
/*6&23*480'024)",04"/*6&23*480'024)",04"
$)0-"2-80..0/3$)0-"2-80..0/3
$$51"4*0/"-)&2"18"1340/&3 &1"24.&/40'$$51"4*0/"-)&2"18
)&4*-*480'."240.&&$)/0-0(87*4)*/$$51"4*0/"-)&4*-*480'."240.&&$)/0-0(87*4)*/$$51"4*0/"-
)&2"182"$4*$&)&2"182"$4*$&
8-*& "-4)&23
&33*&!*..&2
07%0&3"$$&33404)*3702,#&/&:4805&453,/07
0--074)*3"/%"%%*4*0/"-702,3"4)4413$0..0/35/%&%504(2"%
&$0..&/%&%*4"4*0/&$0..&/%&%*4"4*0/
"-4)&238-*&"/%!*..&2&33*&)&4*-*480'."240.&&$)/0-0(87*4)*/$$51"4*0/"-)&2"18
2"$4*$&
$$51"4*0/"-)&2"18"1340/&3
)4413$0..0/35/%&%504(2"%
)*3$)0-"2-820+&$4*3#205()440805'02'2&&"/%01&/"$$&33#84)&&1"24.&/40'$$51"4*0/"-)&2"18"4
$)0-"2-80..0/34)"3#&&/"$$&14&%'02*/$-53*0/*/$$51"4*0/"-)&2"18"1340/&3#8"/"54)02*9&%
"%.*/*342"4020'$)0-"2-80..0/302.02&*/'02."4*0/1-&"3&$0/4"$45/%$0..0/3-*#2"285/%&%5
The Utility of Smart Home Technology within Occupational Therapy Practice
by
Kylie Walthers, MOTS and Jessie Zimmer, MOTS
Advisor: Cherie Graves, PhD, OTR/L
Contributing: Marilyn G. Klug, PhD
An Independent Study
Submitted to the Occupational Therapy Department
of the
University of North Dakota
in partial fulfillment of the requirements
for the degree of
Master’s of Occupational Therapy
Grand Forks, North Dakota
May, 2020

ii
Approval Page
This Independent Study paper, submitted by Kylie Walthers, MOTS and Jessie Zimmer,
MOTS in partial fulfillment of the requirement for the Degree of Master of Occupational
Therapy from the University of North Dakota, has been read by the Faculty Advisor
under whom the work has been done and is hereby approved.
_________________________
Faculty Advisor
April 16, 2020
Date

