
April 2023
ISSUE BRIEF
1
HP-2023-09
Updated National Survey Trends in Telehealth
Utilization and Modality (2021-2022)
Telehealth utilization rapidly expanded during the onset of the COVID-19 pandemic
and continues to provide critical access to health care services. Updated trends show
a steady use of telehealth with a slightly higher proportion of video-based versus
audio-only services by March 2022; however, disparities persist in populations and
across insurance types.
Euny C. Lee, Violanda Grigorescu, Idia Enogieru, Scott R. Smith, Lok Wong Samson, Ann B. Conmy,
and Nancy De Lew
KEY POINTS
• Telehealth utilization has changed since the steep increase from the early stages of the COVID-19
pandemic. This report updates prior findings on national trends of telehealth use through an analysis
using the Census Bureau’s Household Pulse Survey data from April 2021 through August 2022.
Understanding patterns and factors associated with telehealth use are important to inform policy
decisions.
1-4
• Compared to earlier periods in the pandemic, telehealth utilization was lower during the study
period (April 14, 2021 through August 8, 2022), but continued to remain above pre-pandemic
levels.
5
• Telehealth use rates varied throughout the study period between 20.5% and 24.2%, with an average
of 22.0% of adults reporting use of telehealth in the last four weeks.
• Telehealth use rates were lowest among people who are uninsured (9.4%), young adults ages 18 to
24 (17.6%), and residents of the Midwest (18.7%).
• The highest rates of telehealth visits were among those covered by Medicaid (28.3%) and Medicare
(26.8%), individuals who are Black (26.1%), and those earning less than $25,000 (26.4%).
• Individuals who are Hispanic or Latino, Black, and Asian were more likely to use telehealth,
specifically audio-only telehealth, than individuals who are White; however, they were less likely to
use video telehealth services than individuals who are White. There were significant disparities
among subgroups in terms of audio-only versus video-based telehealth use.
• Persistent disparities in accessing video telehealth services requires further study on patient
preferences and how broadband programs, technology resources, and technology literacy training
programs can improve patient access to video telehealth services.
April 19, 2023

April 2023
ISSUE BRIEF
2
BACKGROUND
Telehealth use in the United States grew significantly within the first three months of the COVID-19 pandemic
(January – March 2020), providing access to critical health services, enabling communication between health
care providers and patients, and remote monitoring of conditions through the use of synchronous, real-time
modalities via audio-only or internet-based video on mobile phones and digital devices as well as
asynchronous methods (e.g., store and forward and patient portals).
5, 6
Telehealth use in the last half of 2020 remained high, accounting for 30.2% of all health center visits during
June – November 2020, according to one study.
7
By April 2021, the national telehealth utilization rate among
adults ages 18 years and older was at 27%, which is lower than early pandemic telehealth use, but then
declined to 22% by mid-late 2021 based on an earlier ASPE study.
1
Analyses of commercial claims have shown
that telehealth services were mostly rendered by social workers and primary care and psychiatry/psychology
clinicians, with more than a quarter (26%) of claims for psychotherapy delivered through telehealth.
8
However,
while evidence on patient preferences regarding modality and the impact of telehealth on quality of care and
patient outcomes is still being explored, equitable access to telehealth services – particularly synchronous,
real-time video telehealth – remains a significant concern and potential barrier to health care during the
pandemic.
9
The expected end of the public health emergency on May 11, 2023 may impact telehealth flexibilities
introduced during the pandemic for various state Medicaid programs and private payers.
4
In addition, recent
legislation extended telehealth flexibilities for Medicare until December 31, 2024 to further understand
ongoing patterns of telehealth utilization and disparities which are critical to informed policy-making.
10
This report provides an update to an earlier ASPE Issue Brief that analyzed telehealth utilization using the
Census Bureau’s Household Pulse Survey (HPS) from April 14, 2021 to October 11, 2021.
