
Wait 60 minutes after eating to drink fluids
NO GRAZING
Nibbling or snack throughout the day will add un-necessary calories and is a poor life
style habit
Work with your dietitian as directed
She is available by phone and email, in addition to the routine follow ups
Exercise
Start immediately after surgery
Find something that you enjoy
Make this a habit
Sleep
Get at least 6 hours of regular sleep, 8-9 hours is best
Helps to prevent weight regain
Make and keep your follow up appointments
Get follow up labs are directed
See section 9
Attend the support group
See section 2
Read the monthly newsletter
www.kp.org/bariatric-patients/
145
Food Journaling
Food journaling is one of the most powerful tools you can use to help you lose weight.
Your surgeon, ARNP/PA, dietitian, and bariatric nurse will all ask you about fluids, proteins, and
calories at just about every appointment or phone interaction. The reason for this is easy – it’s
vital that you know the grams of protein, the ounces of fluid and the number of calories that you
are taking in every day.
There are many different forms of journaling. You use a purchased food journal in book form,
any number of online journaling resources, word document or excel sheet, or simply a pad of
paper and a pen.
What to track:
Time of day
Grams of Protein
Main protein sources
Ounces and type of Fluids
Calories
Snacks
Food Portion (¼ cup, ½ cup, etc.)
Symptoms (nausea, pain or vomiting after eating, etc.)
Exercise
Vitamins & Supplements
Other things that may be helpful if you are experiencing symptoms:
Amount of time spend on the meal
Where and who you were with during the meal
o Sometimes we are most tempted in certain environments or with certain people
Emotions
o You are more likely to over eat when stressed or unhappy, etc.
Journaling can help you to:
Ensure adequate nutrition
See patterns
Be accountable
Yes, it takes time and effort, but the benefits that you will get out of this time and effort are well
worth it.
146
Web Page and Newsletter
http://www.kp.org/bariatric-patients
Bariatric page on the Kaiser web site
What you’ll find on this Web Page:
Monthly Newsletter (new one out on the first of each month)
Updated electronic copy of the Bariatric Notebook (Step’s to a Healthier Future)
Support Group announcement (date/time/speaker, etc.)
Food Journal printable document
Probiotic List
Vitamin Resources
Check out the many other hands, as this page continues to grow
Email link for questions
o (do not e-mail with personal medial questions to this e-mail address – use
kp.org/wa or call)
Newsletter
Monthly newsletter covers a different topic each month. These are topics that the bariatric team
feels are important to discuss. You are welcome submit suggestions of topics.
Monthly newsletter available on the first Monday of each month
The dates and time of upcoming Bellevue Kaiser Support Group
Upcoming newsletter topics are listed
New recipes each month
Program announcements or changes
Monthly Topic article
Much more…..
147
148
Emotions
You have taken a very important step towards improving your health. This life changing surgery
can have emotional as well as physical results. Healing from surgery is difficult. Initially you
experience pain, are limited in your activities, lack endurance and become easily fatigued. You
are changing one of the most basic behaviors of all, eating. You are unlearning things, some of
which you have done your whole life. Your feelings about yourself are changing, as perhaps
are feelings others have about you. It is normal to have many different emotions as these
changes happen. You may feel frustrated and angry as well as happy and proud. Each person
is unique and will have a different emotional experience.
As you recover
Be aware of your emotions
Acknowledge negative feelings
If possible, talk with family and friends when you are emotionally vulnerable
Set realistic expectations for yourself and others
Feelings of loneliness, isolation, and withdrawal are signs that may lead to depressions. Talk
with your family doctor or social worker if you feel that depression or anxiety is interfering with
your ability to cope. Behavioral Health Service counselors are also available. Call toll free 1-
888-287-2680 for more information. There are a variety of treatments available to help. See
the Behavioral Health Services brochure found in the back pocket of this booklet for more
information.
Please remember that, as you start this journey, it is not recommended that you change any
current treatment or therapy for depression or other mental health issues. Please work with
provider/therapist – and do not make changes without their advice.
149
If you have Sleep Apnea
Don’t just stop using CPAP/APAP/BiPAP
Procedure for post Bariatric Surgery APAP/CPAP/BiPAP withdrawal
1. The patient in conjunction with the surgical support team will establish a goal weight.
2. The first APAP download will be at 50% of Goal.*
A. If the 90th percentile APAP pressures on download is 6 cwp or less, a follow-up test
will be ordered to determine if OSA has resolved.
B. If download 90th percentile pressure exceed 6 cwp the patient will continue with
APAP use.
3. The second APAP download, if needed, will be at goal weight*
A. If the 90th percentile APAP pressures on download is 6 cwp or less, a follow-up test
will be ordered to determine if OSA has resolved.
B. If download 90th percentile pressure exceed 6 cwp the patient may still need to
continue with APAP. The download will be forwarded to the
sleep physician. He/She will determine if a follow-up test is appropriate.