iii
PERMISSION
Title: The Utility of Smart Home Technology within Occupational Therapy
Practice
Department: Occupational Therapy
Degree: Master’s of Occupational Therapy
In presenting this Independent Study in partial fulfillment of the requirements for
a graduate degree from the University of North Dakota, we agree that the Department of
Occupational Therapy shall make it freely available for inspection. We further agree that
permission for extensive copying for scholarly purposes may be granted by the professor
who supervised our work or, in her absence, by the Chairperson of the Department. It is
understood that any copying or publication or other use of this Independent Study or part
thereof for financial gain shall not be allowed without our written permission. It is also
understood that due recognition shall be given to us and the University of North Dakota
in any scholarly use which may be made of any material in our Independent Study
Report.
__________________________
Signature
_________________________
Date
iv
TABLE OF CONTENTS
LIST OF TABLES…………………..................................................................................v
LIST OF FIGURES……………………………………………………………………...vii
ACKNOWLEDGEMENTS..............................................................................................viii
ABSTRACT……………………………………………………………………………...ix
CHAPTER
I. INTRODUCTION………………………………………………………………1
II. REVIEW OF LITERATURE…………………………………………………..5
III. RESEARCH METHODOLOGY.....................................................................31
IV. PRESENTATION & ANALYSIS OF DATA ...............................................45
V. DISCUSSION ..................................................................................................73
REFERENCES .................................................................................................................86
APPENDICES ..................................................................................................................92
Appendix A................................................................................................92
Appendix B................................................................................................97
Appendix C................................................................................................99
v
LIST OF TABLES
TABLE 1: Demographics ……………………………………………………………….48
TABLE 2: Amount of Education Received on SHT …………………..……….……….. 52
TABLE 3: Time Spent Researching SHT ………………………..…………….……….. 54
TABLE 4: Incorporation of SHT into Practice ……………...…………….….……….. 55
TABLE 5: Comfort and Perceived Effectiveness with Using SHT ……..……..……….. 57
TABLE 6: Supports for Using SHT ……………...…………………………………….. 58
TABLE 7: Level of Interest in Using SHT ………...……….………...………..……….. 59
TABLE 8: Perceived Knowledge of SHT …………………………………......……….. 60
TABLE 9: Time and Access to SHT ………………………………....………..……….. 61
TABLE 10: Employer Funding for SHT and Access to Other Funding Sources for
SHT……………………………………………………………………………………... 63
TABLE 11: Correlation between Availability and Degree of Support ………….…….. 65
TABLE 12: Correlation between Availability and Level of Interest ………….……….. 65
TABLE 13: Correlation between Availability and Funding ……………….....……….. 66
TABLE 14: Correlation between Degree of Support and Level of Interest ……..…….. 66
TABLE 15: Correlation between Degree of Support and Funding …………..……….. 67
TABLE 16: Correlation between Degree of Support and Use ……...….……..……….. 67
TABLE 17: Correlation between Sources of Support and Use ……...………..……….. 68
TABLE 18: Correlation between Education and Interest ……....………..……...…….. 68
TABLE 19: Correlation between Interest and Perceived Effectiveness…..…..……….. 69
TABLE 20: Correlation between Interest and Use …………….......................……….. 69
TABLE 21: Correlation between Perceived Knowledge and Comfort …………..…….. 70
TABLE 22: Correlation between Perceived Knowledge and Perceived Effectiveness… 70
vi
TABLE 23: Correlation between Perceived Knowledge and Use ………….………….. 71
TABLE 24: Correlation between Comfort and Perceived Effectiveness …………..….. 71
TABLE 25: Correlation between Funding and Use ………...………………...……….. 72
vii
LIST OF FIGURES
FIGURE 1: Where SHT Education was Obtained ……………..…………….……..….. 53
FIGURE 2: Hours per Week Spent Researching SHT ……………….……….….…….. 55
FIGURE 3: Percentage that Incorporate SHT into Practice ………..………..……….. 56
FIGURE 4: Perceived Effectiveness & Comfort Using SHT ……………...………..….. 57
FIGURE 5: Supports for Using SHT ……………...……….………...………..……….. 58
FIGURE 6: Interest in SHT ……………………………………………….......……….. 59
FIGURE 7: Perceived Knowledge of SHT ………………………......………..……….. 60
FIGURE 8: Availability to Implement SHT ……………...……..…...………..……….. 62
FIGURE 9: Available Funding for SHT ……………...………..…...……………...….. 63
viii
ACKNOWLEDGEMENTS
We would like to express our deepest gratitude and appreciation to our advisor,
Dr. Cherie Graves, for her guidance, support, endless meetings (phone and us stopping by
unannounced to her office) and feedback throughout this process and completion of this
Independent Study. We would also like to thank Dr. Marilyn Klug for her assistance and
expertise in the research process. Lastly, we would like to thank our friends and family
for all their love, support, patience, and understanding throughout the duration of this
process as we could not have completed it without you all.
Kylie and Jessie
ix
ABSTRACT
Title: The Utility of Smart Home Technology within Occupational Therapy Practice
Kylie Walthers, MOTS, Jessie Zimmer, MOTS, & Cherie Graves, PhD, OTR/L, FAOTA.
Department of Occupational Therapy, University of North Dakota School of
Medicine and Health Sciences, 1301 N Columbia Rd, Stop 9037, Grand Forks,
ND, 58202-9037
Purpose: The purpose of this study is to explore occupational therapist practitioners’
(OTPs) utility of smart home technology (SHT) in their practice, as well as to inquire into
the facilitators and barriers of utilization of smart home technology within the practice of
occupational therapy.
Methodology: This study was approved by the Institutional Review Board at the
University of North Dakota (UND) in Grand Forks, ND. A quantitative, descriptive
research design utilizing survey methodology was used. Recruitment was conducted
through purposive and convenience sampling. A 30-question Qualtrics survey was
distributed to participants via social media and internet pages (OT4OT; AT4OT;
CommunOT; and UND OT Alumni page). There was minimal inclusion criteria for the
population recruited. Quantitative data was analyzed using the Statistical Package for
Social Sciences, version 26. The framework guiding this quantitative research study was
the Unified Theory of Acceptance and Use of Technology 2 (UTAUT2) (Venkatesh,
Thong, & Xu, 2012).
Results: A total of 75 surveys were returned, both by occupational therapists (OTs) and
occupational therapy assistants (OTAs). Most of the respondents were female (91%,
n=68) and were OTs (85%, n=64). Most of the respondents practice in the United States
(61%, n=46) working in home health (33%, n=25) and outpatient settings (31%, n=23).
Overall, the respondents reported that they do not currently use SHT in practice (63%,
n=47), that they are somewhat interested in using SHT (34%, n=21), and that most of
their education on SHT is obtained from independent research or study (25%, n=16).
When considering availability, respondents stated that they do not have time (57%, n=43)
or access (36%, n=22) to incorporate SHT. Lastly, available funding and support are
limited as well, with respondents stating they do not have employer (85%, n=52) or other
funding (52%, n=31). Most non-financial support comes from co-workers (n=16) and
family (n=8). Spearman rho correlations were conducted, finding multiple strong
correlations between: the degree of support and who is providing the support (co-
workers, family, etc.); level of comfort with utilizing SHT and effectiveness when
utilizing SHT; types of funding sources available (private, insurance, etc.) and received
amount of funding currently; and received funding and use.
Conclusion: Occupational therapy practitioners are more likely to use SHT in practice if
they have support in a variety of forms, but especially from their co-workers. Interest is
also linked to increased support, increased access to funding, and increased availability.
However, interest was not the driving force for being effective when using SHT. It was
found that comfort with SHT was the driving force for practitioners to perceive they were
effective when using it as an intervention. The most substantial barriers to using SHT that
were identified include: lack of funding sources, lack of education, and lack of
x
availability to the devices. These factors do not need to remain barriers and in fact can
and should become supports to using SHT. Smart home technology should be used in
care and when a practitioner takes a moment to develop interest in the topic, thus
developing a better understanding and knowledge base, they will likely have an increase
in comfort and therefore, perceived effectiveness when using technologies as
interventions. All of these factors assist clients in the long run.
1
CHAPTER I
INTRODUCTION
Rationale
Smart home technology (SHT) is becoming a popular means to assist people in
their daily lives. Various populations may benefit from the use of SHT including
individuals living with disabilities, individuals that wish to age in place, as well as the
general population. Smart home technology can arguably fall into the category of
assistive technologies (Cook & Polgar, 2014) and therefore can be used by occupational
therapy practitioners (OTPs) for therapeutic interventions. There have been calls to action
for OTPs to be using SHT (Waite, 2015) and studies that look at the feasibility of OTPs
using SHT to assist client’s to live more independent and meaningful lives (Giger &
Markward, 2011; Liu, 2018). Despite this, little research has been done investigating
OTPs actual use of SHT and the barriers and supports that OTPs experience influencing
their use or non-use of SHT.
Theoretical Framework
The framework that was used to guide this quantitative research study was the
Unified Theory of Acceptance and Use of Technology 2 (UTAUT2) (Venkatesh, Thong,
& Xu, 2012). The Unified Theory of Acceptance and Use of Technology 2 is a theory
developed by information systems researchers (Venkatesh et al., 2012). This is an
expansion of the Unified Theory of Acceptance and Use of Technology (UTAUT) (Liu et
al., 2015; Venkatesh et al., 2012). The UTAUT2 considers individual characteristics (age,
2
gender, and experience) and constructs (performance expectancy, effort expectancy,
social influence, facilitating conditions, hedonic motivation, price value, and habit) when
assessing and observing the influence on the consumer’s behavioral intention and
behavioral use of technology (Venkatesh et al., 2012). This model has been used in the
past to study the acceptance of new technologies by rehabilitation therapists (Liu et al.,
2015). The Unified Theory of Acceptance and Use of Technology 2 is a well-suited
theory to utilize when examining the relationship of occupational therapy practitioners
and their integration of SHT into practice due to its extensive nature as it looks into
individual characteristics and constructs, and how these may influence the utilization of
technology in occupational therapy practice. The model was chosen when considering
previous literature that was available on the use and non-use of technology and was
determined by the researchers to be a good fit to guide the research process.
Statement of the Problem
Occupational therapists have the opportunity to assist individuals to live
independent and high quality lives through the use of SHT. To further explore the use of
smart home technology in occupational therapy practice, the researchers designed this
quantitative study. The overarching research question is, what is the utility of smart
home technology within occupational therapy practice? The researchers developed two
additional sub-questions:
• What relationships exist (if any) between factors identified and
reported with use of SHT?
• What relationships exist (if any) between factors identified and
reported with perceived effectiveness with SHT?
3
Assumption
Based on the literature review and personal experience, the researchers assumed
that there would be minimal use of SHT by practitioners. In addition, the researchers
assumed that there would be several factors that have influenced the use or non-use of
SHT by OTPs. Factors that were thought to influence use include but are not limited to
availability, funding, and support.
Scope and Delimitation
This study was granted approval by the University of North Dakota’s Institutional
Review Board. The data for this study was gathered via an online survey. Participants
were recruited via social media and online discussion boards. Inclusion criteria for
participants required the individuals to be occupational therapists or occupational therapy
assistants. The survey tool was open for five weeks before being closed for data
analysis.
Importance of the Study
Little research has been done looking at the actual use of SHT by occupational
therapy practitioners and potential facilitators and barriers of using this technology. This
study shows the importance of occupational therapy in this new realm of technologies. In
addition, this study provides objective information regarding why practitioners may not
be using SHT in practice. This information is relevant and important to occupational
therapy practitioners, occupational therapy programs, assistive technology companies,
SHT companies, and consumers of occupational therapy services.
Definition of Terms
The following terminology is used throughout the remainder of this scholarly project.
4
• Assistive technology: “A broad range of devices, services, strategies, and
practices that are conceived and applied to ameliorate the problems faced by
individuals who have disabilities” (Cook & Polgar, 2014, p.460).
• Occupational therapy practitioners: For the purposes of this study, occupational
therapy practitioners (OTPs) are defined as occupational therapists and
occupational therapy assistants.
• Smart home technology: “Any electronic device (including but not limited to
actuators, sensors, computer processors/software, and supporting structures) that
create an integrated system capable of monitoring and supporting individuals in
real-time” (Davenport, Mann, & Lutz, 2012, p. 169).
5
CHAPTER II
REVIEW OF LITERATURE
Technology has become a part of our lives more now than ever before. It has
become embedded within the way people live and work, and even within people’s bodies
and what they choose to wear (Liu, 2018). There is a variety of different forms of
technology, ranging from robotics, the Internet of Things (IoT), artificial intelligence
(AI), 3-D printing, virtual reality, autonomous vehicles, smart home technology, and
much more (Liu, 2018). With the increase of technology in everyday life comes the
increase of opportunities that individuals can utilize technology in assisting with
healthcare. These technologies can be used to assist individuals with and without
disabilities in a variety of ways. According to Liu (2018), healthcare professionals,
including occupational and physical therapy practitioners, were initially slow to use
technology in the rehabilitation process. However, throughout the years, healthcare
practitioners have increased their overall use of technology when providing services for
clients.
When faced with the idea of implementing technologies into healthcare, many
individuals, practitioners and clients alike, quickly revert to the idea of assistive
technologies. Assistive technology encompasses devices, services, and systems that assist
individuals living with a disability to perform designated tasks throughout their everyday
lives (Cook & Polgar, 2014). Assistive technology falls into two categories, high assistive
technology and low assistive technology. High technology involves more complex
6
devices, such as augmentative and alternative communication devices, whereas low
assistive technology devices involve less moving parts, such as Velcro straps or built up
utensil handles.
A more recent form of technology, smart home technology (SHT), has added
greater opportunities for occupational therapy and other professions. While the promise
of smart home technology in rehabilitation fields is great, the complexity of use has
contributed to its slow rise in popularity and slower rate of implementation in practice. In
Sweden, researchers studied the SmartBo project, which utilizes solutions for elderly
with mobility and/or cognitive impairments. Solutions involve utilizing devices and
sensors that control the lighting, windows, doors, locks, water outlets, electrical power
and stove. In addition, visual and tactile signaling devices, Braille displays for the
visually impaired, and speech synthesizers were incorporated (Demiris et al., 2004).
These examples of technology demonstrate how technology can be utilized by healthcare
practitioners to enable a variety of clients to improve their overall functioning and well-
being in the home environment.
These technological advances have brought about opportunities that occupational
therapists can utilize to support client occupational performance and participation. To
have an impact in the realm of advancing technologies and in the future trends of client
care, the occupational therapy profession must understand the technology available and
how it can be used to support client occupational performance and participation. The
scope of technology is extensive and can include many different devices, terminologies,
and definitions. The focus of this inquiry is on the use of smart home technology in
occupational therapy practice.
7
What is Smart Technology
There are many definitions of smart technology. Davenport, Mann, and Lutz
(2012) define smart technology as “any electronic device (including but not limited to
actuators, sensors, computer processors/software, and supporting structures) that create
an integrated system capable of monitoring and supporting individuals in real-time” (p.
169). According to Dermody and Fritz (2019), smart home is a general term used in two
ways: “when referring to consumer-driven in-home smart products (e.g., Amazon’s®
Alexa), or when referring to technology that assists with in-home delivery of healthcare
aging-in-place technologies such as Life Alert®, AngelSense®, GPS Smart Sole®” (p.
2). Data collected from smart home technology can consist of many things, such as
dates, timestamps, sensor labels (e.g., bedroom, a door), sensor states (e.g., ON/OFF),
and activity labels (e.g., sleeping, grooming) (Dermody & Fritz, 2019). Within this paper,
smart technology and smart home technology will be used interchangeably.
Designing a Smart Home and Available Technology
Smart home technology uses two different approaches to provide services;
distributing direct sensing and infrastructure-mediated sensing (Chung, Demiris, &
Thompson, 2016). Distributed direct sensing uses installed sensors in the home for
indicators, whereas infrastructure-mediated sensing uses sensors that are already in place,
such as an air conditioner or electricity use, to sense activity levels within the home
(Chung et al., 2016). These approaches need to be taken into consideration when
designing a smart home system. A smart home system uses multiple smart technologies
within a home’s IoT system to assist an individual in their desired areas of services
indicated by the type of technologies introduced into the home.
8
To begin the design process of a smart home system, the home’s Wi-Fi needs to
have the capability to support the technology. More than one router may be needed
depending on the size of the home and the technologies being used. A mesh Wi-Fi system
uses multiple devices to provide Wi-Fi in all areas of the home, including near the
home’s parameters to allow Wi-Fi to work outside the home (McKeough, 2019). Once
the initial stages of setting up the system(s) have been addressed, there are several
options to control the smart home system. Individual devices can be controlled by
individual apps from a smartphone. Many companies have apps that allow controls to be
used across the company’s specific devices. A virtual assistant is also able to control
basic features, such as turning the lights on and off or controlling a thermostat
(McKeough, 2019). For a more comprehensive control system, a smart hub or bridge is
used. A hub and bridge offer the same services, which is to connect all smart
technologies in one place (Apple Inc., 2019; McKeough, 2019; Smart Home, 2019). This
allows for complete control from a single app. With a hub or bridge, an individual is able
to set up specific controls that can occur daily, such as low lighting when people arrive at
home in the evening or setting the sprinkler system to turn on at a certain time. In
essence, a hub or bridge allows an individual to easily access all of the abilities and
services technology has to offer from a single app. Hubs and bridges are able to connect
with voice assistants as well (Apple Inc., 2019; McKeough, 2019; Smart Home, 2019).
Voice assistants are likely one of the most popular smart devices that are currently
available. There are several prominent companies that make voice assistants that also
make other smart technologies, allowing for ease of interconnection between the
technologies. Voice assistants are able to play music, answer questions, and give
9
reminders, among other things (McKeough, 2019). Smart speakers can connect with a
central voice assistant to provide the services throughout the home (McKeough, 2019).
Smart home technology is able to address almost all aspects of the modern home,
from security, to lighting, to water leaks. Security systems use door sensors, door locks,
motion sensors, and video monitoring to notify an individual of any changes in the
environment as well as allow access to the home (Apple Inc., 2019; McKeough, 2019;
Smart Home, 2019). These devices can be used throughout the home, as well as outside.
For example, a smart doorbell can be used to monitor who enters the home or who is near
the front of the house (McKeough, 2019). Smart sprinkler systems are also available,
allowing a person to turn on the sprinklers at home from anywhere in the world (Apple
Inc., 2019; McKeough, 2019; Smart Home, 2019). Smart garage doors are a common
feature in smart homes as well (McKeough, 2019).
Inside the home there are a variety of technologies that can sense the air, turn on
the lights, and monitor for potential issues (Apple Inc., 2019; McKeough, 2019; Smart
Home, 2019). Smart lighting can be achieved by installing a bulb or a dimmer
(McKeough, 2019). Battery powered window shades are able to work with shades that
are already existing in the home (McKeough, 2019). Smart outlets are also available to
assist in turning on or off appliances that are plugged in, even those that are not
considered to be a smart device (Apple Inc., 2019; McKeough, 2019; Smart Home,
2019). Smart TVs connect to an online network to allow web access and network
channels without the need for cable or satellite. In the area of home safety and comfort,
the following smart devices are available: fans, thermostats, air purifiers, humidifiers,
smoke and carbon monoxide detectors, water leak detection, kitchen appliances, washing
10
machines, access control, and additional indoor sensors (Apple Inc., 2019; McKeough,
2019; Smart Home, 2019). For many of these devices, individuals, including
professionals and clients alike, forget that the devices are considered SHT.
Using Smart Home Technology to Enhance Quality of Life
Smart home technology is used globally by individuals with and without
disabilities. It is considered assistive technology if it is used specifically to assist an
individual with a disability to complete everyday tasks. For example, SHT can be used to
assist an individual who has a cognitive impairment to remember to take their
medications in the morning. A SHT system can be developed to enable an older adult to
age in place safely and negate the necessity of facility placement.
Currently, there are several companies that provide services targeting older adults
and their loved ones who wish to age in place. Aging in place services are made possible
by use of a variety of sensors, video monitoring, artificial intelligence, two way
communication systems, and voices assistants (Orlov, 2019). These technologies are able
to: detect falls, provide reminders, monitor for safety and security, provide
communication with healthcare professionals, call emergency services, communicate
with family, allow for family to check in with their loved ones, and even monitor
cognition (Orlov, 2019). These services may also be an option for individuals of any age,
with disabilities, to live more independent lives.
In addition to using SHT to age in place at home, smart technology is being made
available to use in facilities such as long term care and assisted living (WytCote
Technologies, 2019). Various sensors, wearable technology, and video monitoring can
11
detect movements and actions of residents and staff, fall detection, and facility
operations, such as moisture and water temperatures (WytCote Technologies, 2019).
This technology is able to provide services and support in many parts of home
life. Smart devices are able to assist individuals with all ability levels and needs, and can
provide huge advancements in care when implemented with rehabilitation services. Smart
home technology is likely to be more interconnected and an accepted part of society as it
becomes more advanced and popular, essentially in all aspects of our daily lives and
environments. Occupational therapy practitioners must follow the trend of technology
and the opportunities it can provide, such as promote client well-being and connect
clients to individuals or systems when needed most. There is a considerable amount of
literature that examines use and non-use of assistive technology devices, among users and
practitioners, but literature is lacking specifically related to use and non-use of smart
home technology. There is a need for further study on SHT and the factors influencing
the implementation of such devices among practitioners into client’s everyday lives.
The Occupational Therapy Process: Incorporating Technology
Technologies are influencing our future and will pose new ways for occupational
therapy practitioners to assess and provide intervention services to clients. With the
continued development and increased use of technology devices, it is likely that the role
of occupational therapy and other interdisciplinary team members in relation to
technology will also continue to grow (Verdonck, McCormack, & Chard, 2011).
Occupational therapy practitioners have many different ways they can incorporate
technologies to help clients, such as critically analyzing the details and skills needed to
use technology, choosing and implementing the appropriate technologies for use outside
12
of a clinical setting (ex. work, home), or being a part of a research team that researches
updated technologies (Cook & Polgar, 2014).
When examining an OTs role as part of a research team, Alex Mihailidis - the
Barbara G. Stymiest Research Chair in the rehabilitation technology center at the
University of Toronto and Toronto Rehab Institute - conducts research on pervasive