1
Specifically, in this
study, national trends in telehealth utilization were analyzed from April 14, 2021 through August 8, 2022 with
results that are similar to the previous analysis. In addition, descriptive and multivariable regression analyses
were performed to better understand telehealth use and more specifically video-enabled telehealth among
different populations.
METHODS
Data Sources
We used the Household Pulse Survey (HPS) data. This is an online survey, administered by the Census Bureau
to measure U.S. households’ experiences and impact of emerging issues during the COVID-19 pandemic. The
HPS response rate ranges from 1.3% to 10.3% and varies across survey cycles.
11
Respondents must be adults ages 18 and older and they are asked to answer questions on use of telehealth for
both themselves and children in their household.
*
_______________________
*
The survey telehealth questions included the following: “At any time in the last 4 weeks, did you have an appointment with a doctor,
nurse, or other health professional by video or by phone? Please only include appointments for yourself and not others in your
household.” “At any time in the last 4 weeks, did any children in the household have an appointment with a doctor, nurse, or other
health professional by video or by phone?” For those who selected Yes: “Did the appointment(s) take place over the phone without
video or did the appointment(s) use video?”
† We grouped respondents based on their answers to health insurance coverage into five mutually exclusive categories: 1) Medicare; 2)
Medicaid; 3) Private; 4) Other Health Insurance, and 5) Uninsured.
‡ Biological sex and gender identity were excluded from the overall telehealth analysis, due to a change in the definition of gender in
the survey as of July 21, 2021.

April 2023
ISSUE BRIEF
3
Data on overall telehealth use was available for the weeks between April 14, 2021 through August 8, 2022, our
study period. Information on telehealth service by modality (audio-only vs. video telehealth) was available only
for the weeks from July 21, 2021 to August 8, 2022.
12
Data Analysis
Overall telehealth use was evaluated from April 14, 2021, to August 8, 2022, for adult telehealth users
(N=265,367). Analysis by telehealth modality (video vs. audio-only) was performed on a secondary cohort* (N=
143,462 respondents from July 21, 2021 through August 8,2022)) representing a subset of the first cohort of
overall telehealth users.
The data were weighted using person-level weights and replicate weights to account for sampling and
response bias.
11
Descriptive statistics followed by bivariate analysis (stratification and crosstabulations) and
multivariable logistic regression modeling were conducted for both cohorts to identify predictors of telehealth
use. Independent variables in the multivariable model included race and ethnicity, age, gender, education,
income, insurance, and region. We repeated our multivariable analysis with the sample stratified by insurance
type. A p-value below .05 was considered statistically significant. All analyses used survey weights to mitigate
non-response bias and Taylor Series Expansion/Linearization for variance estimation.
RESULTS
Characteristics of Telehealth Users
Among the 1,180,248 adults who answered the
telehealth question, 22.5% reported having utilized
telehealth services (audio-only or video) within the
last four weeks. Among 367,887 adults with a child in
the household, 18.1% reported that a child in the
household had used telehealth services in the prior
four weeks.
Figure 1 shows trends in the percentage of adults and
children that had used telehealth services in the prior
four weeks. There was a slight decline in overall
telehealth use in July 2021 that persisted until June
of 2022 before climbing again slightly; however,
telehealth use among adults remained above 20% throughout the study period. Rates for children were slightly
lower, and the gap compared to adults has gradually widened over time. While other studies have found that
overall rates of telehealth use have remained fairly stable for adults, rates for children have gradually declined
in 2022.
13
In one study, telehealth use among pediatric patients varied by subspecialty ranging from 6% to 73%
of total visits with a preference for in-person visits among those having non-English language preference.
14, 15
Telehealth use consistently
remained above 20% from
2021-2022 and for all
population groups.
Disparities persisted in video
utilization from July 2021 to
August 2022.

April 2023
ISSUE BRIEF
4
Figure 1. Percentage of Adults and Children* Who Used Telehealth Services, April 14, 2021 – August 8, 2022
Figure 2 illustrates the share of adults with telehealth visits who utilized audio-only versus video telehealth.
