
Page 1 of 34
Medical Coverage Policy: 0536
Medical Coverage Policy
Effective Date .................... 1/15/2024
Next Review Date .............. 1/15/2025
Coverage Policy Number ............. 0536
Prosthetic Devices
Table of Contents
Overview ............................................ 2
Coverage Policy .................................... 2
General Background ............................. 6
Appendix ........................................... 18
Medicare Coverage Determinations ....... 20
Coding Information ............................. 20
References ........................................ 27
Revision Details ................................. 34
Related Coverage Resources
Intraocular Lens Implant
Male Sexual Dysfunction Treatment: Non-
Pharmacogenic
Gender Dysphoria Treatment
INSTRUCTIONS FOR USE
The following Coverage Policy applies to health benefit plans administered by Cigna Companies.
Certain Cigna Companies and/or lines of business only provide utilization review services to clients
and do not make coverage determinations. References to standard benefit plan language and
coverage determinations do not apply to those clients. Coverage Policies are intended to provide
guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please
note, the terms of a customer’s particular benefit plan document [Group Service Agreement,
Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan
document] may differ significantly from the standard benefit plans upon which these Coverage
Policies are based. For example, a customer’s benefit plan document may contain a specific
exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s
benefit plan document always supersedes the information in the Coverage Policies. In the absence
of a controlling federal or state coverage mandate, benefits are ultimately determined by the
terms of the applicable benefit plan document. Coverage determinations in each specific instance
require consideration of 1) the terms of the applicable benefit plan document in effect on the date
of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including
Coverage Policies and; 4) the specific facts of the particular situation. Each coverage request
should be reviewed on its own merits. Medical directors are expected to exercise clinical judgment
where appropriate and have discretion in making individual coverage determinations. Where
coverage for care or services does not depend on specific circumstances, reimbursement will only
be provided if a requested service(s) is submitted in accordance with the relevant criteria outlined
in the applicable Coverage Policy, including covered diagnosis and/or procedure code(s).
Reimbursement is not allowed for services when billed for conditions or diagnoses that are not
covered under this Coverage Policy (see “Coding Information” below). When billing, providers
must use the most appropriate codes as of the effective date of the submission. Claims submitted
for services that are not accompanied by covered code(s) under the applicable Coverage Policy

Page 2 of 34
Medical Coverage Policy: 0536
will be denied as not covered. Coverage Policies relate exclusively to the administration of health
benefit plans. Coverage Policies are not recommendations for treatment and should never be used
as treatment guidelines. In certain markets, delegated vendor guidelines may be used to support
medical necessity and other coverage determinations.
Overview
This Coverage Policy addresses prosthetic devices. Prosthetic devices are defined as fabricated
items designed as replacements for missing body parts.
The policy statements below provide medical necessity criteria, including functional level
requirements where applicable, and coding information for the following:
• General Criteria for any Prosthetic Device
• External Facial Prosthetic Device
• Upper Limb Prosthetic Device (Myoelectric)
• Lower Limb Prosthetic Device (Microprocessor-controlled, Powered-microprocessor
controlled, Vacuum Suspension System)
• Repair and Replacement
For information regarding medical necessity criteria for any other prosthetic device please
reference the applicable Cigna Medical Coverage Policy:
• Breast Reconstruction Following Mastectomy or Lumpectomy
• Intraocular Lens Implant
• Male Sexual Dysfunction Treatment: Non-Pharmacogenic
• Gender Dysphoria Treatment
Coverage Policy
Coverage for prosthetic devices varies across plans. Please refer to the customer’s
benefit plan document to determine benefit availability and the terms and conditions of
coverage.
Microprocessor-controlled/computer-controlled/myoelectric devices are considered a
type of power enhancement/controlled device.
_____________________________________________________________________
GENERAL CRITERIA FOR A PROSTHETIC DEVICE
Functional Levels
Medical necessity for a lower limb prosthetic appliance is based on an individual’s
functional ability when using the prosthetic device. Functional ability is based on the
following classification levels:
Level 0: Does not have the ability or potential to ambulate or transfer safely with or
without assistance and prosthesis does not enhance his/her quality of life or mobility.
Level 1: Has the ability or potential to use prosthesis for transfers or ambulating on
level surfaces at fixed cadence; typical of the limited and unlimited household
ambulator.
Page 3 of 34
Medical Coverage Policy: 0536
Level 2: Has the ability or potential for ambulating with the ability to traverse
environmental barriers such as curbs, stairs or uneven surfaces; typical of the limited
community ambulator.
Level 3: Has the ability or potential for ambulating with variable cadence; typical of the
community ambulator who has the ability to traverse most environmental barriers and
may have vocational, therapeutic, or exercise activity that demands prosthetic
utilization beyond simple locomotion.
Level 4: Has the ability or potential for prosthetic ambulating that exceeds basic
ambulating skills, exhibiting high impact, stress, or energy levels; typical of the
prosthetic demands of the child, active adult, or athlete.
The following prosthetic devices are considered medically necessary when used to
replace a missing or nonfunctional body part and when applicable medical necessity
criteria listed below is met (Please note: prior authorization requirements may apply):
• External facial (e.g., nose, ear, midfacial, orbital, upper facial, hemifacial)
• Eye prosthesis (e.g., internal ocular, scleral shell)
• Lower extremity (e.g., foot, ankle, above/below knee)
• Upper extremity (e.g., finger, hand, wrist, above/below elbow, shoulder)
• Terminal devices, such as hands or hooks
Accessories to a prosthetic device are considered medically necessary when the
accessory is required for the effective use of the prosthesis.
Not Medically Necessary
The following prosthetic devices are each considered not medically necessary:
• a lower limb prosthetic device for functional level 0
• additions/components that are not required for the effective use of the device
• consumable supplies for the care of prosthetic device (e.g., cosmetics, creams, cleansers,
skin barrier wipes)
• prosthetic devices or additions/components not required for participation in normal
activities of daily living, including those that are chiefly for convenience, for participation in
recreational activities, or that otherwise exceed the medical needs of the individual (e.g.,
back-up/duplicate prosthetic devices, waterproof leg prosthesis [e.g., Water Leg, used for
showering, swimming])
_________________________________________________________________________________________
IRIS PROSTHESISs
An iris prosthesis (HCPCS code C1839) for the treatment of full or partial aniridia is
considered experimental, investigational or unproven.
_____________________________________________________________________
EXTERNAL FACIAL PROSTHESIS
An external facial prosthesis (HCPCS code L8040, L8041, L8042, L8043, L8044, L8045,
L8046, L8047 and L8048) is considered medically necessary when the prosthesis is
prescribed to compensate for the loss or absence of facial tissue as a result of disease,
injury, surgery or congenital defect.
A duplicate external facial prosthesis is considered a convenience item and is
considered not medically necessary.

Page 4 of 34
Medical Coverage Policy: 0536
Each of the following supplies related to the care of, and/or application or removal of,
an external facial prosthesis is a consumable item specifically excluded under most
benefit plans and considered not medically necessary:
• cosmetics
• skin creams
• skin cleansers
• adhesives
• adhesive remover
• skin barrier wipes
• tape
______________________________________________________________________
UPPER LIMB: MYOELECTRIC PROSTHETIC DEVICE
If a benefit is available for an upper limb myoelectric device the following medical
necessity criteria apply.
An upper limb myoelectric prosthetic device is considered medically necessary for an
individual with an amputation or congenital absence of a portion of an arm (e.g., hand,
forearm, elbow) when ALL of the following criteria are met:
• The individual has sufficient cognitive ability to successfully utilize a myoelectric prosthetic
device.
• The remaining musculature of the arm(s) contains the minimum microvolt threshold to
allow operation of a myoelectric prosthetic device.
• A standard body-powered prosthetic device cannot be used or is insufficient to meet the
functional needs of the individual in performing activities of daily living
An upper limb sensor and myoelectric controlled prosthetic device with simultaneous
multiple degrees of freedom (e.g., LUKE [Life Under Kinetic Evolution] Arm) is
considered experimental, investigational or unproven.
An upper limb prosthetic device using electromyography-based brain computer
interface (BCI) is considered experimental, investigational or unproven.
_________________________________________________________________
LOWER LIMB: MECHANICAL (NON-POWERED, NON MICROPROCESSOR)
The following lower limb additions and/or components are considered medically
necessary when the individual is functional level 3 or greater and medical necessity
criteria has been met for the base device:
• A flex-walk system or equal, all lower extremity prosthesis (HCPCS code L5981)
• a single axis, fluid swing and stance phase control (HCPCS L5828)
• a fluid stance extension, dampening feature, with or without adjustability (HCPCS L5848)
An adjustable stance flexion feature (HCPCS L5845) is considered medically necessary
when the individual is functional level 1 or greater and medical necessity criteria has
been met for the base device.
A high activity knee control frame (HCPCS code L5930) is considered medically
necessary for an individual who is functional level 4 and medical necessity criteria has
been met for the base device.

Page 5 of 34
Medical Coverage Policy: 0536
LOWER LIMB MICROPROCESSOR-CONTROLLED PROSTHETIC DEVICE
If a benefit is available for a microprocessor-controlled/computer-controlled lower limb
prosthetic, the following medical necessity criteria apply.
Any of the following microprocessor-controlled prosthetics, including
additions/components that are required for the effective use of the device (and
consistent with the user’s functional level), are considered medically necessary when
the individual is functional level 3 or greater:
• a microprocessor-controlled ankle-foot prosthetic (HCPCS code L5973) for a transtibial
amputee (below-the-knee)
• a microprocessor-controlled knee prosthetic (HCPCS code L5856, L5857, L5858) for a knee
disarticulation amputee or a transfemoral amputee (above-the-knee)
• a combination microprocessor-controlled prosthetic/system (e.g., SYMBIONIC
®
LEG 3,
LiNX
®
), when a microprocessor-controlled prosthetic knee alone is inadequate to meet the
functional needs of the individual (e.g., continued knee/foot instability due to
environmental/anatomical barriers)
A microprocessor-controlled prosthetic is considered not medically necessary for any
other indication.
An osseointegrated/osseoanchored lower limb prosthetic device is considered
experimental, investigational or unproven.
______________________________________________________________________
LOWER LIMB: POWERED MICROPROCESSOR-CONTROLLED PROSTHETIC DEVICE
If a benefit is available for a powered or power-enhanced lower limb prosthetic, the
following medical necessity criteria apply.
An endoskeletal knee-shin system (addition to a lower limb device) with powered and
programmable flexion/extension assist control, including any type of motor(s) (HCPCS
code L5859) (e.g., Össur Power Knee
™
) is considered medically necessary when ALL of
the following criteria have been met:
• Individual has a swing and stance phase type microprocessor controlled (electronic) knee
(HCPCS L5856)
• Is K3 functional level only*
• Has a documented comorbidity of the spine and/or sound limb affecting hip extension
and/or quadriceps function that impairs K-3 level function with the use of a
microprocessor-controlled knee alone
*Note: Coverage of this device is limited to individuals who are Functional Level 3; the
device is not intended for high impact activity, sports, excessive loading, or heavy duty
use.
The following powered prosthetic devices are each considered not medically necessary:
• a microprocessor-controlled ankle foot prosthetic with power assist (e.g., BiOM
®
Ankle,
emPOWER
™
Ankle [HCPCS L5973, L5969])
• a powered lower limb prosthetic for any other indication
______________________________________________________________________