computing and intelligent systems used in healthcare. Along with one of his team
members, who is an occupational therapist, Alex states that “their primary role is making
sure that we understand the human roles for the technology, looking at the functionality
based on the needs and the skills that the particular client has - the OT really has that
lens” (Waite, 2015).
Ultimately, the goal of occupational therapy when working with clients who are
considering the implementation of home modifications and SHT is to help client’s be as
safe and independent as possible, allowing the client to engage in the activities and tasks
that are meaningful to them (Waite, 2015). The intent for many occupational therapists
when considering the implementation of technology is to meet individual’s needs and
desires to remain independent in their home environment, leading to the use of smart
home technology. With the increase in utilization of smart home technology in
healthcare, it is important to consider what the needs of the client are, which is obtained
through the occupational profile and occupational therapy evaluation, and the
expectations of the individual in regards to technology usage (Cook & Polgar, 2014). If
occupational therapy practitioners fail to take the needs of the client into consideration
while implementing the devices or systems, by only considering the direct features of the
13
technology, they risk adopting approaches that are associated with medical, bottom-up
approaches, and disempowering the client (Cook & Polgar, 2014).
There are many examples in the literature that support the occupational therapy
profession in helping clients who are using smart technology. Occupational therapy
practitioners have the ability to provide interventions in the area of smart technology for a
variety of clients in a wide array of contexts. The following are examples from the
literature of utilizing smart technology for interventions. Occupational therapists can use
compensatory strategies with censored eyewear for left inattention poststroke and use of
interactive games with older adults to understand the functions within a home or
community (Giger & Markward, 2011). There are also devices that assess levels of
engagement in clients who are nonverbal or unable to complete traditional assessments
that measure engagement and alerts on mobile devices for community citizens when a
person, such as an older adult with dementia, goes missing from or within a geographical
location (Giger & Markward, 2011). In regards to smart home technology and
occupational therapy, occupational therapists design smart homes to allow clients to
remain in their natural environments by utilizing universal design principles and
implement smart home monitors to assess client’s abilities to complete activities of daily
living (Giger & Markward, 2011). In addition, occupational therapists can recommend
SHT in the homes of individuals with serious mental illness or cognitive impairments to
assist caregivers in monitoring for safety and to assist these individuals in leading more
independent lives by providing reminders, safety alerts, and monitoring (Giger &
Markward, 2011).
14
With the increasing development and utilization of smart home technology in
healthcare, users currently experience challenges such as continuously developing and
maintaining their knowledge of options, implementation, and maintenance of this type of
technology (Verdonck et al., 2011). In addition, occupational therapists experience
challenges with maintaining a client-centered focus, limiting abandonment of the devices,
and keeping up to date with the emerging products (Verdonck et al., 2011). Occupational
therapists must be aware of and consider the way technologies have changed how basic
and instrumental activities of daily living are performed, making some OT assessments
obsolete (Liu, 2018). Occupational therapists delivering occupation-focused and person-
centered services while utilizing smart home technologies need to know what is available
and how to access and use the technologies with clients. Some common barriers, or
challenges, with implementing technology into OT care will be addressed within the next
sections.
Factors Influencing the Implementation of Smart Home Technology
Literature supports the use of SHT for improving the lives of clients (Davenport,
Mann, & Lutz, 2012), recognizing the impact technology can play in improving an
individual’s quality of life. With that said, the researchers of this study assert that
occupational therapist’s experience factors that influence the implementation of smart
home technology. A small-scale study conducted in Ireland explored occupational
therapist’s responses to a short, five-question survey related to their views on utilizing
technology, perceived competence in this area, and an understanding of whose role it is to
assess for and prescribe such technologies (Verdonck et al., 2011). The researchers found
benefits that occupational therapist’s identified when using advanced technologies in
15
client care. These benefits include improved client independence, increased client self-
esteem, increased participation in occupations, improved personal relationships,
increased safety, decreased level of assistance needed, and overall the technology saved
money for the client and the company (Verdonck et al., 2011).
Although there are benefits to utilizing SHT, there are identified factors that
influence the implementation of technology. Hoogerwerf et al. (2002) assert that high
technologies, such as SHT, is described by practitioners as inconsistent, uncoordinated,
fragmented, and difficult to access. Although Hoogerwerf et al. (2002) was published
almost two decades ago, the researchers assert that these descriptions by practitioners in
regards to technology likely remain similar today, even with the considerable advances in
technology. Additional factors have been identified in the literature as either supporting
or inhibiting the use of SHT. These variables include knowledge (Dicianno et al., 2019;
Hamblin, 2017; Jiancaro, Jaglal, & Mihailidis, 2017; Kumar et al., 2013; Proffitt,
Schwartz, Foreman, & Smith, 2019; Verdonck et al., 2011), personal interest (Verdonck
et al., 2011), workplace culture (Proffitt et al., 2019), and funding (Assistive Technology
Industry Association, 2019; Berridge, 2018; Dicianno et al., 2019; Hamblin, 2017;
Haymes, Storey, Maldonado, Post, & Montgomery, 2015; Verdonck et al., 2011). The
researchers assert that access and time are additional factors that support or inhibit the use
of SHT by healthcare professionals, although further research is needed to add to the
insight of how access and time affect occupational therapy practitioner’s use of SHT.
Knowledge
Knowledge is a necessary component when it comes to implementing any type of
intervention. In the case of SHT, there is conflicting literature regarding the knowledge
16
base that occupational therapy practitioners have when it comes to specialized
technologies. There is literature that supports the knowledge and skill set of occupational
therapy practitioners in the use of SHT in practice (Proffitt et al., 2019). Despite that,
additional literature suggests that occupational therapy practitioners have limited
knowledge in incorporating SHT into interventions and practice (Dicianno et al.,
2019). Proffitt et al. (2019) emphasized the importance of contributing to research and
development in disability-related technology designs. These contributions can be made
by occupational therapists. Occupational therapists have the skill set and knowledge in
the areas of research and universal design, which is a common approach that is
encouraged when engineers and designers are creating technologies. Universal design
requires the expertise of practitioners and professionals who understand all types of
disabilities and impairments, and how to represent individuals with these disabilities
when utilizing technologies for functional tasks (Proffitt et al., 2019).
Limitations of knowledge are also represented in the literature. Although there is
support for occupational therapists to be involved in disability-related technology designs
(Proffitt et al., 2019), there seems to be a lack of knowledge among other working
professionals when it comes to incorporating occupational therapists roles in technology
design. The lack of provider knowledge, whether it be about the technology or the
provision process itself, commonly arises (Dicianno et al., 2019). One barrier that
occupational therapists can encounter is a “language barrier”. Engineers and computer
scientists, as well as occupational therapists, all have their own jargon, creating
difficulties for professionals to communicate effectively about potential collaborations
when implementing technologies (Proffitt et al., 2019). Another barrier addressed in
17
current research is that consumers of the technology, such as occupational therapists and
other healthcare professionals, are not waiting for scientific approval before utilizing
these technology-based interventions (Kumar et al., 2013). This indicates a potential
misuse of technology, such as using tech when it is contraindicated for a client.
Jiancaro, Jaglal, and Mihailidis (2017) surveyed professionals within the fields of
occupational therapy, medicine, and psychology. According to the survey results, there
needs to be a larger role for clinical specialists (such as fields mentioned above) to
introduce and guide practice through models that may help frame and specify a situation
in which technological interventions would be appropriate. This can be done by
educating the clinical specialists. Participants in the survey also indicated that they would
be interested in becoming more educated in this area and could see potential value in
learning and utilizing technology-specific models (Jiancaro et al., 2017). According to
Verdonck et al. (2011), 84% of occupational therapists believed that he or she should be
able to assess for and prescribe higher technologies; however, only 34% were able to do
so. The researchers suggested that this difference may be attributed to lack of opportunity
to be involved during this aspect of care, and/or having little training and knowledge in
this area (Verdonck et al., 2011).
Personal Interest
Occupational therapy practitioners have a unique role in mainstreaming the use of
technologies into the delivery of client care. In addition, practitioners may take on the
role of supplying and maintaining the technologies, which may range from low tech to
high tech devices, including smart home technologies (Verdonck et al., 2011). In order
for an occupational therapy practitioner to build knowledge about SHT, some personal
18
interest in technology and incorporating it into practice is needed. Practitioners that are
more interested in the subject have a greater potential for incorporating the technology
into the intervention process (Verdonck et al., 2011). According to Verdonck,
McCormack, and Chard (2011), occupational therapists indicated that professionals that
provide specialized technologies are not exclusive to specialized practitioners, such as
assistive technology practitioners. Instead, the respondents indicated that they were
interested and capable of incorporating specialized technology (Verdonck et al., 2011).
Workplace Culture
When considering the occupational therapy profession, workplace culture can be
viewed as a factor that starts as far back as our educational programs. Students are shaped
by their educators, fieldwork instructors, and other OT students who have been in the
field (Proffitt et al., 2019). Proffitt, Schwartz, Foreman, and Smith (2019) suggests
students have experiences and opportunities to collaborate with other professionals that
may be implementing technologies with clients or creating designs for technologies, such
as engineering and design peers (Proffitt et al., 2019). Another recommendation provided
by Proffitt et al. (2019) is providing administrative leadership to support the role of
occupational therapy in technology research and development. There are special interest
groups among the American Occupational Therapy Association, webinars, articles, and
conferences held throughout the year on technology implementation (American
Occupational Therapy Association [AOTA], 2019a). However, to advance the role of
occupational therapy in implementing technology, professionals must be leaders; leaders
through program directing, principal investigators, becoming a clinical administrator or
influencing an administrator in order to encourage, teach, inform, and facilitate the
19
participation of technology (Profitt et al., 2019). Additional research is needed to explore
the impact of workplace culture on the use of technology in healthcare.
Funding
Cost is an additional factor that often needs to be considered when implementing
technology with clients. According to a survey distributed to 161 occupational therapists,
the most commonly cited barrier was the intensive process of obtaining insurance
approval for the device, including the cost of the device, the availability of funding, and
the time it takes to obtain authorization and the equipment (Dicianno et al., 2019).
Another aspect reported by Hamblin (2017) is the issue with sustainability of cost and use
when using technologies with older adults. One researcher utilized smart technology at
the start of a study, providing a free service at the start of the fieldwork for one year
(Hamblin, 2017). At the end of the year, clients received a letter indicating that fees
would be introduced. This caused some clients to feel unsure whether they would
continue to use the service or not, stating funding to be the direct barrier (Hamblin,
2017). This prevented practitioners from suggesting and implementing smart home
technologies in the future with other older adults, knowing the potential for high cost
from their past experiences. A similar barrier arose with other professionals, as they came
across similar experiences during the assessment and installation of smart technology
(Hamblin, 2017). Professionals stated that their lack of knowledge on the charging policy
was a distinct barrier and some professionals indicated that they may have misadvised
their clients (Hamblin, 2017).
When private pay is not possible, insurance, both private and public, commonly
cover the cost for medical needs and medical equipment. In the United States, Medicare
20
is a commonly used public insurance that often covers medical equipment. Durable
medical equipment provides a therapeutic benefit for an individual with medical needs.
According to Medicare (2019), durable medical equipment is defined as medical
equipment that can withstand frequent use, is needed for a medical reason, is used in the
home, is typically not useful for an individual that is healthy, and lasts at least three
years. When considering SHT, some devices could fit within these parameters depending
on the individual client’s needs and context. Smart home technology may be deemed
medically necessary for some individuals and potentially be covered by insurance.
Several authors suggest that funding can be established through entities such as
Medicare, Medicaid, the Children’s Health Insurance Program, workers compensation,
TRICARE, state vocational rehabilitation centers, other federal and state programs, a
variety of organizations and nonprofits that offer grants, and private insurance (Assistive
Technology Industry Association, 2019; Berridge, 2018; Haymes et al., 2015).
Although the aforementioned funding sources may be available, it should be
understood that SHT is not commonly covered under medical insurance; as these smart
technologies are recently identified as an intervention in healthcare and not often deemed
medically necessary. When attempting to utilize funding sources, push back can occur
through many different sources and companies. In these instances, occupational therapists
need to utilize their advocacy skills to demonstrate a medical need for the technology and
the potential for improved quality of life for their client if the SHT is funded (J.
Loscheider, personal communication, September 6, 2019).
In Ireland and the United Kingdom, higher technologies, such as smart
technology, is funded through a variety of sources, such as charities and health,
21
employment, and educational services (Verdonck et al., 2011). Another possible funding
avenue is homeowner insurance. Coverage would not be for the upfront cost of the
device, but for protection. Many prominent home insurance companies are providing
coverage for SHT in home insurance plans (American Family Insurance, 2019; Golia,
2019; Kozak, 2018; Ochalla, 2018). The insurance industry is supporting the SHT trend
because of recognized benefits to the home (American Family Insurance, 2019; Golia,
2019; Kozak, 2018; Ochalla, 2018). For example, SHT may provide additional security
protection and more awareness of potential water damage, among other things (American
Family Insurance, 2019; Golia, 2019; Kozak, 2018; Ochalla, 2018). Some insurance
companies may even provide discounts to customers who incorporate smart technology
into their homes (American Family Insurance, 2019; Golia, 2019; Kozak, 2018; Ochalla,
2018).
Ethical Considerations
Ethics are a core part of a healthcare professional’s identity. Occupational therapy
practitioners have ethical responsibilities in relation to incorporating technology into
practice. There is a need to not only keep in mind staying up to date on technology, but
also the need to take specific client ethical concerns into consideration when considering
and implementing new technologies, such as those placed in the home environment. Due
to the dynamic nature of the profession, the evolving healthcare environment, and many
new emerging technologies that are utilized in the therapy setting and home environment,
there are potential ethical concerns in research, education, and practice that must be
considered (AOTA, 2015). According to the Occupational Therapy Code of Ethics
(AOTA, 2015), standard of conduct and principle one of beneficence states that
22
occupational therapy practitioners should “take steps (e.g., continuing education,
research, supervision, training) to ensure proficiency, use careful judgement, and weigh
the potential for harm when generally recognized standards do not exist in emerging
technology or areas of practice” (AOTA, 2015, p.3), such as implementing smart
technology.
Ethical Obligations of Occupational Therapy Practitioners
When examining the occupational therapy profession including the ethical
principles and core values, it is observed that the occupational therapy profession has a
duty to uphold when it comes to implementing technologies into practice (Proffitt et al.,
2019). The Accreditation Council for Occupational Therapy Education (ACOTE)
mandates that occupational therapy practitioners must understand, demonstrate, use, and
teach the use of technology (ACOTE, 2018). Standard B.4.15 states that occupational
therapy practitioners must “demonstrate knowledge of the use of technology in practice,
which must include: electronic documentation systems, virtual environments, and
telehealth technology” (ACOTE, 2018, p. S31). Similarly, Standard B.4.11 states that
occupational therapists should “assess the need for and demonstrate the ability to design,
fabricate, apply, fit, and train in assistive technologies and devices (e.g., electronic aids to
daily living, seating and positioning systems) used to enhance occupational performance
and foster participation and well-being” (ACOTE, 2018, p. S30). Although this is specific
to assistive technologies, it relates to technologies generally, and should be considered
when designing, fabricating, applying, fittings, and training colleagues and clients with
smart technology devices.
Specific Ethical Considerations for Smart Home Technology
23
From an evolutionary perspective, the home is a natural place of comfort. Home
is a place for healing where a person can let down barriers and be themselves. Due to the
level of comfort and protection a home provides, caregivers and patients, tend to prefer
that healthcare and healing take place in the home whenever possible (Burrows, Cotle, &
Gooberman-Hill, 2018) and technologies can now assist people in their endeavor to
receive healthcare at home. The increased availability of technology in the homes has
spurred the need to further explore ethical considerations related to the implementation of
SHT and its impact in the daily life of consumers.
An ethnographic study conducted by Burrows, Cotle, and Gooberman-Hill (2018)
investigated the participant’s navigation of SHT data collection and their borders of
privacy and willingness to share their data. Smart home technology is likely to impede or
change borders of the home with data collection potentially encroaching on privacy,
blurring the lines between what is private information and public data (Burrows et al.,
2018). When data is intentionally being collected by healthcare providers, Burrows et al.
(2018) asserted that individuals may feel that they need to leave an impression when they
know that data is being collected and are likely to not act as they would in their natural
and relaxed state. Individuals participating in this study had a variety of SHT ranging
from health monitoring to energy consumption monitors to home security devices.
Participants in the study indicated that it mattered to them what specific data was shared.
For example, data about certain health practices being shared versus data about energy
consumption within the home being shared. Additionally, the personal contexts and
situations the participants were experiencing affected their willingness to be open and
share their data. Individuals living by themselves, who were also concerned about their
24
personal safety, were more willing to share their data compared to individuals living as a
couple that held the belief that they were able to keep safe because they had each other.
Regarding personal contexts and willingness to share data, there were two groups of
individuals that were more willing to be open to implementing SHT, those familiar with
SHT and individuals who had chronic health conditions that held the belief that sharing
their personal data would assist in better understanding their illness and potentially help
other people in the future (Burrows et al., 2018). Burrows et al. (2018) assert that
frameworks need to be put in place that allow individuals to control and interact with
their data. This will allow for people to maintain the boundaries, privacy, and natural
comfort of the home while sharing the necessary data to ensure they are receiving the full
benefits of their technology and assisting technology in becoming more effective.
Chung, Demiris, and Thompson (2016) completed the first integrative review of
ethics in regards to smart home technologies and older adults. Although their research
mainly applies to older adult use of SHT, it can be easily generalized in other contexts of
SHT use as well. In this study, Chung et al. (2016) reviewed 16 articles published
between 1990 and 2014, which used various research methodologies, although most were
qualitative in nature. The following ethical areas were analyzed by the authors: informed
consent, privacy, obtrusiveness, autonomy, usability, reduction in human touch, social
stigma, and equal access.
Informed consent is an important factor for many aspects when introducing SHT
(Chung et al., 2016), not only the research aspect, but also out of respect and
consideration of the client and potential caregivers, or other individuals that may be
living in the home. Informed consent includes: autonomy, doing no harm, and
25
beneficence. Informed consent is needed due to the nature of SHT collecting intimate,
and private data and information, in order to provide services to the client. Consent is
needed when considering SHT interventions, designing a SHT system, and installing
SHT. In the case of older adults, more care needs to be taken in the event of cognitive
decline or dementia. Caregivers need to be given all the information and facts of the risks
and benefits of introducing SHT systems. It is best if informed consent is obtained in all
steps of the implementation process to ensure that caregivers and clients are making the
best decisions for their circumstances.
Privacy is becoming even more important when considering the introduction of
new technologies into one’s life and home. Smart home technology is designed to collect
data and information of the client and their home in order to provide services and actions
that will assist the client in a variety of ways (Burrows et al., 2018). Due to the nature of
the SHT, there is a risk for privacy to be violated and for an individual to be taken
advantage of (Chung et al., 2016). Because of these circumstances, privacy was found to
be the core concern of older adults when considering introducing technology into their
home. Participants indicated that they did not want others to know, and potentially
criticize, their patterns or specific actions throughout the day. However, participants
indicated that they would be willing to give up some privacy if the SHT enabled them to
be more independent in their home (Chung et al., 2016).
Obtrusiveness of SHT impeding into the life and privacy of an older adult was
also identified when conducting the review (Chung et al., 2016). Elements of
obtrusiveness specifically included privacy, human interaction, usability, function,
sustainability, physical aspects, routine, and self-concept. Participants indicated that the
26
installation process was obtrusive as well as specific locations of the technology, such as
the bedroom. Additionally, noise and lighting of the technology was seen as an issue.
Participants were also against the installation of video monitoring systems into their
homes (Chung et al., 2016).
As SHT is introduced into the lives of individuals, caregivers and clients, they are
likely to become accustomed to the services the technology provides. The authors
considered participants autonomy and potential decrease in human touch for the client
after installation of SHT. In many cases, the SHT is introduced to reduce the cost of
care. Chung et al. (2016) assert that individuals, namely caregivers of older adults, may
become too dependent on technology; for example, only using remote monitoring of the
client. If this is the case, older adults may face an increase of technological interactions
and a decrease in human interactions and human touch. This may be a detriment to the
wellbeing of the older adult. Older adults indicated that they place a high value on human
touch and they did not want the possibility of technology replacing those experiences.
Participants imply being more accepting of a technology that initiates human contact
instead of reducing it. With this in mind, before the implementation of SHT, costs, all
aspects of care, and the use of SHT to assist in the care of an older adult should be
contemplated in order to maintain the best quality of life for the individual (Chung et al.,
2016).
Ethics are an important part of the practice of occupational therapy and should not
be put to the wayside when implementing SHT interventions. Ethical considerations
especially need to be made in the areas of keeping to the occupational therapy
professional standards, privacy, autonomy, usability, reliability, access, social stigma,