Note: All Bariatric patients will be set up with an APAP with smart card or chip. This machine
will adjust the pressures as weight is lost. * If the patient was started on CPAP and not APAP,
an order for a 5 day autoset will be submitted to replace the download.
150
Hair Loss
Yes it can happen, though not all patients will experience hair loss. This is thought to be due to
the very low calorie diet, as it happens to those on very low calorie diets that have not had
bariatric surgery. Hair loss is temporary. As your calories increase, the hair loss will lessen
and stop over time.
For prevention:
Eat adequate protein daily
Take supplements as prescribed
Take Biotin 3000mcg-5000mcg daily (aka 3mg-5mg)
Avoid coloring and perming your hair
Can use products like Nioxin that help to prevent hair loss
o Found at hair salons and specialized beauty product stores
151
Excess Skin
This too can happen. The amount of excess skin after weight loss will depend on multiple
factors, to include how much weight you loss, genetics and muscle tone. It will be important to
keep the skin folds clean to prevent infection. If infections do occur, you should see your
primary care physician for evaluation and treatment and to ensure that these are documented in
your medical record. If you are interested in plastic surgery to remove excess skin, it’s
important to know that the only procedures that have a chance of being covered are the
abdominal pannus (panniculectomy) or breasts and that coverage is much like bariatric surgery,
in that it must be medically necessary. Surgeries for cosmetic reasons are rarely covered.
Some insurance contracts cover surgical procedures to remove excess skin when specific
criteria have been met. These criteria are different for varying insurance contracts. You can
discuss possible surgery with your primary physician who can place an authorization request for
you. These requests are then reviewed by the specific health plan to determine whether you
meet the criteria for coverage of the requested procedure. The most important thing you can do
is to receive proper care for any skin infections and have them documented in your medical
record.
There are also garments that can be purchased that will hold skin in place, if plastic surgery is
not something that you are interested in or your referral is denied.
152
Bariatric Resources
Books & Cookbooks
The Success Habits of Weight Loss Patients (Colleen Cook)
Never Going Back (Al Roker)
Weight Loss Surgery for Dummies
Weight Loss Surgery Cookbook for Dummies
Before and After: Eating Well After Weight Loss Surgery
The Everything Weight Loss Surgery Cookbook
The Good Life Weight Loss Surgery Cookbook
The Emotional First Aid Kit: A Practical Guide to Life After Bariatric Surgery (Cynthia
Alexander, PsyD)
Bounderies: When to Say Yes, How to Say No, to Take Control of Your Life (Dr. Henry
Cloud & Dr. John Townsend)
The Seven Habits of Highly Effective People: Powerful Lessons in Person Change
(Stephen Covey)
Small Bites: Daily Inspiration for Weight Loss Surgery Patients (Katie Jay MSW & J.
Persing)
Obesity Surgery: Stories of Altered Lives (Marta Meana, PhD & Lindsey Ricciardi, PhD)
Anatomy of a Food Addiction (Anne Katherine)
Magazines
Weight Loss Surgery Lifestyles
Health
Cooking Light
Fitness
Women’s Health
Men’s Health
Eating Well
Mindful
153
Online
Bariatricpal.com
Obesityhelp.com
Obesitygirl.com
Bariatriceating.com
Baribest.com
nawls.com (National Association for Weight Loss Surgery)
Obesity Action Coalition
Mindful Eating - Am I Hungry?
Sparkpeople.com
Thinner Times Bariatric Support Center
Facebook (see our newsletter for Kaiser Permanente patients Facebook page)
American Bariatric Support Group
Pinterest – Weight Loss Surgery Recipes
Overeatersanonymous.org
Online Journaling Resources
Fitday.com
Sparkpeople.com
Calorie-count.com
Thedailyplate.com
Livestrong.com
154
Weight Loss Surgery Poem
☼__________________________________________________☼
Do you have cookies in your car?
Are those chips not very far way?
Is that soda in your glass?
Was Weight Loss Surgery your choice to do?
Or did someone force you to do it?
If surgery was what you chose,
Why are you still doing all of those things?
Success begins with the wise choices that you make.
Don’t let noncompliance be your mistake.
The surgery you had was to assist you in changing.
Your compliance is for success long term.
So think before you decide to cheat.
Remember the goals you want to meet.
For surgery is not something you were forced to do.
It was what you wanted for a healthier you.