Page 6 of 34
Medical Coverage Policy: 0536
LOWER LIMB: VACUUM SUSPENSION SYSTEM
A vacuum suspension system (e.g., vacuum-assisted socket system [VASS
™
]) (HCPCS
code L5781, L5782) is considered medically necessary to control residual limb volume
when there is contraindication to or failure of other socket-suspension systems (e.g.,
mechanical, passive suction) to adequately secure the limb to the prosthesis.
REPAIR AND REPLACEMENT
Repair and/or replacement of a medically necessary prosthetic device is considered
medically necessary for EITHER of the following indications:
• when anatomical change or reasonable wear and tear renders the item nonfunctional and
the repair will make the equipment usable.
• when anatomical change or reasonable wear and tear renders the item nonfunctional and
nonrepairable.
General Background
PROSTHETIC DEVICE
A prosthesis is an artificial device used to replace a missing body part and is intended to restore
normal function.
The following services and items are typically included in the allowance for a prosthetic device:
• the evaluation and fitting of the prosthesis
• the cost of base component parts and labor, as described in HCPCS base codes
• the repairs due to normal wear and tear during the 90-day period following the date of
delivery
• adjustments of the prosthesis or the prosthetic component made when fitting the
prosthesis or component and for 90 days from the date of delivery, when the adjustments
are not necessitated by changes in the underlying tissue or the patient’s functional ability
Prosthetic devices are secured or retained in place by harnesses or belts, by suction, or using
anatomical structures; some devices such as facial prosthetics are held in place with the use of a
skin adhesive. Additionally, devices may be held in place by implants, such as bone integrated
titanium implants.
U.S. Food and Drug Administration (FDA)
Prosthetic devices are subject to regulation by the FDA as medical devices. Prosthetic accessories
and limb components are classified by the FDA as Class I devices.
IRIS PROSTHESIS
An iris prosthesis is an implanted device recommended for treatment of partial or complete
aniridia. Aniridia is absence of the iris and may be associated with visual conditions such as glare,
photophobia, glaucoma, corneal opacification, and/or cataract formation.The degree of vision loss
varies. Treatment generally consists of contact lenses with iris prints and tinted eyeglasses. The
prosthetic iris device is made out of foldable medical grade silicone which is then custom-sized
and colored for each individual. The iris prosthetic is implanted surgically through a small incision,
it is then unfolded, the edges are smoothed out and it is then held in place by anatomical
structure of the eye or using sutures. It may be placed in the ciliary sulcus without sutures when
there is a pre-existing intraocular lens, implanted into the capsular bag with a new intraocular
lens, or can be sutured to the sclera, with or without an IOL. The device allegedly reduces
Page 7 of 34
Medical Coverage Policy: 0536
sensitivity to light while improving the appearance of the eye and visual acuity. Implant insertion
can be done alone or in combination with cataract or lens fixation surgery.
The CustomFlex™ Artificial Iris (Clinical Research Consultants, Inc., Cinn., OH [HumanOptics])
received premarket approval (P170039) by the U.S. Food and Drug Administration (FDA) in May
2018 as an artificial iris intended for use in children and adults for the treatment of full or partial
aniridia resulting from congenital aniridia, acquired defects, or other conditions associated with full
or partial aniridia. The device is available with or without embedded fiber mesh for implantation,
and may or may not be sutured. The FDA is requiring a post approval study to evaluate long term
safety outcomes up to three years postoperatively for adults and five years for pediatric subjects.
There is a growing body of evidence in the peer-reviewed scientific literature evaluating use of the
artificial iris. In general, sample populations are small, studies are retrospective, study populations
are heterogeneous, and surgical techniques vary precluding generalization of overall safety and
efficacy. Spitzer et al (2016) published the results of a retrospective case series involving 34
subjects who received a customized silicone iris prosthesis (Artificial Iris, HumanOptics, Germany)
after severe globe injury with total or sub-total iris loss. The Artificial Iris is a customized, silicone
prosthetic iris made from silicone material. The median follow-up was 24 months (range 12.0-
48.8). Five patients (15%) had pre-existing glaucoma and eight patients (24%) had pre-existing
hypotony. Mean visual acuity prior to artificial iris implantation was 1.1 logMAR (range 0.3-2.6). At
12 months after surgery 14 subjects had VA improvement between 0.2 and 2.1 logMAR units
(41%), 11 subjects had a VA change of less than 0.2 logMAR units (32%), and nine subjects had
a reduction of VA between 0.2 and 1.4 logMAR units (27%). Visual acuity 12 months after surgery
was 1.4 logMAR (range 0.2-2.6); median VA was unchanged. Complications included newly
diagnosed glaucoma (9%) and hypotony (9%), persisting intraocular inflammation (8.8%),
macular edema (11.8%), and corneal endothelial decompensation requiring corneal
transplantation (18%). Patients' satisfaction increased by reducing photophobia and enhanced
cosmetic appearance; 15 subjects had reduced subjective glare and while a majority of subjects
were satisfied with functional and cosmetic results (80%), three continued to have persistent
glaring or deteriorating vision and were not satisfied. Limitations of the study small sample
population, short-term outcomes, lack of a statement regarding subjective discomfort due to
glaring from 14 subjects (information was only available for 20 subjects at follow-up).
Mayer and colleagues (2016) reported results of a prospective case series investigating functional
results and patient satisfaction after surgical iris reconstruction. Thirty-seven consecutive patients
with traumatic iris defects, presenting from 2011 through 2014 who underwent pupillary
reconstruction with a new artificial iris implant (Artificial Iris, HumanOptics, Germany), were
included in the study. The main outcome measures included change of best-corrected visual acuity
(BCVA), intraocular pressure (IOP), pupillary aperture, glare, contrast sensitivity, endothelial cell
density, anterior chamber depth, anterior chamber angle, and patient satisfaction. Thirty-two eyes
of 32 patients (mean age, 52.9±16.0 years) were included. After implantation and during follow-
up, BCVA and IOP did not change significantly (BCVA, 0.77±0.62 logarithm of the minimum angle
of resolution [logMAR] preoperatively vs. 0.68±0.64 logMAR 1 month postoperatively [P = 0.792];
(IOP, 14.94±3.55 mmHg preoperatively vs. 17.72±5.88 mmHg 1 month postoperatively [P =
0.197]). The pupillary aperture was reduced significantly (42.11±20.1 mm(
2
) to 8.7±0.3 mm(2);
P < 0.001). Contrast sensitivity increased significantly (0.80±0.51 to 0.93±0.49; P = 0.014).
Endothelial cell count revealed a significant decrease postoperatively (1949±716 per 1 mm(
2
) to
1841±689 per 1 mm(2); P = 0.003). Anterior chamber depth (4.03±1.06 mm preoperatively vs.
4.29±0.70 mm postoperatively; P = 0.186) and angle (43.2±13.5° preoperatively vs. 40.5±10.8°
postoperatively; P = 0.772) showed no significant differences. Subjective impairment through
glare (9.12±1.62 preoperatively vs. 3.07±2.29 postoperatively; P < 0.001) and cosmetic
disturbance (6.33±3.21 preoperatively vs. 1.58±0.86 postoperatively; P < 0.001) improved
significantly. Overall patient satisfaction was 8.91±1.51 of 10 points on an analog scale. The
Page 8 of 34
Medical Coverage Policy: 0536
authors concluded that the implantation of the artificial iris is an effective therapeutic option for
the treatment of traumatic iris defects and results in an “individual, aesthetically appealing, and
good functional outcome in addition to high patient satisfaction”. Limitations of the study as noted
by the authors include five subjects excluded from follow-up, and inclusion of subjects with
varying iris defects.
Rickman et al. (2016) reported a retrospective interventional case series of 34 patients who
received an artificial iris between 2004 and 2013 using the Artificial Iris (HumanOptics, Germany).
Only eyes with a minimum follow-up period of 2 years were included, subjects ranged in age from
28-85 years. Indications for treatment were congenital, traumatic, or iatrogenic complete or
partial aniridia. The artificial iris was implanted either with or without embedded fiber mesh for
partial or full prostheses. Mean followup was 50.0 months (SD ±18.9 months). Repositioning of
prostheses was not required in any of the 34 cases. In cases of keratopathy (17.6 %) visual
function increased from baseline mean 1.6 logMAR (SD ±0.7) to 1.2 logMAR (SD ±0.7) after
artificial iris implantation. The remaining iris tissue darkened during the follow-up in 23.5 % (83.3
% with and 10.7 % without mesh), 8.8 % developed glaucoma (50 % with and 0 % without
mesh) and 14.7 % needed consecutive surgery after prostheses implantation (50 % with and 7.1
% without mesh). In three out of seven trauma cases (42.9 %) silicone oil was spilled into the
anterior chamber after 2.5 years, on average. When the VA at baseline was compared to the final
examination, 16 eyes gained two or more VA lines, 15 eyes remained stable and 3 eyes lost two
or more VA lines. There was no significant difference in the mean IOP when baseline was
compared to final examination. According to the authors, the artificial iris prosthesis revealed a
good clinical outcome in terms of long-term stability, cosmetic appearance and visual function.
Limitations noted by the authors included a wide range of aniridia causes and variation in disease
and management. Therefore, direct correlation of the success rate and the surgical technique is
not firmly established. Furthermore, the authors acknowledged long-term complications such as
glaucoma, over-pigmentation of the remaining iris tissue, and need for a secondary surgery are
significantly associated with implants with integrated fiber mesh, however not to implants without
mesh.
Mostafa and associates (2018) evaluated the limitations and benefits of the BrightOcular
prosthetic artificial iris (Stellar Devices) device in management of aniridia associated with aphakia
or cataract. Designed as a retrospective study, the authors evaluated 5 eyes of 4 patients (ages
12, 13, 28 and 34 years) who underwent implantation of the BrightOcular iris prosthesis (Stellar
Devices) for total or partial aniridia. Similar to the HumanOptics prosthesis, this device is silicone,
yet not FDA approved. The study group included 2 eyes of 1 patient with congenital aniridia
associated with congenital cataract, and 3 eyes with traumatic aniridia (1 with subluxated
cataractous lens and 2 with aphakia). The iris prosthesis was implanted after a 3-piece acrylic
intra-ocular lens (IOL) was implanted in all cases. Measured outcomes included intra-operative
and post-operative complications, and the cosmetic satisfaction and evaluation of the clinical
course for at least six months. Uncorrected distance VA and best-corrected distance visual acuity
(BCVA) improved for all subjects. All patients had a transient corneal edema that resolved within
the 1st post-operative week. Only the patient with congenital aniridia had a permanent increase
in IOP and developed a band keratopathy throughout a 2-year follow-up period. The prosthesis
was well-centered in all eyes except for 1 case that needed scleral suture fixation after 3 months.
One case required scleral suturing due to intraoperative displacement. In the authors opinion both
cases were the result of improper sizing of the device. It was reported all subjects had a
satisfactory cosmetic appearance, and improvement in glare and halos. The authors concluded
that the BrightOcular iris prosthesis was a safe and useful tool to correct aniridia associated with
pseudophakia or aphakia. In addition, more research is required to determine the best means of
sizing the implant and to address the problem of post-operative IOP rise; further studies should
also examine the safety of the prosthesis in clear phakic eyes. Limitations of the study include the
small sample population and retrospective study design.
Page 9 of 34
Medical Coverage Policy: 0536
Mayer, et al. (2018) retrospectively evaluated the learning curve of the implantation surgery for
the iris prosthesis and potential complications. A total of 51 subjects were implanted with the
Artificial Iris, (HumanOptics, Germany), follow-up occurred at least three months post procedure
and extended to a maximum of four years. Complications were grouped into categories of none,
mild (with full recovery) or moderate (without full recovery) and severe (required surgical
intervention). The overall complication rate was 25.5% (13/51 subjects). Mild complications
included recurrent bleeding with rise in IOP (n=1), slight but stable iris deviation (n=2), capsular
fibrosis (n=2); moderate complications included suture cutting through the residual iris (n=1),
new onset glaucoma (n=3), and corneal decompensation (n=5); severe complications included iris
suture loosening (n=2), and dislocation (n=3), synechiae (n=2), glaucoma (n=2), and corneal
decompensation (n=5), with need for surgery, cystoid macular edema (n=3) and retinal
detachment (n=1). The complication rate decreased from 83.3% in the first year to 13.3% in the
fourth year. The author group concluded implantation of the artificial iris implant requires
significant surgical experience, should be limited to specialized centers, and requires careful
postoperative management to detect unexpected adverse events.
Yoeruek and Bartz-Schmidt (2019) reported the results of a small case series involving five
subjects with traumatic aniridia, combined with aphakia and corneal scars or graft failure, who
received an intraocular lens attached to a customized silicone iris prosthesis (Artificial Iris,
HumanOptics). The mean age of the subjects was 46.2 years and the mean follow-up was 24.6
months. The mean BCVA improved from 1.36 logMAR before surgery to 0.78 logMAR after surgery
during the follow-up. Data on glare and photophobia was available for three subjects; in three
glare sensation was reduced. Postoperative complications included one graft failure during the first
year after surgery. Three subjects had glaucoma prior to surgery; two were able to be controlled
sufficiently postoperatively. There was no new cases of glaucoma postoperatively. At the last
follow-up visit, the artificial iris-IOL complex was well-centered with good positioning in all
cases. The authors concluded that management of post-traumatic aniridia combined with aphakia
and corneal scars or graft failure by haptic fixation of a foldable IOL on an artificial iris combined
with a simultaneous keratoplasty appeared to be a promising approach, which allowed to correct a
complex lesion with a less traumatic and faster procedure. The study is limited by the small
sample size, retrospective design and short term follow-up.
Mayer and colleagues (2019) reported the results of single center case series to evaluate the
effect of an artificial iris implant on a remnant iris (n = 42). Morphologic evaluation was carried
out over 24 ± 14 months. Main outcome measures included remnant pupillary aperture, iris color,
VA, IOP, and endothelial cell count (ECC). Retraction syndrome, manifest by progressive
enlargement of the pupil and retraction of the residual iris, was detected in seven of 42 (16.7%)
eyes following implantation of the artificial iris prosthesis. Residual iris aperture dilated from 36.6
± 15.4 mm
2
pre-operatively to 61.1 ± 12.5 mm
2
one year post-operatively (66.9 % increase). In
5 of 7 affected eyes, the artificial iris had been implanted into the ciliary sulcus; in 2 eyes it had
been sutured to the sclera. A total of 4 of the 7 subjects presented with remarkable complications:
2 eyes needed glaucoma shunt surgeries owing to pigment dispersion; 1 suffered from recurrent
bleeding; and in 1 case artificial iris explantation was performed owing to chronic inflammation
and elevated intraocular pressure. Anterior chamber depth (ACD) and angle, ECC, and VA did not
change in this cohort. Changes in color were not observed in the remnant iris. The authors
concluded that the implantation of an artificial iris prosthesis could lead to a residual iris retraction
syndrome as a late complication. It was likely that residual iris was trapped in the fissure
between the artificial iris and the anterior chamber angle, preventing further pupil
constriction. Another possibility noted by the authors could be the result of a constriction or
atrophy of the residual iris. Due to the small sample population the authors were unable to
determine statistical comparisons regarding different implantation methods. They concluded that
Page 10 of 34
Medical Coverage Policy: 0536
with increased use of the artificial iris more cases of iris retraction syndrome may be detected in
the future.
Figueiredo and Snyder (2020) retrospectively evaluated the safety and effectiveness of the
CustomFlex device when used to treat photic symptoms in individuals with congenital aniridia
(n=50 subjects, 96 eyes). Mean follow-up was 44 months (36 ± 36 months). Measured outcomes
included pre and post-operative data regarding corrected distance visual acuity (CDVA), subjective
photophobia and glare, keratopathy, glaucoma, IOP, glaucoma drops, and other comorbid
pathologies. Additional postoperative data regarding postoperative complications, prosthesis
decentration, and further surgeries was also collected. In all cases, additional procedures were
performed at the time of implantation, including phacoemulsification, intraocular lens (IOL)
implantation repositioning or replacement, limbal relaxing incision, keratectomy (superficial and
lamellar) or vitrectomy. Intraoperative complications were reported in 14 eyes (14.6%). A total of
95.7% (89/93) reported a reduction in photophobia symptoms, 3.2% (3/93) reported no change
in symptoms and 1.1% (1/93) reported worsening of symptoms. Similarly, subjective reporting of
glare indicated a reduction of symptoms in 95.2% of subjects (79/83), 3.6% (3/83) reported no
change in symptoms and 1.2% (1/83) reported worsening of symptoms. When individuals could
not reliably report their symptoms, family member observations of behaviors was used to gauge
functional improvement in photic symptoms. When preoperative visual acuity was compared to
best achieved postoperative visual acuity, it was found that 72 eyes (75.0%) gained at least 2
lines and 24 eyes (25.0%) stayed within 2 lines, whereas no eye lost 2 or more lines. When
compared with last measured visual acuity 58.3% (56) of the eyes improved 2 or more lines,
32.3% (31) of the eyes stayed within two lines of preoperative measurements, and 9.4% (9) of
the eyes dropped two or more lines. The declines in the VA in the postoperative period were
attributed to underlying comorbidities, which included worsening of the ocular surface, aniridia
fibrosis syndrome, retinal detachment, and posterior capsule opacification. Aniridic keratopathy,
which was present in 84.4% (81) of the eyes preoperatively, was present in 85.4% (82) at last
visit (28.4% [23] of the eyes with preoperative keratopathy had progression of the disease).
Aniridic glaucoma was present in 33.3% (32) of the eyes preoperatively in comparison with 51.0%
(49) of the eyes at last visit (53.1% [17] of the eyes with preoperative glaucoma had progression
of the disease). Additional complications included aniridia fibrosis syndrome (AFS) (3.1%),
prosthesis decentration (9.4%), choroidal folds/effusion secondary to ocular hypotony (2.1%),
retinal detachment (1.0%), cystoid macular edema (1.0%) and vitreous hemorrhage (1.0%).
Overall 33.3% (32) eyes required additional surgical intervention. In the authors opinion
individuals with congenital aniridia syndrome present with highly complex eyes which require an
individualized approach and long-term follow-up. Limitations noted by the authors included
significant heterogeneity related to ariridic pathology within the group.
Ayers et al., (2022) reported the results of a prospective, nonrandomized trial evaluating safety
and efficacy of the CustomFlex Artificial Iris for treatment of partial or complete, congenital or
acquired, iris defects of various causes. Inclusion criteria were 22 years of age or greater,
congenital or acquired iris defect and photophobia, glare sensitivity, or both, and pseudophakia,
phakia, or cataract in the study eye. The initial cohort involved 180 subjects, afterwards eligible
adults were enrolled in a continued access cohort until the device received premarket approval
from the FDA. Following at least four weeks post initial eye implantation fellow eye implantation
was performed in 28 subjects. A compassionate use cohort (n=89) was also followed as part of
the study protocol for individuals who did not meet one or more of the inclusion criteria. The
authors reported subjects were reexamined one day following surgery and one week, one, three,
six and 12 months after surgery. Three different techniques were used: (1) passive fixation within
the capsular bag, (2) passive fixation within the ciliary sulcus, and (3) active suture fixation to
residual iris tissue, the sclera, or an IOL that, in turn, was sutured to the sclera. Primary efficacy
outcomes included a decrease in the severity of patient-reported photosensitivity (i.e., daytime
and nighttime light sensitivity and daytime and nighttime glare), improvement in health-related
Page 11 of 34
Medical Coverage Policy: 0536
quality of life, and improvement in postoperative cosmesis. Primary safety outcomes included
cumulative IOL-related adverse events, cumulative surgery-related adverse events, and device-
related adverse events. Secondary safety outcomes were tabulated and reported at the various
study intervals and included changes in vision (CDVA, uncorrected distance visual acuity [UDVA],
and manifest refraction), IOP, ECD, and slit-lamp observations. Endothelial cell density was
measured at the screening visit and at 6 and 12 months after surgery if no corneal scarring,
edema, or other pathologic features precluding measurement were present and was recorded as
the average of three measurements obtained by noncontact specular or confocal microscopy.
Results demonstrate a 59.7% reduction in marked to severe daytime light sensitivity (P <
0.0001), a 41.5% reduction in marked to severe nighttime light sensitivity (P < 0.0001), a 53.1%
reduction in marked to severe daytime glare (P < 0.0001), and a 48.5% reduction in severe
nighttime glare (P <0.0001). A 15.4 point total score improvement was demonstrated in vision-
related quality of life as measured by the 25-item National Eye Institute Visual Function
Questionnaire (NEI VFQ-25) (P < 0.0001), and 93.8% of participants rated an improvement in
cosmesis on the Global Aesthetic Improvement Scale at the 12-month postoperative examination.
There was no loss of CDVA of > 2 lines related to the device. Median ECD loss was 5.3% at 6
months after surgery and 7.2% at 12 months after surgery. The authors concluded that the
artificial iris surpassed all key safety end points and met all key efficacy end points and is
therefore safe and effective for the treatment of symptoms and an unacceptable cosmetic
appearance created by iris defects. Limitations of the trial include short term followup of 12
months.
The National Institute for Health and Care Excellence (NICE) published interventional procedures
guidance for artificial iris insertion as treatment for acquired aniridia (NICE, 2020). NICE reviewed
evidence consisting of one non-randomized comparative trial, seven case series, and one case
report. The primary efficacy outcomes included reduction in symptoms of glare, improvement in
visual acuity, quality of life and other patient-reported outcomes. Key safety outcomes included
need for explantation, infection, worsening visual acuity, glaucoma, and implant displacement.
Within this document NICE concluded the “evidence on the safety and efficacy of artificial iris
implant insertion for acquired aniridia is limited in quantity and quality. Therefore, this procedure
should only be used with special arrangements for clinical governance, consent, and audit or
research.
Other implants have been investigated in the medical literature, however FDA approvals were not
found on the FDA site (e.g., BrightOcular implants, a newer generation of NewColorIris
®
, [Stellar
Devices, New York, NY] and used for cosmetic purposes) and Ophtec Artificial Iris Model C1 [Reper
– NN, Distributed by Ophtec BV, European Union]). Some of the cosmetic devices have been
associated with a high incidence of serious complications such as corneal decompensation,
glaucoma, native iris trauma, intraocular inflammation, and cataract development, which may
result in permanent structural damage or visual impairment (Ghaffari, 2021).
An ongoing clinical trial can be referenced at the National Library of Clinical Trials, it is a parallel
non randomized study evaluating the safety and efficacy of the CustomFlex Artificial Iris for
treatment of iris defects (NCT01860612). Although promising, evidence in the peer reviewed
scientific literature evaluating use of the artificial iris prosthesis has not firmly established safety
and efficacy of the device. Professional society statements regarding use of the device as
treatment for anridia from the American Academy of Ophthalmology and American Association for
Pediatric Ophthalmology were not found. Within the clinical studies several authors have reported
high complications rates, both intra and post-operatively. As a result strong evidence based
conclusions regarding safety and efficacy cannot be made. Additional clinical studies with longer
followup are needed to evaluate use of the device and impact on health outcomes.
EXTERNAL FACIAL PROSTHESIS