27
obtrusiveness, informed consent, and potential loss of human interactions (Chung et al.,
2016). The potential for blurring the lines between public and private data, as well as the
client’s personal comfort in their own home should also be considered (Burrows et al.,
2018). The client’s individual context, needs, abilities, and experiences should always be
kept in mind when looking at the ethical aspects of incorporating a SHT system.
Models: Connecting Models & Technology Together
Theoretical models, frames of reference, and frameworks are an essential part of
modern occupational therapy practice. These tools assist therapy practitioners with
thinking about multiple factors but also guides clinical reasoning and how he or she
views a client. This ensures a more client centered and holistic practice that meets the
client’s needs and wants. Though there are no specific models, frames of reference, or
frameworks targeted specifically to occupational therapy and SHT, there are existing
ones in and outside of OT practice that can guide a therapist in using SHT throughout the
OT process. The Human Activity Assistive Technology (HAAT) model has been used
since the mid-90s to aid occupational therapists and assistive technology practitioners in
matching clients with assistive technology that meets their wants and needs (Cook &
Hussey, 1995). The model emphasizes the client, in a chosen environment, and
participating in an activity. It is designed to highlight the client’s abilities and the
selection of technology to enable the needs and wants of the individual (Cook & Polgar,
2014). As a part of the human component of the HAAT model, professionals consider
client factors such as affect, cognition, motor ability, sensory ability, and experience of
using technology (Cook & Polgar, 2014). Parts of the context that are assessed include:
institutional, social, physical, and cultural (Cook & Polgar, 2014). The activity demands
28
that are considered include cognition, manipulation, and communication (Cook & Polgar,
2014). The HAAT model can be used by OTs to assess and recommend SHT that fits the
needs, wants, and goals of the client. This model is suited for this because of the
emphasis placed on the client and the activity. The client’s abilities are extensively
assessed as well as the context and activity that needs to be addressed. This directly
correlates with a smart home system as the systems are customizable to each individual,
perhaps even more individualized than the typically thought of assistive technology.
Another model, or design system, used by occupational therapists is universal
design. The goal of universal design is to meet the needs of the broadest population. It is
associated with lower cost overall and requires professionals to utilize their expertise in
understanding all types of impairments and how they present across all functional tasks
(Liu, 2018; Proffitt et al., 2019). Universal design should be at the forefront of the mind
when constructing a smart home for a client. Many spaces that utilize SHT are
constructed using universal design principles such as using SHT to track or assist
occupants in precise, non-intrusive ways (Liu, 2018).
The Unified Theory of Acceptance and Use of Technology 2 (UTAUT2), is a
theory developed by information systems researchers (Liu et al., 2015; Venkatesh,
Thong, & Xu, 2012). This is an expansion of the Unified Theory of Acceptance and Use
of Technology (UTAUT) (Liu et al., 2015; Venkatesh et al., 2012). The UTAUT2 takes
individual characteristics (age, gender, and experience) and constructs (performance
expectancy, effort expectancy, social influence, facilitating conditions, hedonic
motivation, price value, and habit) when assessing and observing the influence of these
characteristics and constructs on the consumer’s behavioral intention and behavioral use
29
of technology (Venkatesh et al., 2012). Liu et al. (2015) used the UTAUT model to
examine factors that affect acceptance behavior and actual use of new technologies for
rehabilitation by therapists. Using the lens of this model, they found statistical support to
assert that rehabilitation professionals did not feel pressured from their co-workers to use
technologies, but ultimately utilized technologies because they were useful and/or helped
the clients (Liu et al., 2015). They also found that the expectation of having better patient
outcomes and increased job performance of the therapist, outweighs the hurdles of
learning to use new challenging technologies in practice (Liu et al., 2015). The Unified
Theory of Acceptance and Use of Technology 2 is a well suited theory to utilize when
examining the relationship of occupational therapy practitioners and their integration of
SHT into practice because of the extensive nature of the theory as it looks into individual
characteristics and constructs, and how these variables may influence the use of
technology.
Summary
As evidenced in the above pages, technology is ever-changing and will continue
to evolve in the future. Similarly, occupational therapy is a constant ever-changing
profession and leaders in the profession during this constant ever-changing era can and
should embrace the opportunities that technologies provide (Liu, 2018). As Liu (2018)
states “occupational therapists cannot be leaders in this new era unless we set aside our
fears and embrace the potential benefits of technologies” (p. 281). Occupational therapy
practitioners can bring many diverse, creative solutions to the table when implementing
technologies into client care, and can bring their expertise and understanding of the client
30
and human occupation into the discourse, design, and implementation of technologies
(Liu, 2018).
When occupational therapy practitioners show interest and see the benefits of
technology in care, they set the stage for the profession as a whole, as they are able to
offer more intervention strategies and see a wide range of clients with and without
disabilities. Although barriers to implementing technologies, such as access, time,
funding, workplace culture, personal interest, and knowledge, can deter occupational
therapy practitioners from using technologies, these same barriers can also be facilitators
if the practitioner seeks out these opportunities. Occupational therapy offers a unique
perspective to the smart technology industry and the profession, as they have the potential
to be gatekeepers, whether working directly with clients or assisting in the process of
developing technologies (Hayden, 2019). With the help of models of practice and guiding
Code of Ethics (AOTA, 2015), occupational therapists already have facilitators in place
to guide technology-based interventions with clients.
31
CHAPTER III
RESEARCH METHODOLOGY
The purpose of this study was to explore occupational therapy practitioners’
utility of smart home technology in their practice. Additionally, the student researchers
inquired into the factors that influence their use or non-use of this technology. Our
specific sub research questions are as follows:
• What relationships exist (if any) between factors identified and reported with use
of SHT?
• What relationships exist (if any) between factors identified and reported with
perceived effectiveness with SHT?
The results of this project provide an understanding of occupational therapy
practitioner’s perspectives on smart home technology (SHT), as well as facilitators and
barriers that commonly arise when using SHT. The research study followed a quantitative
research design utilizing survey methodology. A quantitative internet survey was chosen
because it is flexible and is the most common delivery method used to gather data on
healthcare professionals (Blessing, 2016). Three key advantages to using internet surveys
are (1) the sample size can be large and dispersed, (2) a large amount of data can be
collected, and (3) internet survey results can be downloaded to a database, eliminating
data entry and its associated errors, time, and costs for gathering data (Blessing, 2016). In
addition, a descriptive research design was used, more specifically a correlational
32
research design. This type of design is used to inquire about relationships between at least
two variables (Taylor & Kielhofner, 2017).
The framework utilized to guide this quantitative research study was the Unified
Theory of Acceptance and Use of Technology 2 (UTAUT2) (Venkatesh, Thong, & Xu,
2012). The UTAUT2 is a theory developed by information systems researchers and
considers individual characteristics and constructs, of people and technology, when
evaluating the influence on the consumer’s behavioral intention and behavioral use of
technology (Venkatesh et al., 2012). The UTAUT2 was compatible to employ when the
researchers explored the relationship of occupational therapy practitioners and their
integration of SHT into practice, due to the fact that the theory’s extensive nature looks at
individuals and technology concurrently.
Locale of the Study
After gaining approval from the University of North Dakota’s Institutional
Review Board (IRB), the researchers sent out requests for survey participation virtually.
Specifically, social media was chosen to accommodate for participants all around the
world and for ease of access after work hours. A 30-question Qualtrics survey was
distributed to participants via social media pages, which included occupational therapy-
based Facebook pages that the researchers gained access to first before posting about the
survey. The sites included: OT4OT; AT4OT; and the University of North Dakota
Occupational Therapy Alumni page. A site that is not affiliated with Facebook that the
researchers also posted the survey on was CommunOT, which is an occupational therapy
blog site through the American Occupational Therapy Association (AOTA). It is a place
for AOTA members to interact, engage, and share to build a professional online
33
community through asking questions and posing other discussion topics regarding current
care provided in the field (AOTA, 2019b). By using social media sites as an outlet, this
study was able to reach multiple participants of different geographic locations across the
globe, with possible differing cultural backgrounds.
Population/Sampling
There was minimal inclusion criteria for the population recruited; however, the
participants had to be occupational therapists or occupational therapy assistants who were
interested in providing their perceptions on smart technology by taking the online survey
tool. Participants did not have to be a certified Assistive Technology Practitioner (ATP),
and did not have to be currently utilizing smart technology in practice. Practitioners could
participate in the study regardless of gender, age, location in the world, area of practice or
population most treated, level of educational degree, years of experience in the
occupational therapy field, and experience with the use of technology, including smart
home technologies. Recruitment was conducted through purposive and convenience
sampling. Purposive sampling is done when the researcher seeks out potential
participants based on specific criteria (Porteny & Watkins, 2015). This was done in this
project and is represented in the fact that the researchers chose Facebook groups and
CommunOT because they were specific to OT practitioners, which is a part of the
inclusion criteria. Convenience sampling occurs when participants are recruited based on
availability (Porteny & Watkins, 2015). This is represented in this project because the
researchers reached out to potential participants via Facebook groups and CommunOT
and whoever was available to participate could, if they fit the inclusion criteria.
Survey Construction
34
When creating the survey tool, the researchers aimed to discover how often OT
practitioners were using SHT and what factors were identified as facilitators or barriers to
the use of technology. The questions were based on the fieldwork experiences of the
student researchers, personal educational experiences, and a thorough review of the
literature. The questions were not intended to be exhaustive. When conducting the
literature review the researchers found several variables that stood out to be either a
barrier or support for occupational therapy practitioners in their use of SHT. These
variables include knowledge (Dicianno et al., 2019; Hamblin, 2017; Jiancaro, Jaglal, &
Mihailidis, 2017; Kumar et al., 2013; Proffitt et al., 2019; Verdonck et al., 2011),
personal interest (Verdonck et al., 2011), workplace culture (Proffitt et al., 2019), and
funding (Assistive Technology Industry Association, 2019; Berridge, 2018; Dicianno et
al., 2019; Hamblin, 2017; Haymes, Storey, Maldonado, Post, & Montgomery, 2015;
Verdonck et al., 2011). In addition to the variables above, the researchers assert that
access and time are additional factors that support or inhibit the use of SHT by healthcare
professionals. The access and time variables were not mentioned in the literature that the
researchers reviewed. Because of this, the researchers made sure to add these factors to
the survey tool.
Several different question designs were used including multiple choice, checklist,
Likert, verbal frequency scales and open text entry. With checklist questions, the
participant was able to choose more than one answer that was provided. Likert scales are
of ordinal design and used to obtain participant’s thoughts on the question posed with
values for the answer choices (Blessing, 2016). Verbal frequency scales are similar to
Likert scales but may use more answer choices and do not include values (Blessing,
35
2016). The open text entry options allowed participants to provide additional relevant
options.
The survey tool included eleven demographic list response questions, both
multiple choice and checklist. The questions ranged from age, educational degree, and
country, to populations served and settings of practice. Next, three questions were
designed to analyze where participants learned about SHT, how much time they have
spent researching SHT, and if they have used SHT in their practice. A juxtaposed verbal
frequency scale was utilized to inquire about where participants learned about SHT.
Potential answers ranged from occupational therapy school, in-services, and conferences.
Multiple choice questions were used to find out about how much time researching SHT
was spent by the participant and if he or she used SHT in practice. If the participant
answered “no” to the use of SHT in practice, they were moved to the next block of
questions, in contrast, if they answered “yes”, there were several additional questions in
the block relating to the participant using SHT in practice. A verbal frequency scale was
used to find out how often the participant used SHT in practice and a multiple choice
question asked how many years he or she had been using the technology in practice.
Likert scales were used to ask about the participants comfort with using SHT and
perceived effectiveness with using SHT. Additionally, we utilized checklist questions to
inquire about funding sources the participant used to access SHT for his or her clients, as
well as supports the participant had for utilizing SHT with clients. In the next block of
questions, we wanted to learn about the participant’s interest in SHT and more specific
variables of barriers and supports. The researchers utilized a verbal frequency scale to
measure participants' interest in SHT. Verbal frequency scales were also used to measure
36
interest in researching SHT as well as the participants' perceived knowledge about SHT.
Next, multiple choice questions were used to ask about additional factors including: time
the participants had for researching SHT; how much access to SHT the respondent had; if
the respondent’s employer provided funding for the respondent to use SHT with clients;
and if the respondent had any additional funding sources. Lastly, a verbal frequency scale
was used to inquire about how much the respondent’s workplace supported the use of
SHT.
Instrumentation and Data Collection
The 30-question survey tool was built into Qualtrics survey software (see
Appendix A), which was chosen based on its confidentiality, dependability, and ease of
access to the researchers. When building the survey, the researchers examined the survey
through many lenses. The two student researchers, the research advisor, and an associate
professor in population health, who specializes in working with IBM Statistical Package
for the Social Sciences (SPSS), all analyzed and reviewed the survey for further edits
before submitting to the Institutional Review Board. Once approval was received from
the University of North Dakota’s Institutional Review Board (see Appendix B), the
surveys were made available on social media sites via link connecting to the survey tool
in Qualtrics. An informed consent document (see Appendix C) immediately preceded the
beginning of the Qualtrics survey. Surveys were recorded and stored in the University of
North Dakota’s Qualtrics Survey Software. This data was stored in a password protected,
institutional folder where only the researchers and the researcher’s advisor could access
the data to protect the confidentiality of the participants. The survey remained open for
five weeks, and the researchers were available to participants via email, phone, and social
37
media messaging if the participants had any questions, concerns, or problems based on
taking the Qualtrics survey.
Tools for Data Analysis
After the closure of the survey, the data was downloaded from Qualtrics into an
Excel file, which was then converted and uploaded into a statistical software package. All
of the statistical tests were run with SPSS, version 26 which is the most recent version
available. There were a variety of tests run when completing data analysis, including
descriptive frequencies and Spearman rho correlation coefficients.
Data that was classified as demographic information was analyzed by running
descriptive statistics to identify the frequency distribution and percentage values.
Descriptive frequencies were chosen to analyze demographic data to show distributions
for the specified variables (Cronk, 2017). Descriptive frequencies were also ran on the
variables of perceived effectiveness when using smart home technology, education
(amount of education and amount of research) gained on smart home technology,
supports (e.g. through employers, funding, and workplace atmosphere) for using smart
home technology, personal use (e.g. how often is he/she is utilizing in practice, comfort
with implementing, level of personal interest and knowledge of smart home technology in
practice, and availability (access and time available) to utilize smart home technology
and resources. The output includes the number of occurrences, percentages, valid
percentages, and cumulative percentages (Cronk, 2017).
Running descriptive frequencies and percentage values helped the researchers to
draw conclusions based on describing the numbers or percentages of cases in the sample
based on the variables being examined. The descriptive statistics provided information
38
from the data regarding the number of individuals responding in relation to the specified
variable (n), range of values, minimum and maximum values, mean value, and standard
deviations. All of these descriptives were reviewed to help the researchers get a full
understanding of the population sample. The valid percentages and the cumulative
percentages comprise only the data that are not designated as missing. Valid percentages
give the percentage of records (without including records with missing data) for each
value, whereas cumulative percentages indicate the percentage of records with a score
equal to or smaller than the current value (Cronk, 2017). Thus, the last value is always
100%. The frequencies command is useful for describing samples where the mean is not
useful (Cronk, 2017). It is also useful as a method for getting a better understanding of
the data, and it provides more information than just a mean and standard deviation
(Cronk, 2017). Along with the above reasons for choosing descriptive frequencies, it also
helps to determine skew and identifying outliers (Cronk, 2017). Thus the reason for
choosing descriptive frequencies.
When the researchers analyzed their initial thoughts at the beginning of this
project, there were several areas that the researchers thought would stand out in relation
to barriers and facilitators when utilizing SHT. These areas were: perceived effectiveness
when using SHT, where SHT education was obtained, personal use of SHT in practice,
support to use SHT, access to SHT, and time to implement SHT in practice. As
mentioned previously, the researchers worked with an associate professor who
specializes in statistics and works as a consultant with the occupational therapy
department. The professor assisted in narrowing the 30 questions in the survey tool into
variables that were formed from the areas mentioned above. The variables will be
39
referred to as availability (access and time), support, education, interest, knowledge,
comfort, effectiveness, funding, and use from now on... The survey questions that formed
each variable are described below. In the results of the data analysis (chapter 4), the
relationships between these variables is described further.
Availability (Access and Time)
• Question 26: “Do you feel that you have time to implement smart home
technology with clients?”
• Question 27: “Do you have access to smart home technology products and
resources?”
Support
Support is divided into three different support variables. If a respondent checked
“no supports” (Q21), and gave no rating (Q30), they received a 0. If they had supports in
place, but no rating, they got the number of supports as their score. If they had a rating
but did not list supports, they got their rating as a score. Otherwise, the score was the
multiple of the number of supports and their rating of them (ranging from 0 to 12). The
second support variable was put into a support level, meaning the support variable was
categorized into 4 levels: 0, 1, 2, 3+. Finally, the third support variable was whether they
simply stated “yes” or “no”, indicating they do have some level of support.
• Question 21: “Identify supports you have encountered regarding the use of smart
home technology.”
• Question 30: “Rate the level of support within your place of work in utilizing
smart home technology.”
40
Education
• Question 12: “Identify the amount of education you have gained about smart
home technology through the following means.”
Interest
• Question 22: “Rate the level of personal interest in using smart home
technology.”
• Question 24: “Rate your interest in researching more about smart home
technology use.”
Knowledge
• Question 25: “Rate your knowledge on smart home technology.”
Comfort
• Question 18: “Rate your comfort with using smart home technology.”
Effectiveness
• Question 19: “Rate your effectiveness in utilizing smart home technology.”
Funding
• Question 20: “What sources of funding have you utilized to access smart home
technology for clients?”
• Question 28: “Does your current employer provide funding for trial use of smart
home technology with clients?”
• Question 29: “Do you have access to other funding sources (outside of employer
support) for implementing smart home technology (i.e. grants, insurance)?”
41
Use
Use was divided into three variables. The first being if a participant answered
“yes” to Q15 (uses SHT) then the score was the sum of their frequency of use (Q16) and
the number of years they have used it (Q17). Then, Q17 was subtracted by 1 to only add
to the Q16 score if they had been using more than 5 years. The second and third use
variables were divided into use of SHT levels: 0,1, 2, and 3+, and a “yes” or “no” answer
based on Q15.
• Question 15: “Do you incorporate smart home technology into practice?”
• Question 16: “How often do you use smart home technology in your OT
practice?”
• Question 17: “How many years have you been utilizing smart home technology in
your OT practice?”
The researchers wanted to examine the relationships between perceived effectiveness
of the occupational therapy practitioner with utilizing SHT, education received on SHT,
support to use SHT, the use of SHT in practice, and availability to SHT and resources by
utilizing inferential statistical tests. The Spearman rho correlation coefficient was chosen
to determine if any relationship was present between the above mentioned variables, and
whether the relationship presented itself as a facilitator or barrier to utilizing smart home
technology in practice. The Spearman rho correlation coefficient (sometimes called
Spearman rho) determines the strength of the relationship between two variables (Cronk,
2017). A correlation coefficient will be between -1.0 and +1.0, with coefficients close to
0.0 representing a weak relationship and coefficients close 1.0 or -1.0 representing a
strong relationship (Cronk, 2017). A significant correlation indicates a reliable
42
relationship, but not necessarily a strong correlation (Cronk, 2017). Generally,
correlations with an absolute value greater than 0.7 are considered strong, whereas
absolute values less than 0.3 are considered weak and correlations with an absolute value
between 0.3 and 0.7 are considered moderate (Cronk, 2017).
Reliability and Validity
In order to answer the gaps in the literature on this topic, it was necessary for the
researchers to create an innovative survey tool, thus the tool used in this project was an
unstandardized questionnaire. Unstandardized questionnaires have not been used or
tested previously and therefore do not have data that support or refute their use (Taylor &
Kielhofner, 2017). Hence, it is not possible to establish true reliability and validity of the
tool that was developed. Although the researcher’s tool has been created to answer the
identified specific research questions and the tools reliability and validity is not able to be
measured, the researchers have created a quality survey to accurately measure data. This
was done by minimizing bias in the design of the survey. It is important to avoid bias in a
questionnaire so the most accurate data can be collected from the participants (Choi &
Pak, 2005). Bias can occur when there is miscommunication between what the
investigators are asking and what the participants are perceiving what they are being
asked (Choi & Pak, 2005). Bias as a whole can occur because of the design of individual
questions as well as the design of the entire survey (Choi & Pak, 2005). The researchers
conducted many information sessions with not only each other, but with their advisor and
consulting associate professor to minimize biases.
The researchers minimized bias in the design of the survey by using multiple
methods. Choi and Pak (2005) identified numerous types of bias. With the survey design,
43
it was possible to avoid bias in the areas of wording, missing or inadequate data for
intended purpose, inconsistency, formatting problems, and questionnaire length. Wording
bias was averted by refraining from double-barreled and ambiguous questions, rather the
researchers used clear and concise wording. The bias of missing or inadequate data for
intended purpose was circumvented by ensuring sensitive measures. This was done by
giving multiple categories to choose from to avoid type II errors, which is not reporting a
relationship between two variables where there is one (Taylor & Kielhofner, 2017). In
addition, the researchers made sure to use several intervals ensuring all potential choices
were represented and did not overlap any intervals, contributing to the accuracy of each
category. Inconsistency bias was deflected by remaining consistent with the types of
scales and wording present in the questions.
Formatting problem bias using vertical response formats for listing type questions
was used to avoid responder confusion due to the fact that horizontal response formats for
listing questions may cause confusion with spacing and has a higher likelihood of
incorrect answers being selected (Choi & Pak, 2005). In addition, right alignment
questions were utilized by placing the response choice before the response word. This
makes it easier for the respondent to read more easily (Choi & Pak, 2005). The bias of
questionnaire length was eluded by limiting the amount of yes and no questions and
keeping the survey short. This also assisted in avoiding response fatigue by keeping the
survey completion time to approximately 15 minutes. Surveys should not be longer than
20 minutes (Choi & Pak, 2005). In addition, when it was appropriate for the respondent
to skip questions, automatic question skipping was utilized within the software to avoid
confusion and unintentional skipped questions.
44
Summary
The steps described above outlined the process that was used through the course
of this study to ensure that quality data was produced. Each member of this research team
took significant time to process through the details of this study from start to finish to
ensure that the resulting data could be used to explore and expand the role of
occupational therapy practitioners with implementing smart technology into their practice
now and in the future. The following chapter outlines the findings from the research.
45
CHAPTER IV
PRESENTATION & ANALYSIS OF DATA
Much has been published regarding the usefulness of smart home technology for
clients, as well as pieces encouraging healthcare professionals to use SHT. In contrast,
there is limited literature that examines the perspectives of occupational therapy
practitioners (OTPs) use of SHT. The researchers recognize that there is a need for SHT
to be utilized in OT practice, but the researchers wanted to understand further the
utilization of SHT by OTPs. This quantitative descriptive study primarily sought to
survey participant’s perceptions of SHT, and to determine facilitators and barriers to the
implementation of SHT into practice. Results are presented through descriptive
frequencies and correlations. Findings are discussed in more detail in the discussion
section (Chapter V).
At the commencement of this study, the researchers hypothesized that supports
and barriers impacting use of SHT, would be identified by OTPs. The overarching
research question is “what is the utility of smart home technology within occupational
therapy practice?”. Two additional sub-questions were developed which are as follows:
• What relationships exist (if any) between factors identified and
reported with use of SHT?
• What relationships exist (if any) between factors identified and
reported with perceived effectiveness with SHT?
Descriptive Demographics
46
Descriptive frequencies were run to get a more thorough explanation of the
demographics of the data set. Participation of both occupational therapists (OT) and
occupational therapy assistants (OTA) were both permitted in this research
study. Seventy-five people completed the survey. Participants included five males, 68
females, and one participant preferred not to answer. Participants included 63 OTs and 2
OTAs. The geographical area of the practitioners were split into two categories, rural
(n=29) and metropolitan (n=41). Highest level of education achieved by participants
included bachelors degrees (n=24), masters degrees (n=31), research doctorate degrees
such as Ph.D. or Ed.D. (n=4), and occupational therapy clinical doctorate degrees (n=9).
Age of participants included, 20-30 (n=20), 31-40 (n=15), 41-50 (n=19), 51-60 (n=12),
and 61+ (n=6). One participant preferred not to answer the question. Years of practice
experience included, 1-4 years (n=18), 5-10 years (n=9), 11-15 years (n=9), 16-20 years
(n=7), 21-25 years (n=12), and 26+ years (n=14).
The age of populations served by the practitioners varied, pediatrics (n=26),
adolescents (n=19), adults (n=43), and older adults (n=47). Practice settings identified by
participants include: inpatient/acute (n=16), outpatient (n=23), skilled nursing
facility/transitional care unit (n=8), school system (n=13), home health/in-home care
(n=25), and other (n=17). The practitioner’s identified the focus of their practice using
the American Occupational Therapy Association’s (AOTA’s) practice areas. Identified
practice areas include: children/youth (n=22), health and wellness (n=15), mental health
(n=8), productive aging (n=18), rehabilitation and disability (n=47), and work and
industry (n=5). Thirty-eight participants identified as being a certified Assistive
47
Technology Practitioner (ATP). Please see Table 1 below for a visual summary of the
demographics.