More than half of telehealth users reported use of video telehealth during each wave of the survey from July
2021 to August, 2022, but decreased during June 1, 2022 through August 8, 2022, for reasons that are not yet
well understood.
Note: *Reflects telehealth use reported by adult respondents for any child in the household over the
previous 4 weeks. Note that the survey is typically on a bi-weekly basis, although some weeks were
not surveyed, such as weeks in November of 2021.

April 2023
ISSUE BRIEF
5
Figure 2. Percentage of Adults Who Used Audio-only vs. Video Telehealth Services, July 21, 2021 – August 8,
2022
Demographic Characteristics of Overall and Audio-only vs. Video Adult Telehealth Use
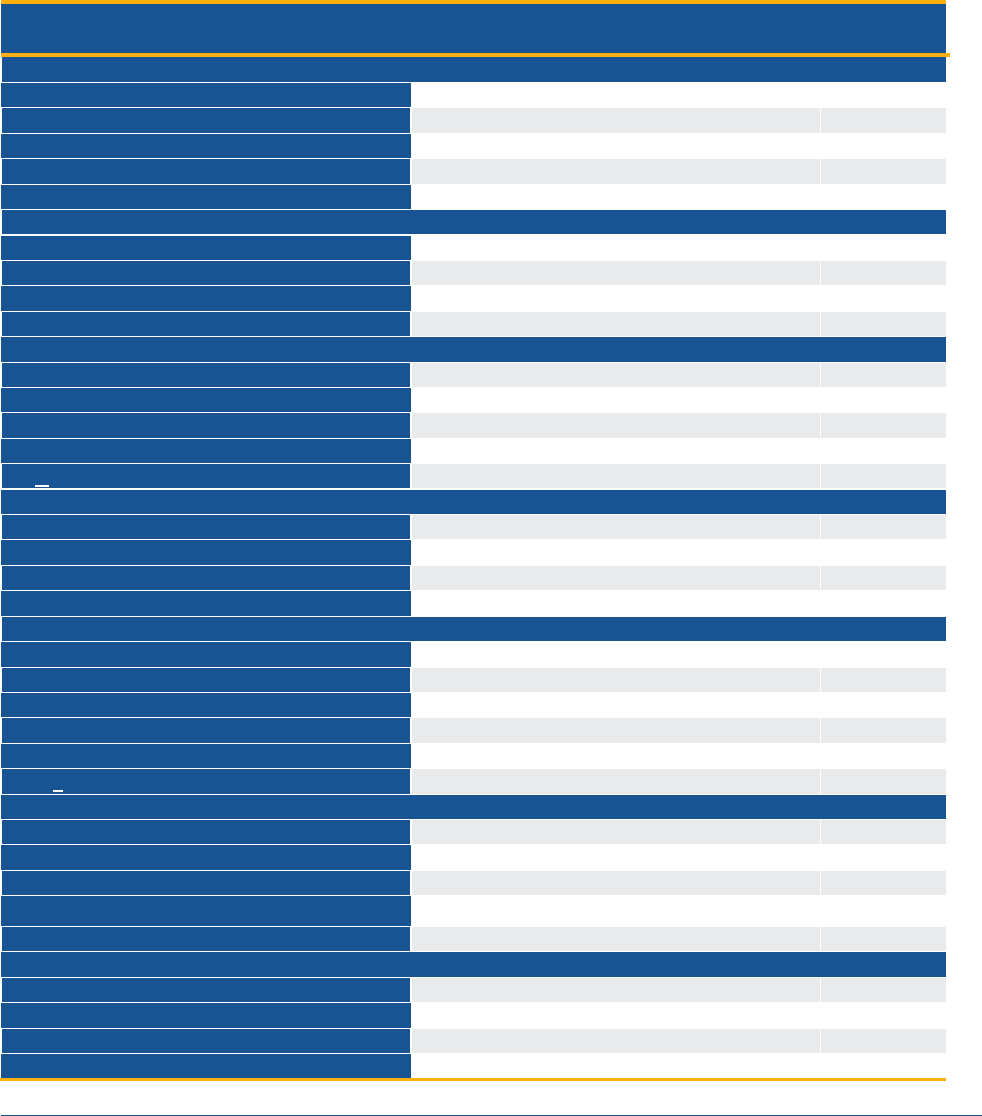
Table 1 presents the findings by demographic categories for each of the two cohorts analyzed: overall
telehealth users (first cohort) and the proportion of survey respondents who reported the modality of
telehealth visit in the prior four weeks from July 2021-August 2022 (second cohort).