☼__________________________________________________☼
155
156
Glossary
A
Ambulation: Walking
Analgestics: Medicine that relieve pain
Anastomosis: A connection between tubular structures
Anesthesia: Medicines used during surgery or other painful procedures to block the ability to feel pain
Antibiotics: Medicine used to fight infections caused by bacteria
Anticoagulation Medicine: Medines used to delay blood clot formation. Sometimes referred to as ‘blood
thinners’
Arthritis: Inflammation of a joint usually accompanied by pain and frequently, changes in structure
B
Bariatric Surgery: An operation for control or treatment of obesity
Blood Clot: Collection of blood proteins and cells that forms a mess to slow or block the flow of blood
Blood Pressure: The amount of force pushing against the walls of blood vessels as blood flows through
them
Blenderized: See Pureed
C
Cardiac: Pertaining to the heart
Cardiologist: Physician specializing in treatment of heart disease
D
Diabetes: A disorder of carbohydrate metabolism characterized by increased blood glucose levels
resulting from inadequate production or utilization of insulin
Digestive Enzymes: Chemical substances that act on food causing it to break down to simpler
compounds for use by the body
Dumping Syndrome: A condition characterized by sweating and weakness after eating. Exact cause is
unknown, but rapid emptying into the small intestine is associated with the symptoms
157
E
Electrocardiogram (EKG): A record of the electrical activity of the heart
Endoscopically: A procedure by which a tube and a means for visualization are passed through a natural
body opening or incision to allow for inspection or manipulation
Embolism: A blockage of a blood vessel by an air bubble, blood clot or other foreign body
Electrolytes: Ions or elements in the body, including potassium, calcium, and magnesium that are
essential to life
G
Gallbladder: Sac attached to the liver for storage of excess bile
Gallstones: Lump of solid matter formed in the gallbladder
Gastroenterologist: Physician specializing in treatment of stomach, intestines and related structures such
as esophagus, liver, gallbladder and pancreas
Gastrografin Study: Xray of the stomach and surrounding structures
Graze: Continued sampling of small amounts of food
H
Hernia: Protrusion of an organ or tissue through an opening in its surrounding walls, especially the
abdomen
Hypertension: High blood pressure
I
Incentive Spirometer: A device used to induce deep breathing
Informed Consent: Agreement to undertake a course of action based on disclosure of complete
information
Intravenous Line: A small plastic tube inserted with a needle into a vein. The needle is removed but the
flexible tube remains in place and is attached by other tubing to a bag of fluids. The IV is used to give
fluids, medications and any blood products, as needed
IV: See Intravenous Line
J
Jejunum: The second section of the small intestine beginning about 8 to 11 inches from the stomach and
extending about 8 feet. The products of digested food are absorbed through the surface lining the
intestine
158
L
Laparoscopic Procedure: A technique which allows the surgeon to perform an operation through small
incisions and the use of an instrument by which to visualize the are of interest inside the body
Liver Enzymes: See Digestive enzymes
M
Marginal Ulcer: See Ulcer
Malaborption: Disordered or inadequate absorption of nutrients from the small intestine
N
Nasal Cannula A soft tube which directs oxygen to the nares of the nose
Nasogastric Tube: Soft plastic tube passed through the nose and throat into the stomach
NG Tube: See Nasogastric Tube
O
Open Procedure: Operative technique which provides full, unobstructed visualization and manipulation of
the areas of interest and surrounding tissues
Oxygen Saturation: Amount of oxygen in the blood available for use by the body
P
Pneumonia: Inflammation of the lungs
Postoperative: Events or activities occurring after a surgery or procedure
Pre-Operative: Events or activities occurring before a surgery or procedure
Pulmonary: Pertaining to the lungs
Pulmonologist: A physician specializing in diseases of the lungs
Pulse Oximeter: A device used to measure the amount of oxygen circulating in the blood
Pureed: To process and strain to make smooth
R
Reflux: A return or backward flow
Roux-en-Y Gastric Bypass: A type of operation performed to treat obesity by dividing the stomach to
reduce its size while maintaining absorption activities of the small intestine
159
S
Saline Lock: Site of IV that is disconnected from the tubing and bag and capped where a small plastic
tube enters the skin. Allows for continued access to the vein for the intermittent administration of fluids,
medications, or blood products without continuous infusion
Satiety: Sensation of being full especially of food
Sleep Apnea: Periods of not breathing occurring during sleep
Sleeve Gastrectomy: A type of operation performed to treat obesity by removing a portion of the stomach
to reduce its size while maintaining absorption activities of the small intestine
Stricture: A narrowing or constricture of the opening of a tube, duct or hollow organ
T
Transfusion: Transfer of blood or blood products
U
Ulcer: An open sore on the skin or any surface of the body
Ultrasound: The use of high frequency sound waves to outline the shape of various tissues and organs in
the body
V
Vital Signs: The indicators of the life processes such as temperature, heart rate, breathing rate and blood
pressure

160
Document Your Measurements
Jan Feb March
April May June July Augus
t
Sept Oct Nov Dec
Weight
Waist
Chest
Thigh
Arm
Wrist
Ankle
Calf
Neck
Hips
Shoe
Size
Dress
Size
Pant
Size
161