48
Table 1
Demographics
Variable
N
Percentage
Gender
Male
5
6.7%
Female
68
90.7%
Age
20-30 years old
20
26.7%
31-40 years old
15
20.0%
41-50 years old
19
25.3%
51-60 years old
6
17.3%
61+ years old
1
8.0%
Prefer not to answer
1
1.3%
Type of Practitioner
Occupational Therapist
64
85.3%
Occupational Therapy
Assistant
2
2.7%
Assistive Technology
Practitioners
3
4%
Live United States
46
61.3%
Living Internationally
18
38.7%
Serve Rural Populations
29
38.7%
Serve Metropolitan Populations
41
54.7%
Years of Practice
1-4 years
18
24%
5-10 years
9
12%
11-15 years
9
12%
16-20 years
7
9.3%
21-25 years
12
16%

49
25+ years
14
18.7%
Level of Education
Bachelors degree
24
32%
Masters Degree
31
41.3%
Research Doctorate
4
5.3%
Clinical Doctorate
9
12%
Populations Served
Pediatrics
26
34.7%
Adolescence
19
25.3%
Adults
43
57.3%
Older Adults
47
62.7%
Setting of Practice
Inpatient/Acute
16
21.3%
Outpatient
23
30.7%
Skilled Nursing Facility
8
10.7%
School System
13
17.3%
Home Health
25
33.3%
Other
17
22.7%
Area of Practice
Children/Youth
22
29.3%
Health and Wellness
15
20%
Mental Health
8
10.7%
Productive Aging
18
24%
Rehabilitation and Disability
47
62.7%
Work and Industry
5
6.7%
50
Descriptive Statistics
Descriptive frequencies were run on all questions presented in the survey. The
researchers identified select questions to present below. The output includes the number
of occurrences (frequencies), percent’s, and valid percent’s. The valid percentages and
the cumulative percentages comprise only the data that are not designated as missing.
Please see Chapter Three: Methodology, for a complete description of what these values
mean, and how to interpret them in relation to the data. Presentation of the data set below
is explained using frequencies (n) and valid percentages, when percentages are presented.
Participants were asked to identify the amount of education they have gained
about smart home technology while in OT school, through independent research/study,
through informal in-services (such as lunch and learns, etc.), general continuing
educational conferences, continuing educational conferences that focused specifically on
smart home technology, and other, which was provided for alternate responses that were
not listed by the researchers. Participants were asked to rate the amount of education they
had received on a 5-point Likert scale (1=no education; 5=significant education). Sixty-
seven participants responded to the question inquiring about the amount of education
gained while in occupational therapy school. Fifty-two percent received none, 30%
received little education, 10% received some education, 5% received a lot of education,
while 3% received significant education on SHT while in OT school.
The same 5-point Likert scale was used to identify education received on SHT
through independent research and study opportunities, 64 participants responded with
22% indicating they received no education, 23% received little education, 25% received
some education, 25% received a lot of knowledge, and only 5% responded receiving
51
significant education on SHT through their own independent research and study
opportunities.
Occupational therapy practitioners gain education on SHT through informal in-
services, such as lunch and learns. Of the participants (n=66) that answered this question,
41% received no education, 33% received little education, 23% received some education,
2% received a lot of education, and 2% received significant education.
General and specialty continuing education conferences provide educational
opportunities for occupational therapy practitioners. General conferences typically
provide information covering several topic areas, whereas specialty conferences provide
in-depth education focusing on a specific topic. When inquiring about general continuing
education conferences (n=66), 29% received no education, 36% received little education,
27% received some education, 6% received a lot of education, and only 2% received
significant education on SHT through general continuing educational conferences.
Specialty continuing education conferences may cover more specific topics which
could include smart home technology. Of the 64 participants, 44% received no
education, 28% received little education, 17% received some education, 11% received a
lot of education and zero participants reported receiving a significant amount of
education on SHT through specialty continuing education conferences. See Table 2 and
Figure 1 for visual representation of the data.

52
Table 2
Amount of Education Received on SHT
Variable
N
Percentage
While in OT school
No education
35
52.2%
Little education
20
29.9%
Some education
7
10.4%
A lot education
3
4.5%
Significant education
2
3%
Independent research/study
No education
14
21.9%
Little education
15
23.4%
Some education
16
25%
A lot education
16
25%
Significant education
3
4.7%
Informal in-service
No education
27
40.9%
Little education
22
33.3%
Some education
15
22.7%
A lot education
1
1.5%
Significant education
1
1.5%
General continuing education Conference
No education
28
43.8%
Little education
18
28.1%
Some education
11
17.2%
A lot education
7
10.9%
Significant education
0
0%
Other
No education
13
61.9%
Little education
3
14.3%
Some education
2
9.5%
A lot education
2
9.5%

53
Figure 1
Where SHT Education was Obtained

54
Participants were asked to identify how much time they had spent researching
smart home technology, either at work or at home, within the last five years, using a 5-
point Likert scale (1=none; 5=10+ hours/week). Of the participants that answered (n=65),
15% had completed no research, 59% completed less than 1 hour/week, 20% completed
1-5 hours/week, 2% completed 5-10 hours/week, and 5% completed 10+ hours of
research per week, within the last 5 years.
Similarly, participants were asked to identify how much time they had spent
researching smart home technology, either at work or at home, within the last six months.
The answer selections were based on the same 5-point Likert scale mentioned
previously. Of the participants that answered (n=65), 18% had completed no research,
54% completed less than 1 hour/week, 25% completed 1-5 hours/week, 3% completed 5-
10 hours/week, and zero participants had completed 10+ hours of research per week on
SHT in the last six months. See Table 3 and Figure 2 for visual representation of the data
Table 3
Time Spent Researching SHT
Variable
N
Percentage
Time spent researching SHT in
the last 5 years
None
10
15.4%
Less than 1hr/wk
38
58.5%
1-5hrs/wk
13
20%
6-10hrs/wk
1
1.5%
10+hrs/wk
1
4.6%
Time spent researching SHT in
the last 6 months
None
12
18.5%
Less than 1hr/wk
35
53.8%
1-5hrs/wk
16
24.6%
6-10hrs/wk
2
3.1%
10+hrs/wk
0
0%

55
Figure 2
Hours per Week Spent Researching SHT
Participants were asked whether they incorporate smart home technology into
their practice. Of the responding participants (n=75), 63% reported not using SHT in
practice whereas 37% reported using SHT in practice. See Table 4 and Figure 3 below for
visual representation of the data.
Table 4
Incorporation of SHT into Practice
Variable
N
Percentage
Incorporation of SHT into
practice
No
47
62.7%
Yes
28
37.3%

56
Figure 3
Percentage that Incorporate SHT into Practice
Survey participants who indicated using smart home technology in practice were
asked to rate their comfort with using smart home technology, on a 5-point Likert scale
(1=not at all comfortable using; 5=extremely comfortable using).Of the participants that
answered (n=27), no participants reported feeling not at all comfortable, 7% feel slightly
comfortable, 33% somewhat comfortable, 56% moderately comfortable, and only 4%
feel extremely comfortable with using SHT.
Survey participants who use smart home technology were also asked to rate their
perceived effectiveness in utilizing smart home technology on a 5-point Likert Scale
(1=not at all effective; 5=extremely effective). Of the participants that answered (n=27),
no participants reported feeling not at all effective, 15% feel slightly effective, 33%
somewhat effective, 45% moderately effective and only 7% feel extremely effective
when using SHT. See Table 5 and Figure 4 below for visual representation of the data.