Among survey respondents (first cohort), telehealth utilization was lowest among people who were uninsured
(9.4%), individuals ages 18-24 (17.6%), and those residing in the Midwest (18.7%). Telehealth use was highest
among those with Medicaid (28.3%) and Medicare (26.8%), Black respondents (26.1%), and those earning less
than $25,000 (26.4%).
Subgroup analysis comparing audio-only vs. video telehealth among telehealth users was conducted for the
second cohort* surveyed between July and August 2021. Although we acknowledge differences in the two
cohorts that make them not comparable, we noted that the characteristics of those reporting higher
proportion of video services (second cohort) were similar with those having a lower overall telehealth use (first
cohort). Among these respondents (second cohort), higher proportion of video visits compared to audio-only
visits were observed in those having lower overall rates of telehealth use. For example, White respondents
reported having an overall telehealth use of 19.6% but had a higher proportion of their telehealth visits using
video (61.3%) compared to audio-only (38.7%). This pattern remained consistent among telehealth users who
were between 18 and 24 years of age (72.5%), and private health insurance enrollees (65.3%). Audio-only
telehealth use was highest among those with less than a high school education (64.2%) and adults ages 65 and
58 58
57
58
60
58
57
56
58
60 60
57
55
54
53
42 42
43
42
40
42
43
44
42
40 40
43
45
46
47
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Percentage (%) of audio vs. video telehealth use
Week Survey was Administered
(HPS weeks 34-48)
Audio vs. Video Telehealth Use
Video Telehealth
Audio Telehealth

April 2023
ISSUE BRIEF
6
older (56.5%). These results are similar to the findings from our previous analysis of Census HPS data through
October 11, 2021.
1
* Note: The telehealth modality question was included in the Household Pulse Survey (HPS) starting July 21,
2021.
Table 1. Rates of Telehealth Use and Audio-only vs. Video Modality, by Demographic Categories, April 14,
2021 – August 8, 2022
% with a
Telehealth Visit
in Previous Four
Weeks
April 14, 2021 to
August 8, 2022
Second Cohort* (July 21, 2021 to August 8, 2022)
% with a
Telehealth Visit in
Previous Four
Weeks
% of Telehealth
Visits by Video in
Previous Four
Weeks
% of Telehealth
Visits by Audio-
only in Previous
Four Weeks
Race and Ethnicity
Hispanic or Latino
23.9
22.7
49.7
50.3
White alone, not Latino
20.7
19.6
61.3
38.7
Black alone, not Latino
26.1
25.0
50.1
49.9
Asian alone, not Latino
21.7
20.8
49.5
50.5
Two or more races + Other
25.5
24.2
59.8
40.2
Age
18-24 years
17.6
16.0
72.5
27.5
25-39 years
20.7
18.6
69.3
30.7
40-54 years
22.7
20.9
60.9
39.1
55-64 years
23.6
21.1
52.1
47.9
> 65 years
24.6
22.0
43.5
56.5
Education
Less than high school
24.5
24.0
35.8
64.2
High school or GED
20.7
19.7
46.5
53.5
Some college/Associate’s
degree
22.8
21.6
58.3
41.7
Bachelor’s degree or higher
22.4
21.3
66.7
33.3
Household Income
Less than $25,000
26.4
25.3
47.6
52.4
$25,000 - $34,999
23.3
21.9
48.9
51.1
$35,000 - $49,999
21.8
20.6
53.3
46.7
$50,000 - $74,999
21.0
19.9
56.9
43.1
$75,000 - $99,999
20.2
19.2
62.0
38.0
> $100,000
20.4
19.4
67.9
32.1
Insurance
Medicare
26.8
25.5
46.1
53.9
Medicaid
28.3
26.8
53.4
46.6
Private
20.2
19.2
65.3
34.7
Other Health Insurance
24.4
23.1
53.8
46.2
Uninsured
9.4
9.0
46.9
53.1
Census Region
Northeast
23.3
22.3
59.6
40.4
South
21.3
20.1
58.0
42.0
Midwest
18.7
17.7
57.7
42.3
West
24.9
23.9
54.1
45.9

April 2023
ISSUE BRIEF
7
Figure 3 illustrates disparities in video telehealth use by race and ethnicity; video telehealth as a share of all
telehealth use was lower among Hispanic or Latino (49.7%), Asian (49.5%), and Black (50.1%) survey
respondents.