Page 12 of 34
Medical Coverage Policy: 0536
External facial prostheses are used to replace lost or absent facial tissue that is the result of
disease, injury, surgery or a congenital defect or they may be considered an alternative to
reconstructive surgery. An external device is usually made from silicone materials and requires
frequent removal and cleaning while a surgically implanted prosthetic device is typically removed
and cleaned less often. The function of the external prosthesis is to protect exposed tissues, cover
exposed cavities, and restore physical appearance.
Common types of external facial prostheses include the following:
• auricular (ear) - restores all or part of the ear, function includes directing sound into the
auditory canal; supporting eyeglasses and acting as a hearing aide if required.
• nasal (nose) - restores all or part of the nose and may include the nasal septum; functions
to direct airflow to the nasopharynx and may also provide support for eyeglasses
• midfacial (nose and adjacent tissues) - restores part or all of the nose and significant
adjacent facial tissue/structures, does not include the orbit or any intraoral maxillary
prosthesis; adjacent facial tissue/structures include one or more of the following: soft
tissue of the cheek, upper lip, or forehead.
• orbital (orbit/eyelids) - restores the eyelids and the hard and soft tissue of the orbit, may
include the eyebrow; functions to house the artificial eye, does not include the ocular
prosthesis
• upper facial (orbit and adjacent tissues) - restores the orbit, plus significant adjacent facial
tissue/structures, does not include the nose, any intraoral maxillary prosthesis or ocular
prosthesis; adjacent facial tissue/structures include soft tissue of the cheek(s) or forehead.
• hemifacial (nose, orbit and adjacent tissues) - restores part or all of the nose, the orbit,
and significant adjacent facial tissue/structures, does not include any intraoral maxillary
prosthesis or ocular prosthesis.
• partial facial prosthesis - restores a portion of the face, does not specifically involve the
nose, orbit or ear
• nasal septal prosthesis - prosthesis that occludes a hole in the nasal septum, does not
include superficial nasal tissue
Prosthetic devices may be secured or retained in place by anatomical structures; however, in most
cases the device is held in place with the use of a skin adhesive. Additionally, some devices may
be held in place by implants, such as bone integrated titanium implants. The method chosen to
secure the device and the type of device are usually dependent upon factors such as the degree of
deformity, the person’s ability to handle maintenance routines, the individual’s occupation and
lifestyle, and the availability of assistance when needed.
Skin care products (e.g., cosmetics, creams, and cleansers) related to care of the prosthesis, and
the application and/or removal of the device are considered personal care items.
UPPER LIMB: Myoelectric Prosthetic Device
The conventional prosthetic appliance for replacement of an upper extremity, either below or
above the elbow, is a body-powered prosthesis with a terminal hand or hook device. A myoelectric
device functions by means of electrical impulses and operates on rechargeable batteries requiring
external cables or harnesses. It is a prosthetic device used as an alternative to a passive or
conventional body-powered device which enables an amputee to adjust the force of his/her grip
and an ability to both open and close the hand voluntarily. Myoelectric devices may be
recommended for amputees who are unable to use body-powered devices or who require
improved grip function/motion for performance of daily activities. Adults or children with above- or
below-the-elbow amputations may use the device effectively, although as a child grows the
prosthesis may require multiple socket replacements for proper fit and function.