57
Table 5
Comfort and Perceived Effectiveness with Using SHT
Variable
N
Percentage
Comfort
Slightly
2
7.4%
Somewhat
9
33.3%
Moderate
15
55.6%
Extremely
1
3.7%
Effectiveness
Slightly
4
14.8%
Somewhat
9
33.3%
Moderate
12
44.4%
Extremely
2
7.4%
Figure 4
Perceived Effectiveness & Comfort Using SHT
Participants that indicated they use smart home technology in their practice were
asked to identify supports they have encountered with using smart home technology. Of
the participants who responded (n=27), 16 identified co-worker(s), 8 identified family, 7

58
identified professional organizations, 6 identified special interest groups/communities of
practice, 6 identified friends, 4 identified mentor(s), and another 4 identifying “other” as
a source of support for utilizing SHT. The four participants (5%) who listed “other”
supports, identified no supports, suppliers, local building designers, and companies
providing the equipment (reps). See Table 6 and Figure 5 below for visual representation
of the data.
Table 6
Supports for Using SHT
Variable
N
Co-workers
16
Mentor(s)
4
Professional organization
7
Special interest
group/community of practice
6
Friends
6
Family
8
Other
4
Figure 5
Supports for Using SHT

59
Participants were asked to rate their level of personal interest using a 5-point
Likert scale (1=not at all interested; 5=extremely interested), in using smart home
technology. Of the participants that chose to answer the question (n=61), only one
participant (2%) stated being not at all interested, 20% slightly interested, 34% somewhat
interested, 21% moderately interested, 23% extremely interested in using smart home
technology. See Table 7 and Figure 6 below for visual representation of the data.
Table 7
Level of Interest in Using SHT
Variable
N
Percentage
Level of interest in using SHT
Not at all
1
1.6%
Slightly
12
19.7%
Somewhat
21
34.4%
Moderate
13
21.3%
Extremely
14
23%
Figure 6
Interest in SHT

60
Participants were asked to rate their perceived level of knowledge on smart home
technology, using a 5-point Likert scale (1=no knowledge; 5=extreme knowledge). Of the
participants that chose to answer the question (n=61), 12% reported no knowledge, 28%
slight knowledge, 33% some knowledge, 26% moderate knowledge, and only one
individual (2%) reported extreme knowledge on smart home technology. See Table 8 and
Figure 7 below for visual representation of the data.
Table 8
Perceived Knowledge of SHT
Variable
N
Percentage
Knowledge of SHT
No knowledge
7
11.5%
Slight knowledge
17
27.9%
Some knowledge
20
32.8%
Moderate knowledge
16
26.2%
Extreme knowledge
1
1.6%
Figure 7
Perceived Knowledge of SHT

61
Participants were asked whether they have time to implement smart home
technology with clients. Of the participants who answered (n=75), 57% reported not
having time whereas 43% reported having time to implement SHT into practice. In
regards to access, participants were asked if they have access to smart home technology
products and resources. Of the participants who answered (n=61), 36% reported having
access, 36% reported not having access and 28% identified being unsure if they had
access to SHT products and resources. See Table 9 and Figure 8 below for visual
representation of the data.
Table 9
Time and Access to SHT
Variable
N
Percentage
Time to implement SHT with
clients
Yes
32
42.7%
No
43
57.3%
Access to SHT products and
resources
Yes
22
29.3%
No
22
29.3%
Unsure
17
22.7%

62
Figure 8
Availability to Implement SHT
The researchers inquired about availability of funding by asking participants
about employer provided funding for trial use of smart home technology and if they have
access to other funding sources outside of employer support to implement SHT. Of the 61
participants who answered, only 5% identified having employer provided funding
whereas 85% identified not having funding available from their employer to implement
SHT into practice. Interestingly, 10% identified being unsure if their employer provided
funding for implementation of SHT.
Participants were also asked if they have access to other funding sources outside
of employer support, such as grants and insurance to support implementation of smart
home technology. Of the participants who answered (n=60), 20% reported having access
to other funding sources whereas 52% reported not having other funding sources
available to implement SHT into practice. Another 28% identified being unsure if they
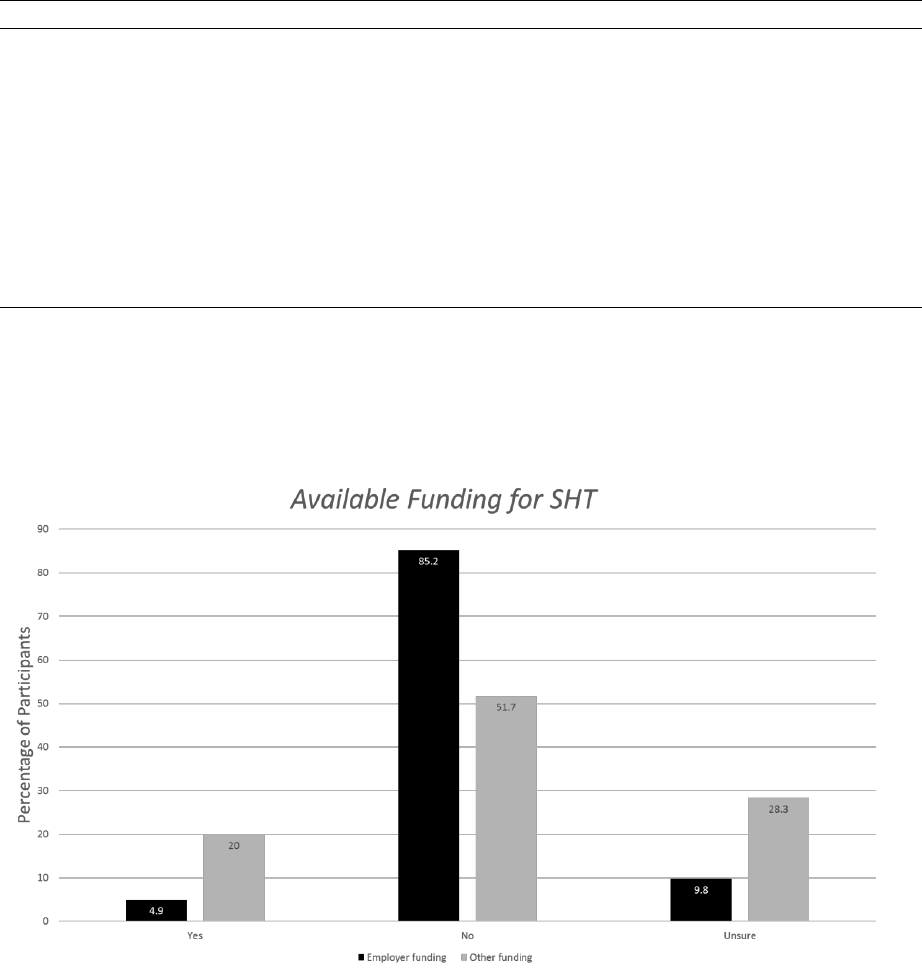
63
have access to other funding sources outside of their current employer for implementation
of SHT. See Table 10 and Figure 9 below for visual representation of the data.
Table 10
Employer Funding for SHT and Access to Other Funding Sources for SHT
Variable
N
Percentage
Employer provides funding for
SHT
Yes
3
4.9%
No
52
85.2%
Unsure
6
9.8%
Access to other funding sources
for SHT
Yes
12
20%
No
31
51.7%
Unsure
17
28.3%
Figure 9
Available Funding for SHT
64
Inferential Statistics
A Spearman correlation coefficient (Spearman rho) was used to determine the
strength of the relationship between the variables. It is a nonparametric procedure, and
can be used in more situations than the Pearson correlation coefficient. The output
consists of a correlation matrix. The three rows represented in each cell contain the
correlation, the significance level, and the N (Cronk, 2017). The Spearman rho ranges
from -1.0 to +1.0. If a correlation is significant at less than the .05 level, a single asterisk
(*) will appear next to the correlation. If it is significant at the .01 level or lower, a double
asterisk (**) will appear next to the correlation. A significant correlation indicates a
reliable relationship, but not necessarily a strong correlation. Coefficients close to 0.0
represent a weak relationship. Coefficients close to 1.0 or -1.0 represent a strong
relationship. Positive correlations indicate that as one variable gets larger, the other
variable gets smaller (Cronk, 2017). Generally, correlations greater than 0.7 are
considered strong, and correlations less than 0.3 are considered weak. Correlations
between 0.3 and 0.7 are considered moderate. For the purpose of the output listed below,
degrees of freedom is N - 2.
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s degree of availability of using smart home technology (time and
access) and degree of support (slight, some, moderate, full) the participants had in
implementing SHT. A moderate positive correlation was found (rho (73) = .607, p =
.000), indicating a significant relationship between the two variables. Participants who
have a higher degree of support for utilizing SHT tend to have more availability for using
SHT in practice. See Table 11 below for visual representation of the data.

65
Table 11
Correlation between Availability and Degree of Support
Correlation Coefficient
.607
Significance (2 tailed)
.000
N
73
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s degree of availability of using smart home technology (time and
access) and the level of interest in utilizing SHT in practice. A moderate positive
correlation was found (rho (59) = .533, p = .000), indicating a significant relationship
between the two variables. Participants who have more availability to SHT tend to be
more interested in learning and utilizing SHT in practice. See Table 12 below for visual
representation of the data.
Table 12
Correlation between Availability and Level of Interest
Correlation Coefficient
.533
Significance (2 tailed)
.000
N
59
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s degree of availability of using smart home technology (time and
access) and whether they currently receive funding (simple yes/no) for utilizing SHT in
practice. A moderate positive correlation was found (rho (73) = .354, p =.001), indicating
a significant relationship between the two variables. Participants who currently receive
funding for implementing SHT into their practice tend to have better availability to SHT.
See Table 13 below for visual representation of the data.

66
Table 13
Correlation between Availability and Funding
Correlation Coefficient
.354
Significance (2 tailed)
.001
N
73
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s degree of support (slight, some, moderate, full) with implementing
smart home technology into practice and level of interest of utilizing SHT in practice. A
moderate positive correlation was found (rho (59) = .550, p = 0.000), indicating a
significant relationship between the two variables. Participants with more interest in SHT
tend to have greater support when utilizing SHT in practice (full support vs. slight). See
Table 14 below for visual representation of the data.
Table 14
Correlation between Degree of Support and Level of Interest
Correlation Coefficient
.550
Significance (2 tailed)
.000
N
59
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s degree of support (slight, some, moderate, full) with implementing
smart home technology into practice and whether they currently receive funding (a
simple yes/no answer) for utilizing SHT in practice. A moderate positive correlation was
found (rho (73) = .614, p = 0.000), indicating a significant relationship between the two
variables. Participants who currently receive funding for implementing SHT into their
practice tend to have greater support when utilizing SHT in practice (full support vs.
slight). See Table 15 below for visual representation of the data.

67
Table 15
Correlation between Degree of Support and Funding
Correlation Coefficient
.614
Significance (2 tailed)
.000
N
73
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s degree of support (slight, some, moderate, full) with implementing
smart home technology into practice and whether they were currently using SHT
(yes/no). A moderate positive correlation was found (rho (73) = .546, p = .000),
indicating a significant relationship between the two variables. Participants who are using
SHT tend to have greater support when utilizing SHT in practice (full support vs. slight).
See Table 16 below for visual representation of the data.
Table 16
Correlation between Degree of Support and Use
Correlation Coefficient
.546
Significance (2 tailed)
.000
N
73
Spearman rho correlation coefficient was calculated for the relationship between
participant’s sources of support (co-workers, mentors, professional organizations, special
interest groups/community of practice, friends, family) and whether they were currently
using SHT (yes/no). A moderate positive correlation was found (rho (73) = .541, p =
.000), indicating a significant relationship between the two variables. Participants who
are using SHT tend to have greater sources of support when utilizing SHT in practice.
See Table 17 below for visual representation of the data.
68
Table 17
Correlation between Sources of Support and Use
Correlation Coefficient
.541
Significance (2 tailed)
.000
N
73
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s amount of education (no education, little education, some
education, a lot of education, and significant education) obtained on SHT through a
variety of means and level of interest in utilizing SHT in practice. A moderate positive
correlation was found (rho (59) = .383, p =.001), indicating a significant relationship
between the two variables. Participants with more education on SHT tend to have greater
interest in incorporating SHT into practice. See Table 18 below for visual representation
of the data.
Table 18
Correlation between Education and Interest
Correlation Coefficient
.383
Significance (2 tailed)
.001
N
59
A Spearman rho correlation coefficient was calculated for the relationship
between participant's level of interest in utilizing SHT in practice and perceived
effectiveness when utilizing SHT. A moderate positive correlation was found (rho (22) =
.368, p < .05), indicating a significant relationship between the two variables. Participants
who have greater levels of interest in incorporating SHT into practice tend to have greater
levels of perceived effectiveness with SHT in practice. See Table 19 below for visual
representation of the data.

69
Table 19
Correlation between Interest and Perceived Effectiveness
Correlation Coefficient
.368
Significance (2 tailed)
.05
N
22
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s level of interest in utilizing SHT in practice and whether they were
currently using SHT (yes/no). A moderate positive correlation was found (rho (59) =
.410, p = .001), indicating a significant relationship between the two variables.
Participants who are currently using SHT tend to have greater levels of interest with
incorporating SHT in their practice. See Table 20 below for visual representation of the
data.
Table 20
Correlation between Interest and Use
Correlation Coefficient
.410
Significance (2 tailed)
.001
N
59
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s perceived level of knowledge on SHT and level of comfort with
utilizing SHT. A moderate positive correlation was found (rho (22) = .556, p = .002),
indicating a significant relationship between the two variables. Participants who have
greater levels of perceived knowledge on SHT tend to have greater levels of comfort with
utilizing SHT in practice. See Table 21 below for visual representation of the data.

70
Table 21
Correlation between Perceived Knowledge and Comfort
Correlation Coefficient
.556
Significance (2 tailed)
.002
N
22
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s perceived level of knowledge on SHT and perceived effectiveness
when utilizing SHT. A moderate positive correlation was found (rho (22) = .516, p =
.005), indicating a significant relationship between the two variables. Participants who
have greater levels of perceived knowledge on SHT tend to have greater perceived
effectiveness when utilizing SHT in practice. See Table 22 below for visual
representation of the data.
Table 22
Correlation between Perceived Knowledge and Perceived Effectiveness
Correlation Coefficient
.516
Significance (2 tailed)
.005
N
22
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s level of perceived knowledge on SHT and whether they were
currently using SHT (yes/no). A moderate positive correlation was found (rho (59) =
.487, p = .000), indicating a significant relationship between the two variables.
Participants who are currently using SHT tend to have greater levels of perceived
knowledge with incorporating SHT in their practice. See Table 23 below for visual
representation of the data.

71
Table 23
Correlation between Perceived Knowledge and Use
Correlation Coefficient
.487
Significance (2 tailed)
.000
N
59
A Spearman rho correlation coefficient was calculated for the relationship
between participant’s level of comfort with utilizing SHT in practice and perceived
effectiveness when utilizing SHT. A strong positive correlation was found (rho (25) =
.854, p = .000), indicating a significant relationship between the two variables.
Participants who report higher comfort with utilizing SHT tend to perceive greater
effectiveness when utilizing SHT in practice. See Table 24 below for visual
representation of the data.
Table 24
Correlation between Comfort and Perceived Effectiveness
Correlation Coefficient
.854
Significance (2 tailed)
.000
N
25
A Spearman rho correlation coefficient was calculated for the relationship
between currently receiving funding (yes/no) for utilizing SHT in practice and whether
they were currently using SHT. A strong positive correlation was found (rho (73) = .720
p = .000), indicating a significant relationship between the two variables. Participants
who are currently using SHT tend to currently have funding in place for incorporating
SHT in their practice. See Table 25 below for visual representation of the data.