Figure 3. Telehealth Modality (Video vs. Audio-only) Among Telehealth Users, By Race/Ethnicity, July 21,
2021 – August 8, 2022
Demographic Predictors Associated with Telehealth Use (Multivariable Model: First Cohort)
Table 2 shows the demographic factors that were predictors of recent telehealth use after multivariable
adjustment (first cohort). Those who were Hispanic or Latino, Black, or reported two or more races or other
race had higher odds of using telehealth in the last 4 weeks than White non-Latino respondents. In addition,
telehealth use was highest among those with lower incomes and declined as income rises. Individuals with
Medicare, Medicaid, or Other insurance
†
were more likely to use telehealth than those with Private Insurance,
while people without any health insurance were the least likely to use telehealth.
_______________________
†
Other insurance includes: TRICARE or other military health care, Veteran’s Administration (VA) Health Care, Indian Health Service
(IHS), and Other health insurance.
49.7
61.3
50.1
49.5
59.8
50.3
38.7
49.9
50.5
40.2
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Hispanic or
Latino
White Black Asian Two or more
races + Other
% of utilization by telehealth users
Telehealth Use by Modality
% video telehealth % audio telehealth

April 2023
ISSUE BRIEF
8
Table 2: Adjusted Odds of Telehealth Utilization by Respondent Demographics, April 14, 2021 – August 8,
2022
Demographics
Odds Ratios
(95% Confidence Interval)
P-value
Race and Ethnicity
Hispanic or Latino
1.27 (1.22, 1.33)
<.0001
Black alone, not Latino
1.36 (1.30, 1.42)
<.0001
Asian alone, not Latino
1.02 (0.96, 1.08)
0.6085
Two or more races + Other Races, not Latino
1.27 (1.20, 1.35)
<.0001
White alone, not Latino
Ref*
Ref*
Age
18-24 years
1.06 (0.96, 1.16)
0.2701
25-39 years
1.19 (1.12, 1.26)
<.0001
40-54 years
1.35 (1.28, 1.43)
<.0001
55-64 years
1.39 (1.32, 1.46)
<.0001
> 65 years
Ref*
Ref*
Education
Less than high school
0.91 (0.78, 1.05)
0.1988
High school or GED
0.77 (0.74, 0.80)
<.0001
Some college/Associate’s degree
0.95 (0.92, 0.97)
<.0001
Bachelor’s degree or higher
Ref*
Ref*
Household Income
Less than $25,000
1.41 (1.34, 1.48)
<.0001
$25,000 - $34,999
1.27 (1.21, 1.34)
<.0001
$35,000 - $49,999
1.15 (1.10, 1.21)
<.0001
$50,000 - $74,999
1.06 (1.03, 1.10)
0.0011
$75,000 - $99,999
1.03 (0.99, 1.07)
0.1532
> $100,000
Ref*
Ref*
Insurance
Medicare
1.70 (1.62, 1.79)
<.0001
Medicaid
1.36 (1.30, 1.44)
<.0001
Private
Ref*
Ref*
Other Health Insurance
1.24 (1.13, 1.35)
<.0001
Uninsured
0.35 (0.32, 0.38)
<.0001
Census Region
Northeast
0.91 (0.88, 0.95)
<.0001
South
0.82 (0.79, 0.85)
<.0001
Midwest
0.70 (0.67, 0.72)
<.0001
West
Ref*
Ref*
†Telehealth modalities were unavailable until HPS week 34 conducted on July 21, 2021.