Page 13 of 34
Medical Coverage Policy: 0536
A hybrid prosthesis is a device that uses a combination of myoelectric and body-powered
technology to enhance the amputee's overall functionality, depending on the level and location of
amputation. A hybrid device is indicated for high level amputations, (i.e, at or above the elbow)
and consists of a body-powered device to control shoulder and elbow movement and a myoelectric
device to control hand and wrist motion, allowing control of two joints at one time.
Literature Review
Results of studies published in the peer-reviewed scientific literature evaluating the impact of
these devices on clinical outcomes are mixed. Evidence is primarily in the form of case series and
does not provide strong conclusions to support the use of these devices for improving quality of
life, although some authors have reported greater function and range of motion among subjects
using the device. In general, the reported outcomes are subjective and there is little data
regarding outcomes such as functional status, studies with direct comparisons to body-powered
devices or passive devices is limited. Moreover, patient selection criteria are not clearly defined.
However, despite these and other confounding variables, the published literature does lend some
support in clinical benefits from the use of a myoelectric prosthesis.
Areas of development for powered upper limb prosthetic devices include devices that function
using implantable sensors, reinnervation of muscle fibers to allow fine movement control as well
as sensory feedback and multiple simultaneous degrees of freedom. The LUKE (Life Under Kinetic
Evolution) Arm (Mobius Bionics, LLC) is an upper limb prosthesis that has been developed to
restore function in individuals who have lost all or part of their upper limb and has multiple
powered joints and grip patterns and is capable of multiple simultaneous degrees of freedom,
controlled using EMG signals. In addition to the EMG electrodes, the LUKE Arm contains a
combination of mechanisms, including switches, movement sensors, and force sensors. The
primary control resides with inertial measurement sensors on top of the feet. The micro-
electromechanical control system is operated through an inertial measurement unit (IMU), which
is located in a sensor that is attached to or embedded in the individual’s shoe. The user
commands motion of the prosthesis by moving the foot in various directions. The device is
available for transradial, transhumeral or shoulder amputation. Nevertheless the evidence in the
peer reviewed literature is insufficient to support safety and efficacy of these emerging-type of
devices.
Upper limb devices (HCPCS L6880, L6935) using electromyography-based brain computer
infterface are being investigated. These devices reportedly function by gathering brain activity or
information in order to trigger movement. One device, the Esper Hand (Esper Bionics Inc., New
York) has five moveable digits which can allow multiple grips and movements of rotation
promoting the ability to perform everyday tasks in addition to a computer or smartphone platform
that collects and stores information regarding the users movements. By doing so it can assume
what the users next action would be allowing it to predict movements more rapidly. Evidence in
the scientific peer reviewed literature evaluating brain based computer interface for upper limb
prostheitc deivices is insufficient to support safety and efficacy at this time.
LOWER LIMB
Prior to being fitted with a lower limb prosthetic device, the individual must demonstrate specific
functional levels. A functional level is defined as a measurement of the capacity and potential of
the individual to accomplish his/her expected post-rehabilitation daily function.
Lower limb prosthetic devices may be preparatory or permanent. A preparatory device is a
prosthesis made soon after an amputation (approximately four weeks) as a temporary method of
retraining a person to walk and balance while shrinking the residual limb. A permanent prosthesis
is recommended when an individual has used a prosthetic device full time for a period of six

Page 14 of 34
Medical Coverage Policy: 0536
months and when the limb volume has stabilized to a point where the socket fit remains relatively
consistent for 2–3 weeks.
Components and/or additions to a prosthesis may be medically necessary; the determination of
medical necessity is based on the person’s functional ability and expected functional potential as
defined by the prosthetist and the ordering physician. Additional documentation supporting
medical necessity must accompany claims submitted for prosthetic components and/or additions.
Customizing prosthetic devices with enhanced features is not medically necessary if activities of
daily living can be met with standard devices.
Accessories that are necessary for the effective use of the prosthetic device may also be
considered medically necessary devices. Accessories that are not necessary for the effective use of
the device are considered not medically necessary. While some prosthetic manufacturers offer
devices with waterproof features, including devices that are submergible (e.g., Water Leg,
[Standard Cyborg, SF, CA] [used for showering, swimming], Genium X3 [Ottobock, US], [a
waterproof microprocessor-controlled knee prosthetic device]), when used for recreational
purposes these prosthetic accessories/devices are considered a convenience item and not
medically necessary.
LOWER LIMB Osseointegrated Prosthesis
Additionally, more advanced technological systems using multiple sensors to send messages back
to a microchip regarding changes in walking patterns and osseoanchored prosthetic devices for
lower limbs are being investigated. These devices represent emerging technologies and are
undergoing clinical trials evaluating performance, safety and durability. In contrast to the standard
of care socket-suspended prosthesis, an osseoanchored prosthetic device consists of a fixture and
abutment screw that is surgically implanted into bone. After healing and various stages of
rehabilitation the fixture is then attached to a prosthesis. One such device, the OPRA™ Implant
System (Integrum AB, Sweden), has received FDA approval as a humanitarian device for
prosthetic use. According to the manufacturer the system consists of three parts; an anchoring
element (the Fixture) and a skin penetrating connection (the Abutment), and a securing titanium
screw (the Abutment Screw). FDA labeling indicates the intended use is for patients who have
transfemoral amputation due to trauma or cancer and who have rehabilitation problems with, or
cannot use, a conventional socket prosthesis. The OPRA device is intended for skeletally mature
patients. A systematic review published in 2018 by Kunutsor and colleagues evaluating the safety
and efficacy of osseintegrated prostheses included a total of 22 eligible articles; 13 of the studies
were unique. The average sample size of the studies included ranged from 11 to 100 participants,
none of the studies were RCTs. The reported outcomes of all studies supported improvement in
functional outcomes (walking ability, prosthetic use and mobility), and satisfaction and quality of
life following osseointegration, compared with their preoperative status or when using a
conventional socket prosthesis. Infection rates varied from 1% to 77%, with the majority of
infections described as low-grade soft tissue or superficial infections related to the skin–implant
interface. Infections were treated effectively with antibiotics. According to the authors none of the
studies reported additional amputation or death as a result of osseointegration and they concluded
osseointegration following limb amputation improved prosthetic use, comfort when sitting, walking
ability, mobility, gait and quality of life. However, use of such devices is associated with an
increased risk of soft tissue infection.
In 2017 the Canadian Agency for Drugs and Technologies in Health (CADTH) published a
systematic review to evaluate the evidence for osseointegrated prosthetic devices for lower limb
amputation. After reviewing seven studies that met inclusion criteria, the authors concluded the
quality of evidence is generally low, and while some evidence suggests there is improvement in
quality of life, function and mobility after implantation there is concern regarding high rates of
infection, and the design of and materials used affecting safety and efficacy. Overall, the authors

Page 15 of 34
Medical Coverage Policy: 0536
reported the available evidence suggests that careful attention should be given to patient
selection, implant selection, and residual limb skin integration, as well as surgical and
rehabilitation protocols, to optimize outcomes and reduce adverse event rates.
LOWER LIMB: Vacuum Suspension System
Suspension systems for lower limb prostheses keep the prosthesis in place, ensuring a good fit
between the socket and residual limb. The intended function is to provide a connection that
reduces rotational and shearing forces which can result in skin breakdown as well provide for
balance and steady gait. Various types of suspension systems are available and include those that
are primarily mechanical or suction-type systems. Mechanical systems involve the use of belts,
straps, or sleeves, for example, to attach the device to the residual limb (L5666, L5670-L5672).
Suction-type systems function by way of a negative pressure created between the socket and
insert/liner. These devices can be passive (air escapes while donning via a one-way valve) or
active (suction pump evacuates the air). Passive systems involve the use of a soft liner, a one-
way valve and a donning sleeve. A liner is placed over the limb, the limb is placed in the socket
and the force of one’s body weight upon standing expels excess air through the valve creating a
seal. With active suction devices the sleeve creates a seal around the edge of the socket and a
pump and exhaust remove the excess air between the socket and the liner to ensure a secure fit.
Various vacuum suction-type devices (mechanical or electrical) are available and include the
Vacuum-Assisted Socket System (VASS
™
) (Otto Bock Harmony Vacuum-Assisted Socket System,
Otto Bock HealthCare; Minneapolis, MN), the eVAC® (Smith, Global), and the LimbLogic ™ VS
prosthetic vacuum suspension system (Mount Sterling, Ohio). Each device is a vacuum suction-
type suspension system that manufacturers claim helps control volume fluctuation in the residual
limbs of lower-extremity amputees, reduces forces to the limbs, and improves both suspension
and proprioception without restricting vascular flow. Although patient selection criteria have not
been firmly established, the device has been proposed for individuals with non-healing skin
ulcerations located on the stump and/or when other socket systems have failed to provide a
secure fit.
Evidence in the published, peer-reviewed scientific literature evaluating suspension systems, in
particular vacuum suction–type suspension systems is limited. Much of the published literature is
in the form of feasibility trials, case reports, and uncontrolled case series involving small
populations. Reported outcomes are mixed, are short term, lack high statistical power and cannot
be generalized. The results of one published randomized trial (Traballesi, et al., 2012)
demonstrated that following a 12 week rehabilitation program VASS users had better clinical
mobility compared to subjects using a conventional prosthesis with a standard suction socket. The
authors reported that VASS users used their prosthesis more than the control group and that
despite increased use, pain while using the VASS device did not differ significantly compared to
the control group at various points of follow-up. The sample size of the trial involved only 20
subjects, three of whom dropped out of the study, and therefore generalization of results to larger
populations cannot be made.
The published evidence does not provide strong support of clinical utility for this technology
compared to conventional socket-suspension systems for the general population and clinical
effectiveness has not been firmly established in this subgroup. The choice of a suspension system
is determined by factors such as activity level, residual stump shape, age, and health status.
There is some evidence to support vacuum systems decrease limb volume fluctuations, can
improve socket fit, reduce inside movement for some individuals, as well as improve comfort and
satisfaction (Gholizadeh, et al., 2016). While additional long term studies and higher quality data
would be helpful for evaluating an active suction-type vacuum suspension system, for individuals
where other types of suspension systems have failed to provide a secure fit or are contraindicated,
a vacuum suction-type suspension system may be considered an effective alternative.

Page 16 of 34
Medical Coverage Policy: 0536
LOWER LIMB: Microprocessor-controlled Device
Microprocessor-controlled Knee: Microprocessor-controlled knee prosthetics are sensor-
equipped devices. The sensor detects when the knee is in full extension and adjusts the swing
phases automatically, allowing a more natural pattern of walking at variable speeds (passive
powered device). Multiple devices are available that use various degrees of computer technology
to enhance the clinical function of the basic mechanical knee design; all microprocessor controlled
systems do not have identical features and functions. Some devices have swing phase only,
stance phase only, or swing and stance phase. Some of the devices currently available include
but are not limited to the Otto Bock C-Leg
®
, Genium and X2 (Otto Bock HealthCare, Minneapolis,
MN), and the Endolite Orion, Intelligent and SmartIP (Endolite North America, Chase A.
Blatchford and Sons Ltd., Miamisburg, OH). Another microprocessor device, the X3 (Otto Bock
HealthCare, Minneapolis, MN), is waterproof; the device is completely submersible according to
the manufacturer. The Kenevo prosthetic knee (Ottobock) is a device that is recommended for
users with low to moderate mobility (indoor ambulation, limited outdoor ambulation) and is
purported to better support those who use a walker, cane, crutch or wheelchair device. According
to the manufacturer this device is not indicated for walking speeds greater than 3 km/hour and
has a supported feature for stand-to-sit and sit-to-stand, wheelchair mode, and for putting on the
prosthesis while seated. A number of other devices are currently under investigation.
The purported advantages of a microprocessor controlled above-the-knee (AKA) prosthesis
include:
• reduced energy expenditure of the amputee
• improved ability to walk on uneven ground
• improved ability to climb and descend stairs
• increased walking distance
Literature Review: In the published, peer-reviewed scientific literature, evidence supporting the
use of microprocessor-controlled/computer-controlled prostheses comes primarily from small-
group case studies with few randomized, case-controlled trials, and systematic reviews. Of the
groups studied clinically, most individuals were in good health and without other medical
complications. Evidence in the peer-reviewed, published scientific literature does support reduction
in energy consumption improved physical function, and a more symmetrical gait pattern when
compared to a conventional device (Carse, et al., 2021; Aldridge Whitehead, et al., 2014) with
some studies showing a decreased fall risk (McGrath, et al., 2022; Campbell, et al., 2020). Some
evidence supports both reduced hip moment and metabolic requirements particularly at faster
speeds. Although the evidence continues to evolve, there is evidence that supports the effective
use of these devices for limited populations. Evidence evaluating microprocessor prosthetic knee
devices for users that are less active in the community, and/or limited to indoor use (i.e., <
functional level 3) is insufficient to support clinical utility and improved health outcomes.
Microprocessor-controlled Ankle: In order to enhance the basic mechanical design and mimic
the action of a biological ankle researchers have applied microprocessor technology to prosthetic
feet (e.g., Proprio Foot, Ossur, élan Foot, Endolite). Stair ambulation is limited in the transtibial
amputee as a result of neutral and fixed ankle position. Newer prosthetic ankles which adjust for
ankle angle during swing phase and identify sloping gradients and ascent or descent of stairs are
under investigation. One microprocessor-controlled ankle foot prosthesis currently available which
has received FDA approval is the Proprio Foot
®
(Ossur, ALiso Viejo, CA). The Proprio Foot is a
quasi-passive ankle that is able to actively change the ankle angle in the unloaded swing phase as
the result of microprocessor-control and sensor technology. The device is passive (without power)
while in stance phase. According to the manufacturer the proposed benefits of microprocessor–
controlled ankle movements include the ability to identify slopes and stairs, when ascending or
descending stairs the device automatically adapts ankle position to enable the next step; allows