72
Table 25
Correlation between Funding and Use
Correlation Coefficient
.720
Significance (2 tailed)
.000
N
73
73
CHAPTER V
DISCUSSION
Purpose
The purpose of this study was to inquire about the use of smart home technologies
(SHT) by occupational therapy practitioners (OTPs) in practice. Additionally, the
researchers were interested in what facilitators and barriers may impact the use of SHT as
an intervention. The researchers developed one overarching research question, along with
two additional sub-questions that will further be presented in this chapter as “the first
sub-question” and “the second sub-question”. They are as follows: What is the utility of
smart home technology within occupational therapy practice?
• What relationships exist (if any) between factors identified and reported with use
of SHT?
• What relationships exist (if any) between factors identified and reported with
perceived effectiveness with SHT?
Summary
Participants of this study primarily practiced occupational therapy in the areas of
productive aging (24%) and rehabilitation and disability (62.7%). The majority of
participants served the older adult population (62.7%) by working in settings such as
home health care and skilled nursing facilities. The literature also supports the notion that
OTPs are likely to use SHT with the older adult population (Giger & Markward, 2011) in
home health, long term care, and assisted living settings (Burrows et al, 2018;
74
McKeough, 2019; Orlov, 2019). This is likely due to the fact that many older adults are
interested in aging in place and there are many opportunities to use SHT in the
aforementioned areas of practice.
The researchers were interested in gathering data about where OTPs obtained
education on SHT as an occupational therapy intervention. Education and continuing
education are hallmarks and necessities of the practice of the occupational therapy
profession. There is an ethical obligation for OTPs to have education on technology, and
therefore SHT (AOTA, 2015). Participants of this study reported receiving the greatest
amount of education on SHT through independent research and by attending general
conferences. Perhaps the most important data point regarding SHT education was that the
majority of participants did not receive any education in SHT while in OT school. That
being said, the researchers did not find any literature identifying where OTPs were
receiving education and training on the topic of SHT.
The first sub-question the researchers looked to answer was the overall use of
SHT in occupational therapy practice. Approximately one-third (37.3%) of the
participants of this study indicated that they are utilizing SHT in their practice, leaving
62.7% that were not using SHT. There was no literature found by the researchers that
determined the overall use of SHT by practitioner. In addition to overall use, the
researchers were interested in what factors may have influenced occupational therapy
practitioners to use or not use SHT. This leads to the second research question which
focused on exploring factors that were identified influencing the use of SHT. The data
highlighted four factors that were found to have a correlation with the use of SHT in
practice, which included support, interest, knowledge, and funding. A relationship was
75
found between the utilization of SHT in practice and the sources of support (co-workers,
friends, and family) as well as the degree (slight, some, moderate, full) of support that the
participant received in regards to SHT. The literature also shows that sources of support
may influence the use of technology in practice, specifically support from within the
workplace (AOTA, 2019a; Proffitt et al., 2019). A correlation was also found between
interest and use, suggesting that the more interested a practitioner was in SHT, the more
likely they were to use it as an intervention. This finding was also supported by the
literature (Verdonck et al., 2011). The researchers found a relationship between use of
SHT and the amount of perceived knowledge a practitioner had about SHT. This
indicates the higher a practitioner perceived their knowledge to be, the more likely they
were to use SHT. Interestingly, one finding from the literature found that although 84%
of practitioners believed they could use SHT effectively in practice due to their
knowledge base, only 34% were actually able to use SHT while using their own
knowledge base (Verdonck et al., 2011). This point raises the question of what is the
relationship between perceived knowledge, use, and effectiveness. The last factor found
to correlate with use of SHT was funding, indicating a relationship between these two
variables. Interestingly, funding was found to be the most commonly cited barrier to
using technology as an intervention, by both clients and OTPs (Dicianno et al., 2019;
Hamblin, 2017).
The second sub-question investigated the factors influencing the perceived
effectiveness of occupational therapy practitioners when implementing SHT in practice.
The researchers found that three factors were shown to relate to practitioners' perceived
effectiveness. The three factors include knowledge, interest, and comfort. Over half of
76
the participants responded that they have at least some knowledge about SHT and the
relationship with the variable of effectiveness suggests that individuals need to have some
knowledge about SHT in order to feel effective when using it as an intervention. In
addition, a common barrier, found in the literature, for the nonuse of technologies of
interventions was the lack of knowledge. This includes limited knowledge of charging
policies when using technology (Hamblin, 2017) and the jargon that is used amongst
technological products (Proffitt et al., 2019). In relation to interest in SHT, the data
suggests that practitioners that have more interest in SHT perceive that they are more
effective when using it as an intervention than those who have less interest in the topic.
Lastly, the data suggests that individuals that are more comfortable with these
technologies are also more likely to perceive that they are effective with using SHT in
practice. Though the researchers found relationships between perceived effectiveness and
comfort, perceived effectiveness and interest, there was no literature found at the time of
the study that corroborated these relationships.
Throughout the data analysis process, the researchers found several other
correlations and relationships of note with the variables of availability, support,
education, and knowledge. A correlation with the variable of availability was established
with the factors of interest, support and funding. These relationships suggest that the
more interest, support, and funding a practitioner has in and for SHT the more likely that
they will have it available for them to use in practice. Correlations with the variables of
access and funding were also established in the literature. The literature suggests that
access to high technology is a barrier to using it in practice (Hoogerwerf et al., 2002). In
addition, the literature suggests that a common obstacle that practitioners experience
77
when attempting to use technology in practice are the intensive process of obtaining
insurance approval for device, cost of device, availability of funding, and time it takes to
obtain authorization and equipment (Dicianno et al., 2019), thus limiting the availability
of SHT.
Correlations were also found between the variable of support with funding and
interest. This suggests that the more support an individual experiences, the more likely
they will also have funding to use SHT and they may have more interest to use it as an
intervention. That being said, no literature was found by the researchers on the
relationships between the aforementioned variables. In addition to the aforementioned
relationships, education was also found to correlate with the variable of interest. This
suggests that the more interest a practitioner has regarding SHT, the more education the
practitioner has received about the topic. The literature also suggests a relationship
between these two factors. Jiancaro et al. (2017) indicated that participants were drawn to
use technology in practice and were interested in obtaining additional education in
technology and were able to identify that they valued learning more about technology and
using technology in practice. Lastly, the researchers established a correlation between the
variables of knowledge and comfort. This suggests that the more knowledge a
practitioner has about SHT the more comfortable they will be to use it as an intervention
within their practice. This relationship was also detected in the literature but was
interpreted to be a barrier. Specifically, practitioner’s lack of knowledge on some aspects
of using technology was a distinct barrier for practitioners to be comfortable when using
technology with their clients (Hamblin, 2017).
78
Implications
As stated previously, only 37% of the participants in this study actually used SHT
in their practice. The researchers assert that there are key factors that are either assisting
practitioners in their use of SHT or hindering their use and access of it. First supports for
SHT will be identified and then barriers of utilizing SHT will be discussed. The biggest
support to using SHT indicated by participants was their co-workers. In addition, the
higher degree of support an OTP has to use SHT the more likely they are to be using it in
practice as well. This information suggests that if an OTP has support from their
colleagues and leaders in the workplace to use this technology they will be more likely to
use it as an intervention with their clients. Moreover, the community and workplace are
areas of opportunity to share more about SHT which ties into the workplace culture. This
shows a need for support and access to SHT and it calls for leaders in the workplace to
provide support and resources to their colleagues. A way for people to gather ideas and
resources about SHT is to start a community of practice focused on the topic. Using
social media is a strong outlet for communities of practice. With the recent increase in
social media use, communities of practice on these platforms will likely grow in the
future.
Another support that has been identified is the practitioner’s interest in SHT.
Interest in the topic is linked to increased support, increased access to funding, and
increased availability. That being said, it was found that interest in the topic did not
necessarily mean that a practitioner perceived they were effective when using it as an
intervention, therefore an OTP’s interest in SHT is not a driving force for it to be an
effective intervention. It was found that comfort with SHT was a driving force for
79
practitioners to perceive they were effective when using it as an intervention. Though the
topic of SHT is vast and may be overwhelming to a practitioner, practitioners should take
interest in it because of the boundless opportunities it has to assist clients in their
achievement of independent and meaningful lives and there is an ethical obligation for
practitioners to use and investigate updated technologies and information in practice.
Smart home technology should be used in care and when a practitioner takes a moment to
develop interest in the topic, and hence develops a better understanding and knowledge
base, they will likely have an increase in comfort and therefore, perceived effectiveness
when using technologies as interventions. All of these factors assist clients in the long
run. In summary, the biggest supports for using SHT participants indicated included co-
workers and workplace culture, interest in SHT, and comfort with using SHT.
There were three barriers that were most often cited by participants which
included availability, funding, and education. The majority of participants indicated that
they did not have availability to access SHT, more specifically, they did not have time or
access to these technologies. This suggests that OTPs may not have immediate resources
to utilize in regards to SHT. This may be linked to ease of access to information, lack of
information, or lack of time to inquire about SHT. This information suggests that more
informative resources need to be developed by the occupational therapy profession,
whether in research articles, conferences, or a simple OT Practice article. This is no
different than other types of assistive technology interventions that may have had a lack
of availability early on. There are certain factors that can be addressed to change
availability from a barrier to a support to using SHT in practice including access to
information, increased funding and insurance coverage, a commitment by practitioners to
80
spend their time resources, and a pledge by administrative and workplace leaders to take
action on increasing SHT availability both for their colleagues and clients.
Funding was a barrier that was strongly represented in the literature and was also
strongly represented in the data in this study. The obstacle of funding has two
components to it. One, there is not funding available to the practitioner to use it through
their workplace. This means that a practitioner may not have the opportunity to work
directly with the devices before using them in intervention. This may affect an OTPs
decision to use SHT as an intervention because the practitioner may not have any other
experiences they can fall back on when it comes to SHT devices. The second part of the
funding obstacle relates to the clients. Over half of participants indicated that there were
no funding sources outside of their workplace for SHT. This suggests that there SHT is
not currently being covered under insurance, both private and public, and there also may
be a lack of grant funding available. The lack of these funding sources has implications
for the client because even if SHT would be a good intervention and assistive device for
the client, the client may not be able to afford the necessary devices out of pocket. This
too may be an implication for the lack of use of SHT as an intervention. Practitioners
should take time to advocate for increased funding for SHT in their workplace and from
insurance companies, just like they would with other AT, such as wheelchairs. In the very
least, managers and administrative leaders should take the time to investigate funding
sources that may be available, such as grants and private donations. In addition, AOTA
should advocate for the role of SHT in practice and therefore should advocate for the
reimbursement of SHT interventions by CMS. If CMS were to provide coverage for SHT
81
it is likely that private insurance companies would do so as well. These changes have the
potential to increase the quality of life for many clients.
Occupational therapy practitioners have an ethical obligation to stay up to date
with technologies, and in order to do this education and training is needed. Therefore,
perhaps the most important data point regarding SHT education is that 82% of
participants received little to no education about SHT while they were in occupational
therapy school. Occupational therapy programs need to provide more education on the
use of SHT in order to stay in tune with the times and meet their ethical obligations. The
lack of education of SHT also likely contributes to the overall nonuse of SHT as an
intervention. Occupational therapy students that are currently in school now and those
that will be entering school in the future have likely all grown up with using technology.
Therefore, they have an increased level of technological literacy than perhaps those who
are already established in practice. Consequently, ACOTE could easily update standards
to include SHT as a skill required for entry level practice. This would mandate programs
to include these updated technologies in their curriculums. SHT is here now and will only
continue to increase in use in the future. Including it in curriculums is no different than
including other assistive technologies. Not only do schools and ACOTE have a call to
include this topic, they have a moral and ethical responsibility to do so. The fact that this
is not being incorporated in professional programs is reprehensible.
Limitations
Limitations of this study include the survey design, confusing or misleading
structure of survey question wording, errors in initial grouping of data and difficulties
82
with correlation data, unidentified correlations in relation to other factors (e.g. education)
in the research, and finally missing survey responses.
When considering survey design, the researchers of the study took careful
consideration in creating the survey before distributing it via the social media pages.
However, after completing the data analysis and writing up the results and implications,
the researchers found that there was little variety in question type, resulting in more
simple yes/no question answers with little room for clarification. The survey did contain
some open-ended questions, allowing the participant to answer the “other” option and
explain if the answer options for said questions were not appropriate. However, the
researchers chose not to analyze this information or include many of the responses, as
there were very few that chose to answer “other” and explain when appropriate. When
considering the survey design after data collection, the researchers believe the question
order could have been reworked and reorganized in a more fluid fashion. After asking
more descriptive questions in nature, there was a question regarding smart home
technology use along with a definition and examples. This definition and examples were
examined through the lenses of the two occupational therapy students, and the student
researcher’s advisor, an occupational therapy professor and PhD holder. All individuals
believed this definition to be understandable; however, the researchers believe the
definition and example could have been written differently in order for better
understanding and an increased likelihood that participants would answer the remainder
of the questions in relation to the definition. The researchers believe that this definition
was either skipped entirely or misunderstood in relation to how some participants
answered questions throughout the survey, thus leading to possible skewed data.
83
Another limitation evident throughout the research was errors in initial data
groupings. The student researchers do not claim to be experts in data analysis and
knowing appropriate tests to run while using SPSS in relation to a variety of survey
questions and the data collected. After completing initial data analysis and moving
forward in writing results, the student researchers found skewed data in relation to poor
data groupings, and finding minimal and incorrect correlations between variables. This
led the student researchers to start the data analysis process over and regroup the data into
new groupings, along with the assistance of a research consultant, who assisted greatly in
grouping our variables and providing guidance while using SPSS. This provided for
greater understanding and presentation of the data moving forward, especially when
analyzing and presenting relationships in the data.
When considering the survey design and multiple reassessments of the data, the
researchers found a limitation with limited correlation relationships in regards to the
variables being studied. There were many correlations that showed importance in regards
to support, interest, knowledge, and funding, as well as other factors such as use.
However, the researchers were also examining the relationship between education and
availability in relation to the variables listed above. Through the data, there was little to
support use with education and availability, which was of particular interest of the
student researchers. This could have been due to the survey design, uncertainty of the
student researchers when grouping variables, and possible skewed data due to the
limitations stated above. Another possible limitation is the moderate frequency of
missing survey responses, which created difficulties when analyzing the data and finding
relationships between variables.
84
Recommendations
The researchers have identified several recommendations for the future study of
smart home technology devices within occupational therapy practice. Additional studies
should be completed to evaluate trends in devices and overall use of SHT. This is
especially important now as the world, and occupational therapy practice, has been
affected by the Corona Virus pandemic and the use of technology, both to engage in
practice and as an intervention, has likely increased significantly given the circumstances.
Furthermore, repeating this study in the future would be beneficial to identify changes in
knowledge, attitudes, current practices, perceived barriers and supports, years of
experience and active involvement by practitioners in future years with SHT. The
aforementioned studies would be beneficial for the profession to know what SHT is being
used by professionals and how successful the use of technology was for their clients. In
addition, it is our recommendation that more education be available to current and future
occupational therapy practitioners. This can be done by occupational therapy programs,
including more information about updated technologies in their curriculum as well as
including the topic of smart home technology in specialty and general conferences.
Conclusion
Occupational therapists have an ethical and moral obligation to use the best
available interventions for their clients to assist their clients in leading more independent
and meaningful lives. It has been shown throughout this paper that SHT has the potential
to be the intervention that allows individuals to lead more independent and meaningful
lives. Therefore, OTPs should, in theory, be using these devices in their practice. Sadly,
the data from this study point to the fact that the majority of practitioners are not using it
85
as an intervention even though they are working in areas and populations, such as
productive aging, rehabilitation, home health and the older adult population, that would
see the most benefit from the utilization of these devices.
The most substantial barriers to using SHT that were identified include lack of
funding sources, lack of education, and lack of availability to the devices. These factors
do not need to remain barriers and in fact can and should become supports to using SHT.
Though the data from this study and literature support the use of SHT as an intervention
for older adults in particular, it has the potential to assist individuals in other settings as
well. For example, individuals with intellectual and developmental disabilities, and
individuals who may have physical disabilities such as a spinal cord injury.
Occupational therapy practitioners are creative in nature and should use the tool
of SHT creatively as well to assist their clients in obtaining independence and increased
quality of life. Smart home technology has boundless potential in the hands of
occupational therapy practitioners. Practitioners should not let the opportunity to use
these tools pass as other professions certainly will not. “Occupational therapists cannot be
leaders in this new era unless we set aside our fears and embrace the potential benefits of
technologies” (Liu, 2018, p. 281).

86
REFERENCES
American Family Insurance. (2019). 6 benefits of smart home technology.
https://www.amfam.com/resources/articles/at-home/six-benefits-of-smart-home-
technology
American Occupational Therapy Association. (2015). Occupational therapy code of
ethics (2015). American Journal of Occupational Therapy, 69(Suppl. 3),
6913410030. http://dx.doi.org/10.5014/ajot.2015.696S03
American Occupational Therapy Association. (2018). 2018 Accreditation Council for
Occupational Therapy Education (ACOTE®) standards and interpretive Guide.
American Journal of Occupational Therapy, 72(2, Suppl.), S1–S83. doi:
10.5014/ajot.2018.72S217
American Occupational Therapy Association. (2019a). Telehealth resources.
https://www.aota.org/Practice/Manage/telehealth.aspx
American Occupational Therapy Association. (2019b). AOTA CommunOT.
https://communot.aota.org/home
Apple Inc. (2019). Home accessories. Retrieved from
https://www.apple.com/ios/home/accessories/
Assistive Technology Industry Association. (2019). AT resource funding guide.
https://www.atia.org/at-resources/what-is-at/resources-funding-guide/
Berridge, C. (2018). Medicaid becomes the first third-party payer to cover passive remote
monitoring for home care: Policy analysis. Journal of Medical Internet Research,
20(2), 19. https://doi-org.ezproxylr.med.und.edu/10.2196/jmir.9650
Blessing, J. D. (2016). Survey Research. In J. G. Forister & J. D. Blessing

87
(Eds.), Introduction to research and medical literature for health
professionals (pp. 79-96). Burlington, MA: Jones & Barlett
Learning, LLC.
Bork, C. E., Jarski, R. W., & Forister, J. G. (2016). Methodology. In J. G. Forister & J. D.
Blessing (Eds.), Introduction to research and medical literature for health
professionals (pp. 61-78). Burlington, MA: Jones & Barlett Learning, LLC.
Burrows, A., Coyle, D., & Gooberman-Hill, R. (2018). Privacy, boundaries and smart
homes for health: An ethnographic study. Health & Place, 112–118. https://doi-
org.ezproxylr.med.und.edu/10.1016/j.healthplace.2018.01.006
Choi, B.C., & Pak, A.W. (2005). A catalog of biases in questionnaires.
Preventing Chronic Disease, 2, 51-63.
https://www.cdc.gov/pcd/issues/2005/jan/04_0050.htm
Chung, J., Demiris, G., & Thompson, H. J. (2016). Ethical considerations regarding the
use of smart home technologies for older adults. Annual Review of Nursing
Research, 34(1), 155–181. https://doi-org.ezproxylr.med.und.edu/10.1891/0739-
6686.34.155
Cook, A.M. & Hussey, S. (1995). Assistive technologies: Principles and practices. St.
Louis, Missouri: Mosby.
Cook, A. M. & Polgar, J. M. (2014). Assistive technologies: Principles & practices (forth
edition). St. Louis, Missouri: Elsevier Mosby.
Cronk, B. (2017). How to use SPSS: A step-by-step guide to analysis and
interpretation. New York, NY: Routledge: A Taylor & Francis
Group.