‡ Insurance categories were coded to be mutually exclusive.
* Reference value/control group for calculation of odds ratios intervals.
Table 3 shows the demographic predictors of video telehealth among telehealth users after multivariable
adjustment (second cohort). Age was the strongest predictor of video telehealth use, with young adults having
an odds ratio of 4.55 compared to adults 65 and older and a declining rate of video telehealth use for each
older age group. Compared to females, males were less likely to use video telehealth, whereas transgender
individuals were 3.12 times more likely to use video telehealth.
April 2023
ISSUE BRIEF
9
Video telehealth use was less likely among lower income households and those with lower educational
attainment compared to those who had a household income of ≥ $100,000 and a bachelor’s degree or higher.
The rates of video telehealth use rose steadily as household income or educational attainment increased.
Black, Hispanic or Latino, and Asian individuals were less likely to use video telehealth than White respondents,
with Asians having the lowest odds ratio of 0.55. Respondents who were insured by Medicare were 1.23 times
more likely to use video telehealth compared to those who were insured by a private payer. Lastly, those
residing in the Midwest region were less likely to use video telehealth compared to those residing in the West.
Table 3: Predictors of Video Telehealth Utilization Among Telehealth Users, July 21, 2021 – August 8, 2022
Demographics
Odds Ratios
(95% Confidence Interval)
P-value
Race and Ethnicity
Hispanic or Latino
0.74 (0.66, 0.83)
<.0001
Black alone, not Latino
0.85 (0.76, 0.96)
0.0077
Asian alone, not Latino
0.55 (0.47, 0.64)
<.0001
Two or more races + Other, not Latino
0.98 (0.84, 1.14)
0.7527
White alone, not Latino
Ref*
Ref*
Gender Identity
Male
0.929 (0.87, 1.00)
0.038
Female
Ref*
Ref*
Transgender
3.12 (1.72, 5.68)
0.0002
Other
1.10 (0.83,1.46)
0.4998
Age
18-24 years
4.55 (3.51, 5.91)
<.0001
25-39 years
4.12 (3.60, 4.71)
<.0001
40-54 years
2.73 (2.42, 3.08)
<.0001
55-64 years
1.92 (1.70, 2.16)
<.0001
> 65 years
Ref*
Ref*
Education
Less than high school
0.50 (0.347 0.709)
0.0001
High school or GED
0.60 (0.541 0.657)
<.0001
Some college/associate’s degree
0.81 (0.753 0.864)
<.0001
Bachelor’s degree or higher
Ref*
Ref*
Household Income
Less than $25,000
0.61 (0.54, 0.69)
<.0001
$25,000 - $34,999
0.61 (0.54, 0.70)
<.0001
$35,000 - $49,999
0.69 (0.61, 0.78)
<.0001
$50,000 - $74,999
0.76 (0.69, 0.84)
<.0001
$75,000 - $99,999
0.82 (0.74, 0.91)
0.0002
> $100,000
Ref*
Ref*
Insurance
Medicare
1.23 (1.09, 1.38)
0.0005
Medicaid
0.99 (0.87, 1.13)
0.8709
Private
Ref*
Ref*
Other Health Insurance
0.97 (0.78, 1.22)
0.8145
Uninsured
0.73 (0.57, 0.94)
0.0137
Census Region
Northeast
1.07 (0.96, 1.19)
0.2474
South
1.05 (0.96, 1.14)
0.2648
Midwest
0.86 (0.78, 0.94)
0.0015
West
Ref*
Ref*

April 2023
ISSUE BRIEF
10
†Telehealth modalities were unavailable until HPS week 34 conducted on July 21, 2021.