Page 17 of 34
Medical Coverage Policy: 0536
the user to place both feet behind their knees when rising from a chair; and automatically gives a
toe-lift allowing sufficient ground clearance when walking. The device is designed to promote a
more symmetrical and balanced gait and is intended for use by transtibial amputees engaging in
low to moderate impact activities who are classified as level K3 (i.e., community ambulatory, with
the ability or potential for ambulation with variable cadence); it is not suitable for sport and high
impact activities.
Literature Review: Evidence in the published peer-reviewed scientific literature evaluating the
use of microprocessor-controlled ankle foot devices is limited and consists mainly of pilot studies
and case series involving small sample populations (Ernst, et al., 2022; Kim, et al., 2021;
Struchkov, Buckley, 2016; Although limited, the evidence does demonstrate some clinical
advantages for use compared to conventional ankle foot prosthesis for individuals who are
functional level 3 or greater. These devices may improve slope and uneven terrain ambulation
allowing larger range of motion of the ankle when compared with other conventional devices.
Combination Microprocessor-controlled Knee-Ankle/Foot Prosthetic: Combination
microprocessor prosthetics are available integrating both a microprocessor knee and the
ankle/foot device (e.g., SYMBIONIC
®
LEG 3 [Ossur, Iceland]; LiNX
®
[Endolite]). One device, the
SYMBIONIC
®
LEG 3 is a prosthetic that combines a microprocessor knee with a powered
microprocessor ankle with proactive ankle flexion. The device purportedly has a more powerful
knee actuator and new kinematic sensors for improved stability, increased support with stance
flexion, and more rapid, and consistent swing extension. For a transfemoral amputee, combining
both types of prosthetic devices theoretically enables a more natural and symmetrical gait when
ambulating, decreasing energy expenditure, and offering increased stability. The device is
intended for use by individuals who are Functional Level 3 or 4. The LiNX
®
[Endolite]) prosthetic
system is intended for individuals who are Functional Level 3 or greater; according to the
manufacturer this system is an integrated prosthetic utilizing a microprocessor-controlled system
in addition to sensors and actuators which simultaneously controls the knee and foot.
LOWER LIMB: Powered Microprocessor-controlled Prosthetic Device
Powered Knee: Powered prosthetic devices that use signals from muscle activity in the
remaining limb to bend and straighten the device remain under investigation. These devices utilize
sensors and electronics to process data and control movement and power of the knee. Examples
of this type of device include the Power Knee™, manufactured by Ossur (Foothill Ranch, CA).
According to the manufacturer, the Power Knee is described as a motorized device which contains
a rechargeable battery pack. It is designed to replace muscle activity of the quadriceps muscle
and uses artificial proprioception with sensors in order to anticipate and respond with the
appropriate movement required for stepping (active powered device). In comparison to a passive
prosthetic knee, including a microprocessor device, the manufacturer suggests a power knee
offers advantages such as powered extension with standing, controlled resistance with
descending, and active flexion and extension during walking. The device controls the transition
from a bent knee to an extended knee, at heel strike supports the individual’s full body weight,
and can help lift above-knee amputees out of a chair to a standing position. It is suggested the
device helps to maintain walking speeds, assists with upward motion (required for stairs and
inclines), and learns and responds to gait patterns. With the initial use of the device a practitioner
must program and align the knee. Once programming and alignment are complete, the user needs
only to press the power button to use the device. The device is compatible with a variety of
dynamic flex-foot feet, must be re-charged daily and is not intended for high impact activity,
sports, excessive loading or heavy duty use.
According to criteria outlined in the Centers for Medicare and Medicaid Services Local Coverage
Determination, the following individuals may benefit from the use of a power knee-ankle device:

Page 18 of 34
Medical Coverage Policy: 0536
• the individual has a microprocessor (swing and stance phase type (L5856) controlled
(electronic) knee
• is K3 functional level only
• has a documented comorbidity of the spine and/or sound limb affecting hip extension
and/or quadriceps function that impairs K-3 level function with the use of a
microprocessor-controlled knee alone
• is able to make use of a product that requires daily charging
• is able to understand and respond to error alerts and alarms indicating problems with the
function of the unit.
Powered Foot-ankle: Similar to the powered knee device, powered foot-ankle prosthetic
devices (HCPCS L5973 and L5969) are currently being developed. Two such devices are the
BiOM
®
Ankle and emPOWER
™
Ankle, (BionX Medical Technologies, [previously iWalk, Inc., Bedford,
MA). The BiOM device (previously referred to as Powerfoot One) uses a combination of
processors, sensors, motors, and springs that allow the user a powered push-off with taking steps.
Theoretically the device replaces the action of the foot, Achilles tendon and calf muscle to result in
a near normalized gait for amputees and is intended for amputees that are functional level 3 or 4.
According to the manufacturer, the emPOWER
™
Ankle is a more recent generation of the BiOM
®
Ankle.
Literature Review: The available evidence in the published scientific literature consists mainly of
studies evaluating device design and biomechanics with few comparative clinical trials available.
While some authors have reported on performance such as kinematic measures, improved energy
costs, and biomechanical analysis (Simon, et al.,, 2016; Ingraham, et al., 2016; Gates, et al,
2013; Aldridge, et al., 2012) with the use of a powered prosthetic device (ankle/foot or knee),
these studies involve small sample populations and evaluate short-term outcomes. Wolfe et al.
(2013) evaluated functional and clinical differences during sit-to-stand and step-up among power
knee device users (n=5) compared to the microprocessor C-Leg (n=5). The authors noted few
differences between users during sit-to-stand and step-up task and no difference with regards to
decreased impact on the intact limb. Currently there remains a paucity of published clinical trials
evaluating ankle/foot powered devices (Rabago, et al., 2016; Esposito, et al., 2016;Takahashi, et
al., 2013; Grabowski, DeAndrea, 2013; Herr, Grabowski, 2012). Until clinical trials are conducted
to confirm the safety, efficacy and overall clinical utility of the powered ankle/foot device
compared with other conventional or microprocessor prostheses, improvement in net health
outcomes has yet to be determined.
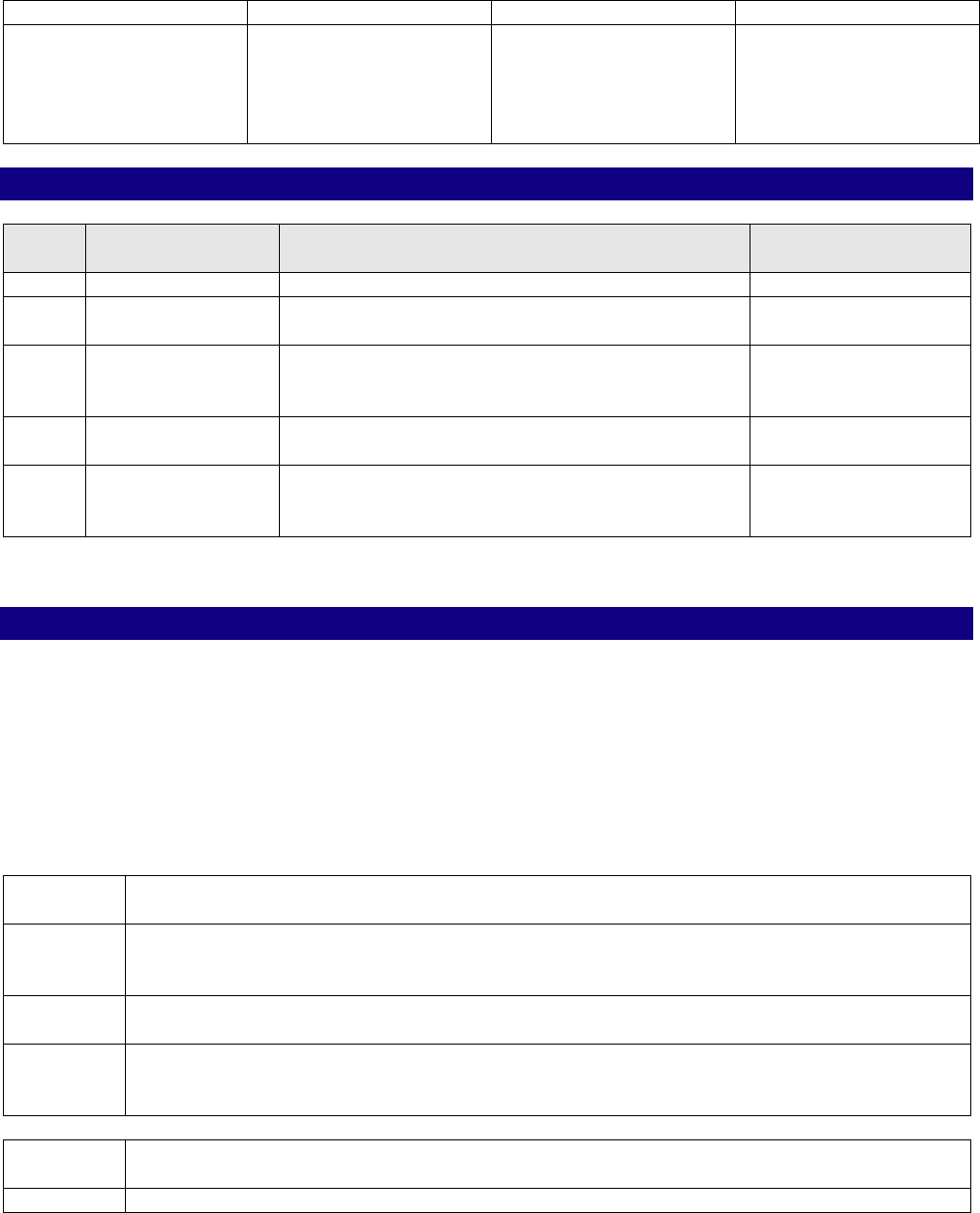
Appendix
Appendix 1 – Lower Limb Prosthetic “Device to Coding” Crosswalk
Please note, coding may vary according to manufacturer. This list is for informational
purposes only, it DOES NOT indicate coverage/non-coverage of a device.
Device Name
Brief Description
Manufacturer
Code(s)
Allux
Microprocessor-
controlled knee
Nabtesco
L5613, L5845, L5848,
L5856, K1014
BiOM Foot
Microprocessor-
controlled ankle foot
(power)
BionX Medical
Technologies
L5969, L5973
C-Leg
Microprocessor-
controlled knee
Otto Bock
L5856, L5848, L5845,
L5828