88
Davenport, R. D., Mann, W., & Lutz, B. (2012). How older adults make decisions
regarding smart technology: An ethnographic approach. Assistive Technology, 24,
168-181.
Demiris, G., Rantz, M. J., Aud, M. A., Marek, K. D., Tyrer, H. W., Skubic, M., … &
Hussam, A. (2004). Older adults’ attitudes towards and perceptions of ‘smart
home’ technologies: A pilot study. Medical Informatics & The Internet in
Medicine, 29(2), 87-94.
Dermody, G., & Fritz, R. (2019). A conceptual framework for clinicians working with
artificial intelligence and health-assistive smart homes. Nursing Inquiry, 26(1),
N.PAG. http://doi-org.ezproxylr.med.und.edu/10.1111/nin.12267
Dicianno, B. E., Joseph, J., Eckstein, S., Zigler, C. K., Quinby, E. J., Schmeler, M. R., …
Cooper, R. A. (2019). The future of the provision process for mobility assistive
technology: A survey of providers. Disability and Rehabilitation: Assistive
Technology, 14(4), 338-345. Doi: 10.1080/17483107.2018.1448470
Giger, J. T., & Markward, M. (2011). The need to know caregiver perspectives toward
using smart home technology. Journal of Social Work in Disability &
Rehabilitation, 10(2), 96–114. DOI: 10.1080/1536710X.2011.571529
Golia, N. (2019). 14 top home insurance companies' smart-tech initiatives.
https://www.dig-in.com/list/15-top-home-insurance-companies-smart-home-
initiatives
Hamblin, K. (2017). Telecare, obtrusiveness, acceptance, and use: An empirical
exploration. British Journal of Occupational Therapy, 80(2), 132-138. Doi:
10.1177/0308022616667751

89
Hayden, C. (2019). The role of Alexa in clinical practice.
https://www.theothub.com/post/the-role-of-alexa-in-clinical-practice
Haymes, L. K., Storey, K., Maldonado, A., Post, M., & Montgomery, J. (2015). Using
applied behavior analysis and smart technology for meeting the health needs of
individuals with intellectual disabilities. Developmental Neurorehabilitation,
18(6), 407–419. https://doi-
org.ezproxylr.med.und.edu/10.3109/17518423.2013.850750
Hoogerwerf, E. J., Lysley, A., Clarke, M. (2002). BRIDGE: Assistive technology against
social exclusion.
http://www.ausilioteca.org/bridge/docs/condens/condrep_eng.pdf
Jiancaro, T., Jaglal, S. B., & Mihailidis, A. (2017). Technology, design and dementia: An
exploratory survey of developers. Disability and Rehabilitation: Assistive
Technology, 12(6), 573-584. Doi: org/10.1080/17483107.2016.1187671
Kozak, B. (2018). Smart home technology claims the insurance industry.
https://ihsmarkit.com/research-analysis/smart-home-technology-claims-the-
insurance-industry.html
Kumar, S., Nilsen, W. J., Abernethy, A., Atienza, A., Patrick, K., Pavel, M., . . .
Swendeman, D. (2013). Mobile health technology evaluation: The mHealth
evidence workshop. American Journal of Preventive Medicine, 45, 228 –236.
http://dx.doi.org/10.1016/j.amepre.2013.03.017
Liu, L., Cruz, A. M., Rincon, A. R., Buttar, V., Ranson, Q., & Goertzen, D. (2015). What
factors determine therapists’ acceptance of new technologies for rehabilitation – a
study using the Unified Theory of Acceptance and Use of Technology (UTAUT).

90
Disability and Rehabilitation, 37(5), 447-455. doi:
10.3109/09638288.2014.923529
Liu, L. (2018). Occupational therapy in the fourth industrial revolution. Canadian
Journal of Occupational Therapy, 85(4), 272-285. Doi:
10.1177/0008417418815179.
Medicare. (2019). Durable medical equipment coverage.
https://www.medicare.gov/coverage/durable-medical-equipment-dme-coverage
McKeough, T. (2019). The easy way to create a smart home. The New York Times.
https://www.nytimes.com/2019/04/02/realestate/the-easy-way-to-create-a-smart-
home.html
Ochalla, B. (2018). Smart-home technology and homeowners insurance.
https://quotewizard.com/home-insurance/smart-home-technology-homeowners-
insurance
Orlov, L. (2019). Six new technologies for older adults [Blog post].
https://www.ageinplacetech.com/blog/six-new-technologies-older-adults-july-
2019
Porteny, L.G., & Watkins, M.P. (2015). Foundations of clinical research: Applications to
practice (3rd ed.). Philadelphia, PA: F.A. Davis Company
Proffitt, R., Schwartz, J. K., Foreman, M., & Smith, R. O. (2019). The Issue Is —Role of
occupational therapy practitioners in mass market technology research and
development. American Journal of Occupational Therapy, 73, 7301347010.
https://doi.org/10.5014/ajot.2019.028167
Smart Home. (2019). Solution center. https://www.smarthome.com/sc-solution-center

91
Taylor, R., & Kielhofner, G. (2017). Collecting quantitative data. In R.
Taylor (Ed.), Kielhofner’s research in occupational therapy:
Methods of inquiry for enhancing practice (pp. 296-312).
Philadelphia, PA: F.A. Davis Company.
Venkatesh, V., Thong, J., & Xu, X. (2012). Consumer acceptance and use of information
technology. Extending the unified theory of acceptance and use of technology.
MIS Quarterly, 36(1), 157-178. http://www.jstor.org/stable/41410412
Verdonck, M. C., McCormack, C., & Chard, G. (2011). Irish occupational therapists’
views of electronic assistive technology. British Journal of Occupational
Therapy, 74(4), 185-190. doi: 10.4276/030802211X13021048723291
Waite, A. (2015). Using the OT brain to implement smart home technology. OT Practice,
20(16), 8-11.
WytCote Technologies. (2019). SeniorSense™. https://seniorsense.wytcotetech.com/
92
APPENDIX A
QUALTRICS SURVEY TOOL

93
What is your identified gender?
Male Female Prefer not to answer
Select the age range you fall within.
20-30 31-40
41-50
51-60
61+
Prefer not to answer
How many years have you been a registered and licensed OT or OTA?
1-4 yrs. 5-10 yrs. 11-15 yrs.
16-20 yrs.
21-25 yrs.
26+ yrs.
Where do you currently practice?
United States of America
Internationally; please specify country
What best describes your geographical area of practice?
Rural
Metropolitan
What is your title?
OT OTA
What is your highest educational degree earned?
Bachelors
Masters
Research Doctorate (Ph.D/Ed.D)
Clinical Doctorate (OTD)
What populations do you serve? (Select all that apply)
Pediatrics
Adolescents
Adults
Older Adults

94
What areas best describe your practice focus, based on AOTA's practice areas (Select all that apply)
Children/Youth
Health & Wellness
Mental Health
Productive Aging
Rehabilitation & Disability
Work & Industry
Are you a certified Assistive Technology Practitioner (ATP)?
Yes
No
Smart Home Technology
Definition of smart home technology:
A smart home is an environment that adopts information and communications technology to collect and share
information, analyze and monitor residents’ behavioral patterns, and, finally, improve residents’ quality of life within the
home. Smart home technologies are also able to link individuals to services and systems outside of the home (Brandt,
Samuelsson, Toytari, & Salminen, 2011; Courtney, 2008). Some examples of smart home technology include, an in
home monitoring system, an artificial intelligence device that controls aspects of the home such as lighting and
temperature, sensors placed throughout the home that alert if the resident has fallen or left the oven on.
Identify amount of education you have gained about smart home technology through the following means.
In the last 5 years, how much time have you spent researching smart home technology, either at work or at home?
None
Less than 1 hr/wk
1-5 hrs/wk
6-10 hrs/wk
10+ hrs/wk
In the last 6 months, how much time have you spent researching smart home technology, either at work or at home?
None
Less than 1 hr/wk
1-5 hrs/wk
6-10 hrs/wk
10+ hrs/wk

95
Do you incorporate smart home technology into your practice?
Yes
No
How often do you use smart home technology in your OT practice?
Never Seldom Occasionally Almost always Always
How many years have you been utilizing smart home technology in your OT practice?
0-5 yrs.
6-10 yrs.
11-15 yrs.
16-20 yrs.
21+ yrs.
Rate your comfort with using smart home technology.
1 = not at all 2 = slightly
3 = somewhat
4 = moderately
5 = extremely
Rate your effectiveness in utilizing smart home technology.
1 = not at all 2 = slightly
3 = somewhat
4 = moderately
5 = extremely
What sources of funding have you utilized to access smart home technology for clients. (Check
all that apply)
Private pay
Grant funding
Private donation
Private medical insurance
Government funded medical insurance (Medicare, Tricare, state supported)
Identify supports you have encountered regarding the use of smart home technology. (Check
all that apply)
Personal Interest
Rate the level of your personal interest in using smart home technology.
Not at all interested Slightly interested Somewhat interested
Moderately interested
Extremely interested

96
4/22/2020 Qualtrics Survey Software
Please state why you are not interested in smart home technology
(Ex. Do not see how it is applicable to practice)
Rate your interest in researching more about smart home technology use.
Not at all Slightly Somewhat Moderately Extremely
Rate your knowledge on smart home technology.
No knowledge Slight knowledge Some knowledge Moderate knowledge Extreme knowledge
Do you feel that you have time to implement smart home technology with clients?
Yes
No
Do you have access to smart home technology products and resources?
Yes
No
Unsure
Does your current employer provide funding for trial use of smart home technologies with clients?
Yes
No
Unsure
Do you have access to other funding sources (outside of employer support) for implementing smart home technology (ie. grants,
insurance)?
Yes
No
Unsure
Rate the level of support within your place of work in utilizing smart home technology.
No support Slight support Some support Moderate support Full support
97
APPENDIX B
IRB APPROVAL

98
UND IRB approval letter
Bowles, Michelle
Fri 7/26/2019 3:53 PM
To: Zimmer, Jessie; Walthers, Kylie; Cc: Graves, Cherie
Institutional Review Board
Tech Accelerator, Suite 2050
4201 James Ray Drive Stop 7134
Grand Forks, ND 58202-7134
Phone: 701.777.4279
Fax: 701.777.2193
July 26, 2019
Principal Investigator(s):
Kylie Walthers and Jessie Zimmer
Project Title:
The Utility of Smart Home Technology Within Occupational Therapy
Practice
IRB Project Number:
IRB-201907-013
Project Review Level:
Exempt 2
Date of IRB Approval:
07/26/2019
Expiration Date of This
Approval:
07/25/2022
The application form and all included documentation for the above-referenced project have been reviewed and approved via the procedures of the
University of North Dakota Institutional Review Board.
If you need to make changes to your research, you must submit a Protocol Change Request Form to the IRB for approval. No changes to
approved research may take place without prior IRB approval.
This project has been approved for 3 years, as permitted by UND IRB policies for exempt research. You have approval for this project through the
above-listed expiration date. When this research is completed, please submit a Termination Form to the IRB.
The forms to assist you in filing your project termination, adverse event/unanticipated problem, protocol change, etc. may be accessed on the IRB
website: http://und.edu/research/resources/human-subjects/
Sincerely,
Michelle L. Bowles, M.P.A., CIP
IRB Manager
Cc: Cherie Graves, MOT, OTR/L
Michelle L. Bowles, M.P.A., CIP
Manager, Ins tu onal Review Board
University of North Dakota
Tech Accelerator, Suite 2050
4201 James Ray Drive Stop 7134
Grand Forks, ND 58202-7134
P: 701.777.4279
F: 701.777.2193
Michelle[email protected]
[UND.edu/research/resources/human-subjects/]UND.edu/research/resources/human-subjects/
99
APPENDIX C
STATEMENT OF INFORMED CONSENT
100
The University of North Dakota
Consent to Participate in Research
Project Title: The Utility of Smart Home Technology Within Occupational Therapy
Practice
Principal Investigators:
Kylie Walthers; Jessie Zimmer
Email Address:
[email protected]; jessie.n.zimme[email protected]
Department: Occupational Therapy
Research Advisor: Cherie Graves
Research Advisor
Phone/Email Address:
701-777-6086
cherie.graves@und.edu
Purpose of the Study:
The purpose of this study is to explore occupational therapists utility of smart home
technology in their practice. Additionally, the student researchers will inquire into the
facilitators and barriers of utilization of smart home technology within the practice of
occupational therapy.
Procedures to be followed:
You are being asked to complete an online survey.
Risks:
There are no risks in participating in this research beyond those experienced in everyday
life.
Benefits:
The results of this study will better inform occupational therapy practitioners of the use of
smart home technology and the barriers and facilitators experienced when smart home
technology is implemented by occupational therapy practitioners. Results may impact
101
the use of smart home technology by occupational therapists within the profession that
are currently practicing in many different settings.
Duration:
It will take approximately 15 minutes to complete the survey.
Statement of Confidentiality:
No identifying information will be collected on this survey. All data will be stored and
analyzed in a private setting, and only the researchers and our advisors will have access
to the data. You should complete the survey in a private location to ensure confidentiality
while you are completing the survey. If this research is published, you will not be
identified as your name is not collected and cannot be linked to your responses in any
way.
All survey responses that we receive will be treated confidentially and stored on a secure
server. However, given that the surveys can be completed from any computer (e.g.,
personal, work, school), we are unable to guarantee the security of the computer on
which you choose to enter your responses. As a participant in our study, we want you to
be aware that certain "key logging" software programs exist that can be used to track or
capture data that you enter and/or websites that you visit.
Right to Ask Questions:
The researchers conducting this study are Kylie Walthers and Jessie Zimmer. If you
have questions, concerns, or complaints about the research please contact Cherie
Graves, with any questions at (701) 777-6086.
If you have questions regarding your rights as a research subject, you may contact The
University of North Dakota Institutional Review Board at (701) 777-4279 or
UND.irb@UND.edu. You may contact the UND IRB with problems, complaints, or
concerns about the research. Please contact the UND IRB if you cannot reach research
staff, or you wish to talk with someone who is an informed individual who is independent
of the research team.
General information about being a research subject can be found on the Institutional
Review Board website “Information for Research Participants”
http://und.edu/research/resources/human-subjects/research-participants.html
Compensation:
You will not receive compensation for participation.
Voluntary Participation:
You do not have to participate in this research. You can stop your participation at any
time. You may refuse to participate or choose to discontinue participation at any time
102
without losing any benefits to which you are otherwise entitled.
You do not have to answer any questions you do not want to answer.
You must be 18 years of age older to participate in this research study.
Completion of the survey implies that you have read the information in this form and
consent to participate in the research.
Please keep this form for your records or future reference.