‡ Insurance categories were coded to be mutually exclusive.
*Reference value/control group for calculation of odds ratios intervals.
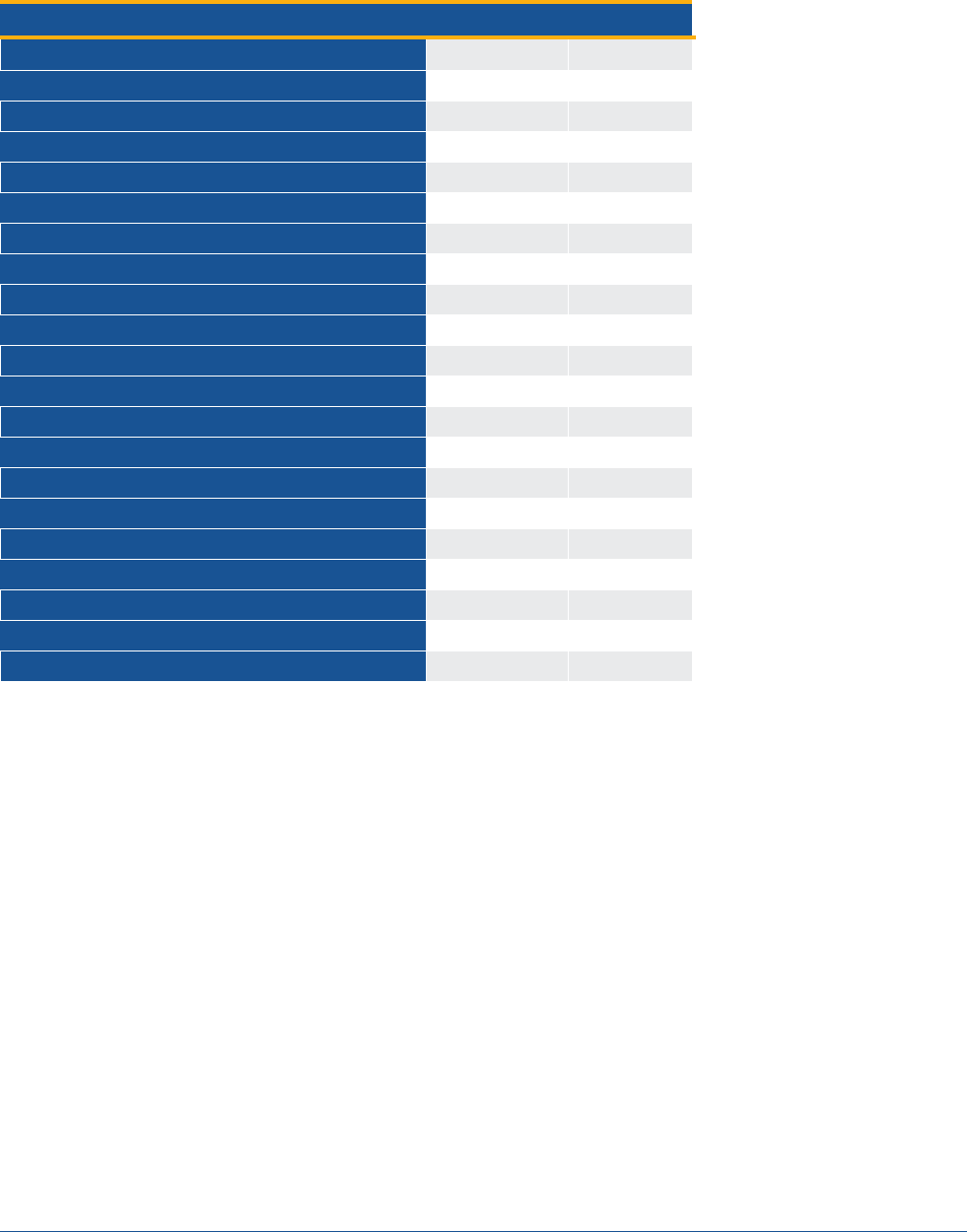
Table 4 shows demographic predictors of video telehealth use by individuals, stratified by different insurance
types. Disparities in access to video telehealth were observed in most insurance types similar to the overall
telehealth users. Generally, younger adults, those with higher incomes, and those with more education were
more likely to use video telehealth across insurance types. One notable exception is the absence of disparities
among Black and Latino respondents compared to White respondents covered by Medicare; however,
disparities in video telehealth access were greater among Asian respondents. These findings suggest Medicare
may provide more equitable access to video telehealth services compared to other payers but can improve its
access for Asians.