Page 19 of 34
Medical Coverage Policy: 0536
Device Name
Brief Description
Manufacturer
Code(s)
C-Leg Compact
Microprocessor-
controlled knee
Otto Bock
L5858, L5828, L5848
Élan Foot
Microprocessor-
controlled ankle foot
Blatchford
L5973
EmPOWER™
Microprocessor-
controlled ankle foot
(power)
BionX Medical
Technologies
L5969, L5973
Genium
Microprocessor-
controlled knee
Otto Bock
L5999, L5999,
L5999,L5848, L5828,
L5850, and L5930
Genium X2, Genium
X3
Microprocessor-
controlled knee (X3 is
water proof)
Otto Bock
L5999
Kenevo
Microprocessor
controlled knee joint
Otto Bock
L5828,L5845, L5848,
L5856
Kinnex Foot
Microprocessor
ankle/foot
(waterproof)
Freedom Innovations
L5973
LiNX
®
Combination
microprocessor-
controlled knee and
foot; additionally has
sensors and actuators
Blatchford
L5856, L5848, L5845,
L5828, L5973
Meridium Foot
Microprocessor-
controlled ankle foot
Otto Bock
L5999
Orion 3
Microprocessor-
controlled knee
Blatchford
L5856, L5848, L5845,
L5828
Össur Power Knee
Motor powered knee
Össur
L5859, L5856, L5828,
L5848, L5845
Plié 3
Microprocessor-
controlled knee
(submersible)
Freedom Innovation
(Freedom innovation
component recently
purchased by Otto
Bock)
L5856, L5848, L5845,
L5828
Proprio Foot
®
Microprocessor-
controlled ankle foot
Össur
L5973
Raize Foot
Microprocessor foot
(does not have the
power ankle)
Fillauer
L5973
Rheo
Microprocessor-
controlled knee
Össur
L5856, L5848, L5845,
L5828
Rheo XC
Microprocessor-
controlled knee
(supports
rehabilitation to full
recovery)
Össur
L5856, L5848, L5845,
L5828
Smart IP
Microprocessor-
controlled knee, with
weight activated
stance control
Blatchford
L5857, L5830, (L5845
for Stancflex models
only)
Page 20 of 34
Medical Coverage Policy: 0536
Device Name
Brief Description
Manufacturer
Code(s)
SYMBIONIC
®
LEG 3
Combination
microprocessor-
controlled knee and
ankle with proactive
ankle flexion
Össur
L5856, L5848, L5845,
L5828, L5973
Medicare Coverage Determinations
Contractor
Determination Name/Number
Revision Effective
Date
NCD
National
No NCD
LCD
CGS
Administrators
Lower Limb Prosthesis (LCD L33787)
1/1/2020
LCD
Noridian
Healthcare
Solutions
Lower Limb Prosthesis (LCD L33787)
1/1/2020
LCD
CGS
Administrators
Facial Prosthesis LCD L33738)
1/1/2020
LCD
Noridian
Healthcare
Solutions
Facial Prosthesis (LCD L33738)
1/1/2020
Note: Please review the current Medicare Policy for the most up-to-date information.
(NCD = National Coverage Determination; LCD = Local Coverage Determination)
Coding Information
Notes:
1. This list of codes may not be all-inclusive since the AMA and CMS code updates may occur
more frequently than policy updates.
2. Deleted codes and codes which are not effective at the time the service is rendered may
not be eligible for reimbursement.
IRIS PROSTHESIS
Experimental/ Investigational/ Unproven:
CPT
®
*
Codes
Description
0616T
Insertion of iris prosthesis, including suture fixation and repair or removal of iris,
when performed; without removal of crystalline lens or intraocular lens, without
insertion of intraocular lens
0617T
Insertion of iris prosthesis, including suture fixation and repair or removal of iris,
when performed; with removal of crystalline lens and insertion of intraocular lens
0618T
Insertion of iris prosthesis, including suture fixation and repair or removal of iris,
when performed; with secondary intraocular lens placement or intraocular lens
exchange
HCPCS
Codes
Description
C1839
Iris prosthesis

Page 21 of 34
Medical Coverage Policy: 0536
EXTERNAL FACIAL PROSTHESIS
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met and only when coverage is available under the plan for the specific
device/component/item.
Nasal Prosthesis
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
CPT
®
*
Codes
Description
21087
Impression and custom preparation; nasal prosthesis
HCPCS
Codes
Description
L8040
Nasal prosthesis, provided by a non-physician
L8047
Nasal septal prosthesis, provided by a non-physician
Orbit Prosthesis
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
CPT
®
*
Codes
Description
21077
Impression and custom preparation; orbital prosthesis
HCPCS
Codes
Description
L8042
Orbital prosthesis, provided by a non-physician
Ear Prosthesis
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
CPT
®
*
Codes
Description
21086
Impression and custom preparation; auricular prosthesis
HCPCS
Codes
Description
L8045
Auricular prosthesis, provided by a non-physician
Facial Prosthesis
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
CPT
®
*
Codes
Description
21088
Impression and custom preparation; facial prosthesis

Page 22 of 34
Medical Coverage Policy: 0536
HCPCS
Codes
Description
L8041
Midfacial prosthesis, provided by a non-physician
L8043
Upper facial prosthesis, provided by a non-physician
L8044
Hemi-facial prosthesis, provided by a non-physician
L8046
Partial facial prosthesis, provided by a non-physician
Maxillofacial Prosthesis, External
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
HCPCS
Codes
Description
L8048
Unspecified maxillofacial prosthesis, by report, provided by a non-physician
Considered not medically necessary when used to report non-covered consumable
supplies outlined in the coverage policy:
HCPCS
Codes
Description
A4364
Adhesive, liquid or equal, any type, per ounce
A4450
Tape, non-waterproof, per 18 square inches
A4452
Tape, waterproof, per 18 square inches
A4455
Adhesive remover or solvent (for tape, cement or other adhesive), per ounce
A4456
Adhesive remover, wipes, any type, each
L9900
Orthotic and prosthetic supply, accessory, and/or service component of another
HCPCS “L” code
______________________________________________________________________
UPPER LIMB ADDITIONS/COMPONENTS
Additional Components/Features of Non Myoelectric Prosthetic Device
Considered Medically Necessary when used to report a medically necessary component
or addition to an upper limb prosthetic device in the absence of a specific code:
HCPCS
Codes
Description
L6646
Upper extremity addition, shoulder joint, multipositional locking, flexion, adjustable
abduction friction control, for use with body powered or external powered system
L6647
Upper extremity addition, shoulder lock mechanism, body powered actuator
L7499
†
Upper extremity prosthesis, not otherwise specified
†
Note: Covered when used to report a medically necessary component or addition to an
upper limb prosthetic device in the absence of a specific code.
UPPER LIMB: MYOELECTRIC PROSTHETIC DEVICE

Page 23 of 34
Medical Coverage Policy: 0536
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met and only when coverage is available under the plan for the specific
device/component/item:
HCPCS
Codes
Description
L6026
Transcarpal/metacarpal or partial hand disarticulation prosthesis, external power,
self-suspended, inner socket with removable forearm section, electrodes and
cables, two batteries, charger, myoelectric control of terminal device, excludes
terminal device(s)
L6611
Addition to upper extremity prosthesis, external powered, additional switch, any
type
L6638
Upper extremity addition to prosthesis, electric locking feature, only for use with
manually powered elbow
L6646
Upper extremity addition, shoulder joint, multipositional locking, flexion, adjustable
abduction friction control, for use with body powered or external powered system
L6648
Upper extremity addition, shoulder lock mechanism, external powered actuator
L6715
Terminal device, multiple articulating digit, includes motor(s), initial issue or
replacement
L6880
Electric hand, switch, or myoelectric controlled, independently articulating digits,
any grasp pattern or combination of grasp patterns, includes motor(s)
L6881
Automatic grasp feature, addition to upper limb electric prosthetic terminal device
L6882
Microprocessor control feature, addition to upper limb prosthetic terminal device
L6920
Wrist disarticulation, external power, self-suspended inner socket, removable
forearm shell, Otto Bock or equal, switch, cables, two batteries and one charger,
switch control of terminal device
L6925
Wrist disarticulation, external power, self-suspended inner socket, removable
forearm shell, Otto Bock or equal, electrodes, cables, two batteries and one
charger, myoelectronic control of terminal device
L6930
Below elbow, external power, self-suspended inner socket, removable forearm
shell, Otto Bock or equal switch, cables, two batteries and one charger, switch
control of terminal device
L6935
Below elbow, external power, self-suspended inner socket, removable forearm
shell, Otto Bock or equal electrodes, cables, two batteries and one charger,
myoelectronic control of terminal device
L6940
Elbow disarticulation, external power, molded inner socket, removable humeral
shell, outside locking hinges, forearm, Otto Bock or equal switch, cables, two
batteries and one charger, switch control of terminal device
L6945
Elbow disarticulation, external power, molded inner socket, removable humeral
shell, outside locking hinges, forearm, Otto Bock or equal electrodes, cables, two
batteries and one charger, myoelectronic control of terminal device
L6950
Above elbow, external power, molded inner socket, removable humeral shell,
internal locking elbow, forearm, Otto Bock or equal switch, cables, two batteries
and one charger, switch control of terminal device
L6955
Above elbow, external power, molded inner socket, removable humeral shell,
internal locking elbow, forearm, Otto Bock or equal electrodes, cables, two batteries
and one charger, myoelectronic control of terminal device
L6960
Shoulder disarticulation, external power, molded inner socket, removable shoulder
shell, shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or
equal switch, cables, two batteries and one charger, switch control of terminal
device

Page 24 of 34
Medical Coverage Policy: 0536
HCPCS
Codes
Description
L6965
Shoulder disarticulation, external power, molded inner socket, removable shoulder
shell, shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or
equal electrodes, cables, two batteries and one charger, myoelectronic control of
terminal device
L6970
Interscapular-thoracic, external power, molded inner socket, removable shoulder
shell, shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or
equal switch, cables, two batteries and one charger, switch control of terminal
device
L6975
Interscapular-thoracic, external power, molded inner socket, removable shoulder
shell, shoulder bulkhead, humeral section, mechanical elbow, forearm, Otto Bock or
equal electrodes, cables, two batteries and one charger, myoelectronic control of
terminal device
L7007
Electric hand, switch or myoelectric controlled, adult
L7008
Electric hand, switch or myoelectric controlled, pediatric
L7009
Electric hook, switch or myoelectric controlled, adult
L7040
Prehensile actuator, switch controlled
L7045
Electric hook, switch or myoelectric controlled, pediatric
L7170
Electronic elbow, Hosmer or equal, switch controlled
L7180
Electronic elbow, microprocessor sequential control of elbow and terminal device
L7181
Electronic elbow, microprocessor simultaneous control of elbow and terminal device
L7185
Electronic elbow, adolescent, Variety Village or equal, switch controlled
L7186
Electronic elbow, child, Variety Village or equal, switch controlled
L7190
Electronic elbow, adolescent, Variety Village or equal, myoelectronically controlled
L7191
Electronic elbow, child, Variety Village or equal, myoelectronically controlled
L7259
Electronic wrist rotator, any type
L7499
†
Upper extremity prosthesis, not otherwise specified
†
Note: Considered Medically Necessary when used to report components and/or
additions to an upper limb prosthetic myoelectric device, if coverage for a myoelectric
prosthetic device is available, and when medical necessity criteria are met.
Experimental/ Investigational/ Unproven when used to report an upper limb sensor and
myoelectric controlled prosthetic device with simultaneous multiple degrees of freedom
(e.g., LUKE [Life Under Kinetic Evolution] Arm) or for an upper limb prosthetic device
using electromyography-based brain computer interface (BCI):
HCPCS
Codes
Description
L7499
Upper extremity prosthesis, not otherwise specified
______________________________________________________________________________
LOWER LIMB: MECHANICAL (NON-POWERED, NON MICROPROCESSOR)
Considered Medically Necessary when used to report a component or addition to a lower
limb prosthetic device when criteria in the applicable policy statements listed above are
met and when coverage is available under the plan for the specific
device/component/item:
HCPCS
Codes
Description

Page 25 of 34
Medical Coverage Policy: 0536
L5828
†
Addition, endoskeletal knee-shin system, single axis, fluid swing and stance phase
control
L5845
††
Addition, endoskeletal knee-shin system, stance flexion feature, adjustable
L5848
†
Addition to endoskeletal, knee-shin system, fluid stance extension, dampening
feature, with or without adjustability
L5930
†††
Addition, endoskeletal system, high activity knee control frame
L5981
†
All lower extremity prostheses, flex-walk system or equal
L5999
††††
Lower extremity prosthesis, not otherwise specified
†
Note: Considered medically necessary for functional level 3 or above when medical
necessity criteria has been met for the base device.
††
Note: Considered medically necessary for functional level 1 or above when medical
necessity criteria has been met for the base device.
†††
Note: Requires K-4 functional level and when medical necessity criteria has been met
for the base device.
††††
Note: Considered medically necessary when used to report a medically necessary
component or addition to a lower limb prosthetic device in the absence of a more
specific code and when medical necessity criteria has been met for the base device.
LOWER LIMB MICROPROCESSOR-CONTROLLED PROSTHETIC DEVICES
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met and when benefits are available under the plan for a microprocessor-
controlled prosthetic:
HCPCS
Codes
Description
L5856
Addition to lower extremity prosthesis, endoskeletal knee-shin system,
microprocessor control feature, swing and stance phase, includes electronic
sensor(s), any type
L5857
Addition to lower extremity prosthesis, endoskeletal knee-shin system,
microprocessor control feature, swing phase only, includes electronic sensor(s),
any type
L5858
Addition to lower extremity prosthesis, endoskeletal knee shin system,
microprocessor control feature, stance phase only, includes electronic sensor(s),
any type
L5973
Endoskeletal ankle foot system, microprocessor controlled feature, dorsiflexion
and/or plantar flexion control, includes power source
Additional Components/Features of Microprocessor-Controlled Prosthetic Devices:
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met and when benefits are available under the plan for a microprocessor-
controlled prosthetic:
HCPCS
Codes
Description
K1014
Addition, endoskeletal knee-shin system, 4 bar linkage or multiaxial, fluid swing
and stance phase control
L5828
Addition, endoskeletal knee-shin system, single axis, fluid swing and stance phase
control

Page 26 of 34
Medical Coverage Policy: 0536
L5845
Addition, endoskeletal knee-shin system, stance flexion feature, adjustable
L5848
Addition to endoskeletal, knee-shin system, fluid stance extension, dampening
feature, with or without adjustability
L5920
Addition, endoskeletal system, above knee or hip disarticulation, alignable system
L5925
Addition, endoskeletal system, above knee, knee disarticulation or hip
disarticulation, manual lock
L5930
†
Addition, endoskeletal system, high activity knee control frame
L5950
Addition, endoskeletal system, above knee, ultra-light material (titanium, carbon
fiber or equal)
L5999
††
Lower extremity prosthesis, not otherwise specified
†
Note: L5930 requires K-4 functional level.
††
Note: Covered when used to report a medically necessary component/feature or
addition to a lower limb prosthetic microprocessor-controlled device in the absence of a
specific code.
LOWER LIMB: POWERED MICROPROCESSOR-CONTROLLED PROSTHETIC DEVICES
Considered Medically Necessary and when benefits are available for a power-controlled
or power- assisted lower limb knee device (e.g., Ossur Power Knee):
HCPCS
Codes
Description
L5859
†
Addition to lower extremity prosthesis, endoskeletal knee-shin system, powered
and programmable flexion/extension assist control, includes any type motor(s)
†
Note: L5859 requires K-3 functional level; the device is not intended for high impact
activity, sports, excessive loading or heavy duty use.
Microprocessor-Controlled Ankle Foot Prosthetic with Power Assist (e.g., BiOM
®
Ankle,
emPOWER
™
Ankle)
Considered Not Medically Necessary:
HCPCS
Codes
Description
L5969
Addition, endoskeletal ankle-foot or ankle system, power assist, includes any type
motor(s)
L5973
Endoskeletal ankle foot system, microprocessor controlled feature, dorsiflexion
and/or plantar flexion control, includes power source
LOWER LIMB OSSEOINTEGRATED DEVICE
Experimental/Investigational/Unproven:
HCPCS
Codes
Description
L5991
Addition to lower extremity prostheses, osseointegrated external prosthetic
connector
Additional Components/Features of Powered Prosthetic Devices, Including Power Assist
Features:

Page 27 of 34
Medical Coverage Policy: 0536
Experimental/Investigational/Unproven when reported in addition to a non-covered
power-controlled (L5859, L5973) or power-assisted (L5969) prosthetic device:
HCPCS
Codes
Description
L5828
Addition, endoskeletal knee-shin system, single axis, fluid swing and stance phase
control
L5845
Addition, endoskeletal knee-shin system, stance flexion feature, adjustable
L5848
Addition to endoskeletal knee-shin system, fluid stance extension, dampening
feature, with or without adjustability
L5856
Addition to lower extremity prosthesis, endoskeletal knee-shin system,
microprocessor control feature, swing and stance phase, includes electronic
sensor(s), any type
L5969
Addition, endoskeletal ankle-foot or ankle system, power assist, includes any type
motor(s)
______________________________________________________________________________
LOWER LIMB: VACUUM SUSPENSION SYSTEM
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
HCPCS
Codes
Description
L5781
Addition to lower limb prosthesis, vacuum pump, residual limb volume management
and moisture evacuation system
L5782
Addition to lower limb prosthesis, vacuum pump, residual limb volume management
and moisture evacuation system, heavy duty
______________________________________________________________________________
REPAIR AND REPLACEMENT
Considered Medically Necessary when criteria in the applicable policy statements listed
above are met:
HCPCS
Codes
Description
L7510
Repair of prosthetic device, repair or replace minor parts
L7520
Repair prosthetic device, labor component, per 15 minutes
L8049
Repair or modification of maxillofacial prosthesis, labor component, 15 minute
increments, provided by a non-physician
*Current Procedural Terminology (CPT
®
) ©2023 American Medical Association: Chicago,
IL.
References
1. Aldridge JM, Sturdy JT, Wilken JM. Stair ascent kinematics and kinetics with a powered
lower leg system following transtibial amputation. Gait Posture. 2012 Jun;36(2):291-5.

Page 28 of 34
Medical Coverage Policy: 0536
2. Aldridge Whitehead JM1, Wolf EJ, Scoville CR, Wilken JM. Does a Microprocessor-controlled
Prosthetic Knee Affect Stair Ascent Strategies in Persons With Transfemoral Amputation?
Clin Orthop Relat Res. 2014 Feb 11.
3. Alzeer AM, Bhaskar Raj N, Shahine EM, Nadiah WA. Impacts of Microprocessor-Controlled
Versus Non-microprocessor-Controlled Prosthetic Knee Joints Among Transfemoral
Amputees on Functional Outcomes: A Comparative Study. Cureus. 2022 Apr
21;14(4):e24331.
4. Ang M, Tan D. Anterior segment reconstruction with artificial iris and Descemet membrane
endothelial keratoplasty: a staged surgical approach. Br J Ophthalmol. 2021 Feb
26:bjophthalmol-2020-317906.
5. Ayres BD, Fant BS, Landis ZC, Miller KM, Stulting RD, Cionni RJ, Fram NR, Hamilton S,
Hardten DR, Koch DD, Masket S, Price FW Jr, Rosenthal KJ, Hamill MB, Snyder ME. Results
of the United States Food and Drug Administration Clinical Trial of the CustomFlex Artificial
Iris. Ophthalmology. 2022 Jun;129(6):614-625.
6. Barnett CT, Hughes LD, Sullivan AE, Strutzenberger G, Levick JL, Bisele M, De Asha AR.
Exploring the interaction of knee and ankle component use on mobility test performance in
people with unilateral transfemoral amputation. Prosthet Orthot Int. 2021 Dec 1;45(6):470-
476.
7. Beil TL, Street GM, Covey SJ. Interface pressures during ambulation using suction and
vacuum-assisted prosthetic sockets. J Rehabil Res Dev. 2002 Nov-Dec;39(6):693-700
8. Bellmann M, Schmalz T, Blumentritt S. Comparative biomechanical analysis of current
microprocessor-controlled prosthetic knee joints. Arch Phys Med Rehabil. 2010
Apr;91(4):644-52.
9. Bergman K, Ornholmer L, Zackrisson K, Thyberg M. Functional benefit of an adaptive
myoelectric prosthetic hand compared to a conventional myoelectric hand. Prosthet Orthot
Int. 1992 Apr;16(1):32-7.
10. Blatchford. Prosthetic Products. Knees. Accessed November 30, 2023. Available at URL
address: https://www.blatchfordmobility.com/en-us/products/feet-ankles
11. Bonnet C, Miller KM. Safety and efficacy of custom foldable silicone artificial iris
implantation: prospective compassionate-use case series. J Cataract Refract Surg. 2020
Jun;46(6):893-901.
12. Bouwsema H, van der Sluis CK, Bongers RM. Learning to control opening and closing a
myoelectric hand. Arch Phys Med Rehabil. 2010 Sep;91(9):1442-6.
13. Brunelli S, Delussu AS, Paradisi F, Pellegrini R, Traballesi M. A comparison between the
suction suspension system and the hypobaric Iceross Seal-In® X5 in transtibial amputees.
Prosthet Orthot Int. 2013 Dec;37(6):436-44.
14. Canadian Agency for Drugs and Technologies in Health (CADTH). Osseointegrated Prosthetic
Implants for Lower Limb Amputation: A Review of Clinical Effectiveness, Cost Effectiveness
and Guidelines. Feb 27, 2017. Accessed November 30, 2023. Available at URL address:
https://www.cadth.ca/sites/default/files/pdf/htis/2017/RC0856%20Osseointegrated%20Pro
sthetic%20Implants%20Final.pdf
Page 29 of 34
Medical Coverage Policy: 0536
15. Carey SL, Lura DJ, Highsmith MJ; CP; FAAOP. Differences in myoelectric and body-powered
upper-limb prostheses: Systematic literature review. J Rehabil Res Dev. 2015;52(3):247-
62.
16. Carse B, Scott H, Brady L, Colvin J. Evaluation of gait outcomes for individuals with
established unilateral transfemoral amputation following the provision of microprocessor
controlled knees in the context of a clinical service. Prosthet Orthot Int. 2021 Jun
1;45(3):254-261.
17. Crawford AZ, Freundlich SEN, Lim J, McGhee CNJ. Endocapsular artificial iris implantation
for iris defects: Reducing symptoms, restoring visual function and improving cosmesis. Clin
Exp Ophthalmol. 2022 Jul;50(5):490-499.
18. Darter BJ, Sinitski K, Wilken JM. Axial bone-socket displacement for persons with a
traumatic transtibial amputation: The effect of elevated vacuum suspension at progressive
body-weight loads. Prosthet Orthot Int. 2015 Sep 30.
19. Darter BJ, Wilken JM. Energetic consequences of using a prosthesis with adaptive ankle
motion during slope walking in persons with a transtibial amputation. Prosthet Orthot Int.
2013 Mar 22.
20. Datta D, Ibbotson V. Powered prosthetic hands in very young children. Prosthet Orthot
Int.1998 Aug;22(2):150-4.
21. Davie-Smith F, Carse B. Comparison of patient-reported and functional outcomes following
transition from mechanical to microprocessor knee in the low-activity user with a unilateral
transfemoral amputation. Prosthet Orthot Int. 2021 Jun 1;45(3):198-204.
22. Delussu AS, Brunelli S, Paradisi F, Iosa M, Pellegrini R, Zenardi D, Traballesi M. Assessment
of the effects of carbon fiber and bionic foot during overground and treadmill walking in
transtibial amputees. Gait Posture. 2013 Sep;38(4):876-82.
23. Edwards SG, Gellman H. Elbow and Above-elbow Amputations. Medscape. December 23,
2015. Updated Oct 2, 2019, Dec 01, 2022. Accessed November 30, 2023. Available at URL
address: http://emedicine.medscape.com/article/1237886-overview
24. Ernst M, Altenburg B, Schmalz T, Kannenberg A, Bellmann M. Benefits of a microprocessor-
controlled prosthetic foot for ascending and descending slopes. J Neuroeng Rehabil. 2022
Jan 28;19(1):9.
25. Figueiredo GB, Snyder ME. Long-term follow-up of a custom-made prosthetic iris device in
patients with congenital aniridia. J Cataract Refract Surg. 2020 Jun;46(6):879-887.
26. Frisina R, De Biasi CS, Londei D, et al. A new intraocular lens with artificial iris for treating a
case of iris extrusion secondary to traumatic opening of a radial keratotomy. Eur J
Ophthalmol. 2020 Jan 23.
27. Fuenzalida Squella SA, Kannenberg A, Brandão Benetti Â. Enhancement of a prosthetic knee
with a microprocessor-controlled gait phase switch reduces falls and improves balance
confidence and gait speed in community ambulators with unilateral transfemoral
amputation. Prosthet Orthot Int. 2017 Jul 1:309364617716207.
Page 30 of 34
Medical Coverage Policy: 0536
28. Gailey RS, Gaunaurd I, Agrawal V, Finnieston A, O'Toole C, Tolchin R. Application of self-
report and performance-based outcome measures to determine functional differences
between four categories of prosthetic feet. J Rehabil Res Dev. 2012;49(4):597-612.
29. Gates DH, Aldridge JM, Wilken JM. Kinematic comparison of walking on uneven ground
using powered and unpowered prostheses. Clin Biomech (Bristol, Avon). 2013
Apr;28(4):467-72.
30. Ghaffari R, Aldave AJ, Al-Hashimi S, Miller KM. Complications of Cosmetic Artificial Iris
Implantation and Post Explantation Outcomes. Am J Ophthalmol. 2021 Jun;226:156-164.
31. Gholizadeh H, Lemaire ED, Eshraghi A. The evidence-base for elevated vacuum in lower
limb prosthetics: Literature review and professional feedback. Clin Biomech (Bristol, Avon).
2016 Jun 22;37:108-116.
32. Grabowski AM, D'Andrea S. Effects of powered ankle-foot prosthesis on kinetic loading of
the unaffected leg during level-ground walking. Neuroeng Rehabil. 2013 Jun 7;10:49.
33. Hafner BJ, Halsne EG, Morgan SJ, Morgenroth DC, Humbert AT. Effects of prosthetic feet on
metabolic energy expenditure in people with transtibial amputation: A systematic review
and meta-analysis. PM R. 2021 Aug 14.
34. Hahn A, Bueschges S, Prager M, Kannenberg A. The effect of microprocessor controlled exo-
prosthetic knees on limited community ambulators: systematic review and meta-analysis.
Disabil Rehabil. 2021 Oct 25:1-19.
35. Herr HM, Grabowski AM. Bionic ankle-foot prosthesis normalizes walking gait for persons
with leg amputation. Proc Biol Sci. 2012 Feb 7;279(1728):457-64.
36. Highsmith MJ, Kahle JT, Miro RM, Mengelkoch LJ. Ramp descent performance with the C-Leg
and interrater reliability of the Hill Assessment Index. Prosthet Orthot Int 2013 Jan 17.
37. Hoskins RD1, Sutton EE, Kinor D, Schaeffer JM, Fatone S. Using vacuum-assisted
suspension to manage residual limb wounds in persons with transtibial amputation: a case
series. Prosthet Orthot Int. 2014 Feb;38(1):68-74.
38. Jakob-Girbig J, Salewsky S, Meller D. Use of the Ophtec Artificial Iris Model C1 in Patients
with Aniridia/Aphakia. Klin Monbl Augenheilkd. 2021 Jul;238(7):803-807.
39. Jayaraman C, Mummidisetty CK, Albert MV, Lipschutz R, Hoppe-Ludwig S, Mathur G,
Jayaraman A. Using a microprocessor knee (C-Leg) with appropriate foot transitioned
individuals with dysvascular transfemoral amputations to higher performance levels: a
longitudinal randomized clinical trial. J Neuroeng Rehabil. 2021 May 25;18(1):88.
40. Ingraham KA, Fey NP, Simon AM, Hargrove LJ. Assessing the Relative Contributions of
Active Ankle and Knee Assistance to the Walking Mechanics of Transfemoral Amputees
Using a Powered Prosthesis. PLoS One. 2016 Jan 25;11(1):e0147661.
41. Kim J, Wensman J, Colabianchi N, Gates DH. The influence of powered prostheses on user
perspectives, metabolics, and activity: a randomized crossover trial. J Neuroeng Rehabil.
2021 Mar 16;18(1):49.
Page 31 of 34
Medical Coverage Policy: 0536
42. Klute GK, Berge JS, Biggs W, Pongnumkul S, Popovic Z, Curless B. Vacuum-assisted socket
suspension compared with pin suspension for lower extremity amputees: effect on fit,
activity, and limb volume. Arch Phys Med Rehabil. 2011 Oct;92(10):1570-5.
43. Komolafe O, Wood S, Caldwell R, Hansen A, Fatone S. Methods for characterization of
mechanical and electrical prosthetic vacuum pumps. J Rehabil Res Dev. 2013;50(8):1069-
78.
44. Kuiken T. Targeted reinnervation for improved prosthetic function. Phys Med Rehabil Clin N
Am. 2006 Feb;17(1):1-13.
45. Kuiken TA, Dumanian GA, Lipschutz RD, Miller LA, Stubblefield KA. The use of targeted
muscle reinnervation for improved myoelectric prosthesis control in a bilateral shoulder
disarticulation amputee. Prosthet Orthot Int. 2004 Dec;28(3):245-53.
46. Kuiken TA, Li G, Lock BA, Lipschutz RD, Miller LA, Stubblefield KA, Englehart KB. Targeted
muscle reinnervation for real-time myoelectric control of multifunction artificial arms. JAMA.
2009 Feb 11;301(6):619-28.
47. Kuiken TA, Marasco PD, Lock BA, Harden RN, Dewald JP. Redirection of cutaneous sensation
from the hand to the chest skin of human amputees with targeted reinnervation. Proc Natl
Acad Sci USA. 2007 Dec:104(50):20061-6.
48. Kunutsor SK, Gillatt D, Blom AW. Systematic review of the safety and efficacy of
osseointegration prosthesis after limb amputation. Br J Surg. 2018 Dec;105(13):1731-
1741.
49. Ledoux ED, Lawson BE, Shultz AH, Bartlett HL, Goldfarb M. Metabolics of stair ascent with a
powered transfemoral prosthesis. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:5307-10.
50. Liberating Technologies. LTI Boston Digital™ Arm Systems for Adults. Accessed December
5, 2022. Available at URL address: http://www.liberatingtech.com/
51. Mayer CS, Baur ID, Storr J, Khoramnia R. Bilateral Artificial Iris implantation in patients with
bilateral iris defects. Am J Ophthalmol Case Rep. 2021 Apr 30;22:101108.
52. Mayer CS, Laubichler AE, Khoramnia R, et al. Challenges and complication management in
novel artificial iris Implantation. J Ophthalmol. 2018 Sep 23; 2018:3262068.
53. Mayer CS, Laubichler AE, Masyk M, et al. Residual iris retraction syndrome after artificial iris
implantation. Am J Ophthalmol. 2019 Mar;199:159-166.
54. Mayer CS, Reznicek L, Hoffmann AE. Pupillary reconstruction and outcome after artificial iris
implantation. Ophthalmology. 2016 May; 123(5):1011-1018.
55. Mileusnic MP, Rettinger L, Highsmith MJ, Hahn A. Benefits of the Genium microprocessor
controlled prosthetic knee on ambulation, mobility, activities of daily living and quality of
life: a systematic literature review. Disabil Rehabil Assist Technol. 2021 Jul;16(5):453-464.
56. Mostafa YS, Osman AA, Hassanein DH, et al. Iris reconstruction using artificial iris prosthesis
for management of aniridia. Eur J Ophthalmol. 2018 Jan;28(1):103-107.
Page 32 of 34
Medical Coverage Policy: 0536
57. Motion Control, Inc. Utah Arm 3+, U3 and U3 base. Accessed November 30, 2023. Available
at URL address: http://www.utaharm.com/ua3-myoelectric-arm.php
58. National Institute for Health and Care Excellence (NICE). Direct skeletal fixation of limb or
digit prostheses using intraosseous transcutaneous implants. IPG 270. Published July 2008.
Accessed November 30, 2023. Available at URL address:
https://www.nice.org.uk/guidance/ipg270/chapter/1-Guidance).
59. National Institute for Health and Care Excellence (NICE). Artificial iris insertion for acquired
aniridia. Interventional procedures guidance (IPG)674. Published July 22, 2020. Accessed
November 30, 2023. Available at URL address: https://www.nice.org
60. Ossur, UA. Power knee. Accessed November 30, 2023Available at URL address:
https://www.ossur.com/en-us/prosthetics/knees/power-knee
61. Otr OV, Reinders-Messelink HA, Bongers RM, Bouwsema H, Van Der Sluis CK. The i-LIMB
hand and the DMC plus hand compared: a case report. Prosthet Orthot Int. 2010
Jun;34(2):216-20.
62. Otto Bock®. C-Leg® System. Accessed November 30, 2023. Available at URL address:
https://shop.ottobock.us/Prosthetics/Lower-Limb-Prosthetics/Knees---Microprocessor/C-
Leg/c/1203
63. Pasquina PF, Evangelista M, Carvalho AJ, et al. First-in-man demonstration of a fully
implanted myoelectric sensors system to control an advanced electromechanical prosthetic
hand. J Neurosci Methods. 2014 Aug 4. pii: S0165-0270(14)00267-2.
64. Pitkin M, Frossard L. Loading effect of prosthetic feet’s anthropomorphicity on transtibial
osseointegrated implant. Military Medicine. 2021;186(Suppl 1):681-687.
65. Prinsen EC, Nederhand MJ, Sveinsdóttir HS, et al. The influence of a user-adaptive
prosthetic knee across varying walking speeds: A randomized cross-over trial. Gait Posture.
2017 Jan;51:254-260.
66. Rábago CA, Aldridge Whitehead J, Wilken JM. Evaluation of a Powered Ankle-Foot Prosthesis
during Slope Ascent Gait. PLoS One. 2016 Dec 15;11(12):e0166815.
67. Rickmann A, Szurman P, Januschowski K, et al. Long-term results after artificial iris
implantation in patients with aniridia. Graefes Arch Clin Exp Ophthalmol. 2016 Jun;
254(7):1419-1424.
68. Romano D, Bremond-Gignac D, Barbany M, Rahman A, Mauring L, Semeraro F, Cursiefen C,
Lagali N, Romano V. Artificial iris implantation in congenital aniridia A systematic review.
Surv Ophthalmol. 2022 Nov 12:S0039-6257(22)00152-7.
69. Russell Esposito E, Aldridge Whitehead JM, Wilken JM. Step-to-step transition work during
level and inclined walking using passive and powered ankle-foot prostheses. Prosthet Orthot
Int. 2016 Jun;40(3):311-9.
70. Samitier CB, Guirao L, Costea M, Camós JM, Pleguezuelos E. The benefits of using a
vacuum-assisted socket system to improve balance and gait in elderly transtibial amputees.
Prosthet Orthot Int. 2014 Sep 26.

Page 33 of 34
Medical Coverage Policy: 0536
71. Simon AM, Fey NP, Ingraham KA, Finucane SB, Halsne EG, Hargrove LJ. Improved Weight-
Bearing Symmetry for Transfemoral Amputees During Standing Up and Sitting Down With a
Powered Knee-Ankle Prosthesis. Arch Phys Med Rehabil. 2016 Jul;97(7):1100-6.
72. Son H-S, Yildirim T, Khoramnia R, et al. Implantation of a small-aperture intraocular lens
and a partial aniridia implant in eyes with traumatic iris defects. Am J Ophthalmol Case Rep.
2020 Mar;18:100673.
73. Struchkov V, Buckley JG. Biomechanics of ramp descent in unilateral trans-tibial amputees:
Comparison of a microprocessor controlled foot with conventional ankle-foot mechanisms.
Clin Biomech (Bristol, Avon). 2016 Feb;32:164-70.
74. Touch Bionics Inc. i-Limb Ultra Hand. Accessed December 5, 2022. Available at URL
address: http://www.touchbionics.com/products/active-prostheses/i-limb-ultra/
75. Traballesi M, Delussu AS, Fusco A, Iosa M, Averna T, Pellegrini R, Brunelli S. Residual limb
wounds or ulcers heal in transtibial amputees using an active suction socket system. A
randomized controlled study. Eur J Phys Rehabil Med. 2012 May 28.
76. U.S. Food and Drug Administration (FDA). Center for Device and Radiological Health (CDRH).
Code of Federal Regulations. Title 21, Volume 8. Part 890-Physical Medicine Devices. Subpart
D-Physical Medicine Prosthetic Devices. Updated April 1, 2016. Accessed November 30,
2023. Available at URL address:
https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=890.3420
77. United States Food and Drug Administration. Center for Devices and Radiological Health.
CustomFlex™ Artificial Iris. Premarket Approval P170039. May 30, 2018. Accessed
November 30, 2023. Available at URL address:
https://www.accessdata.fda.gov/cdrh_docs/pdf17/P170039A.pdf
78. United States Food and Drug Administration. Center for Devices and Radiological Health.
Humanitarian Device Exemption (HDE). The Osseoanchored Prostheses for the
Rehabilitation of Amputees (OPRA). H080004. July 16, 2015.
79. van der Niet O, Bongers RM, van der Sluis CK. Functionality of i-LIMB and i-LIMB pulse
hands: case report. J Rehabil Res Dev. 2013;50(8):1123-8.
80. Weber EL, Stevens PM, England DL, Swilley VD, Wurdeman SR. Microprocessor feet improve
prosthetic mobility and physical function relative to non-microprocessor feet. J Rehabil
Assist Technol Eng. 2022 Jul 11;9:20556683221113320.
81. Weissbart SB, Ayres BD. Management of aniridia and iris defects: An update on iris
prosthesis options. Curr Opin Ophthalmol. 2016 May;27(3):244-249.
82. Wolf EJ, Everding VQ, Linberg AA, Czerniecki JM, Gambel CJ. Comparison of the Power
Knee and C-Leg during step-up and sit-to-stand tasks. Gait Posture. 2013 Jul;38(3):397-
402.
83. Yoeruek E, Bartz-Schmidt KU. A new knotless technique for combined transscleral fixation of
artificial iris, posterior chamber intraocular lens, and penetrating keratoplasty. Eye (Lond).
2019 Mar;33(3):358-362.

Page 34 of 34
Medical Coverage Policy: 0536
84. Youngblood RT, Brzostowski JT, Hafner BJ, Czerniecki JM, Allyn KJ, Foster RL, Sanders JE.
Effectiveness of elevated vacuum and suction prosthetic suspension systems in managing
daily residual limb fluid volume change in people with transtibial amputation. Prosthet
Orthot Int. 2020 Jun;44(3):155-163.
85. Zachariah SG, Saxena R, Fergason JR, Sanders JE. Shape and volume change in the
transtibial residuum over the short term: preliminary investigation of six subjects. J Rehabil
Res Dev. 2004 Sep;41(5):683-94.
Revision Details
Type of Revision
Summary of Changes
Date
Annual
No changes.
1/15/2024
“Cigna Companies” refers to operating subsidiaries of The Cigna Group. All products and services
are provided exclusively by or through such operating subsidiaries, including Cigna Health and Life
Insurance Company, Connecticut General Life Insurance Company, Evernorth Behavioral Health,
Inc., Cigna Health Management, Inc., and HMO or service company subsidiaries of The Cigna
Group. © 2024 The Cigna Group.