April 2023
ISSUE BRIEF
11
Table 4: Predictors of Video Telehealth Utilization Among Telehealth Users, Stratified by Insurance Type, July 21, 2021 – August 8, 2022
* Significant – p-value below 0.05
**Reference value/control group for calculation of odds ratios intervals.
Demographics
Medicare
OR (95% CI) P-value
Medicaid
OR (95% CI) P-value
Private
OR (95% CI) P-value
Other Health Insurance
OR (95% CI) P-value
Uninsured
OR (95% CI) P-value
Race and Ethnicity
Hispanic or Latino
0.88 (0.71, 1.11)
0.286
0.57 (0.43, 0.77)
0.0002*
0.76 (0.66, 0.88)
0.0003*
1.08 (0.61, 1.91)
0.787
0.50 (0.28, 0.89)
0.017*
Black alone, not Latino
1.08 (0.89, 1.31)
0.453
0.62 (0.46, 0.83)
0.001*
0.83 (0.70, 0.99)
0.037*
0.57 (0.31, 1.03)
0.060
0.99 (0.49, 1.99)
0.969
Asian alone, not Latino
0.49 (0.34, 0.70)
0.0001*
0.42 (0.23, 0.76)
0.004*
0.59 (0.49, 0.71)
<.0001*
1.51 (0.52, 4.32)
0.447
0.24 (0.09, 0.66)
0.006*
Two+ races / Other, not Latino
0.98 (0.73, 1.33)
0.915
0.76 (0.52, 1.10)
0.142
1.01 (0.82, 1.23)
0.952
1.62 (0.75, 3.48)
0.221
0.78 (0.25, 2.41)
0.659
White alone, not Latino
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Gender Identity
Male
0.92 (0.82, 1.04)
0.171
0.97 (0.76, 1.25)
0.833
0.96 (0.88, 1.05)
0.387
0.97 (0.65, 1.45)
0.863
0.50 (0.31, 0.79)
0.003*
Female
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Transgender
4.37 (0.92,
20.75)
0.063
3.18 (1.26, 8.04)
0.015*
2.21 (1.02, 4.76)
0.044*
755.88, (19.52,
>999.99)
0.0004*
2.26 (0.2, 25.34)
0.510
Other
1.01 (0.59, 1.73)
0.987
1.2 (0.63, 2.3)
0.575
1.15 (0.77, 1.71)
0.495
0.75 (0.21, 2.66)
0.652
0.83 (0.18, 3.94)
0.814
Age
18-24 years
9.92 (3.57, 27.6)
<.0001*
3.14 (1.30, 7.56)
0.011*
5.04 (3.63, 7.00)
<.0001*
3.49 (1.03, 11.75)
0.044*
2.26 (0.48,
10.77)
0.305
25-39 years
4.02 (2.67, 6.05)
<.0001*
3.85 (1.92, 7.73)
0.0001*
4.34 (3.60, 5.24)
<.0001*
2.37 (1.17, 4.83)
0.017*
2.2 (0.67, 7.26)
0.197
40-54 years
2.31 (1.88, 2.83)
<.0001*
2.26 (1.13, 4.51)
0.021*
3.13 (2.61, 3.76)
<.0001*
1.44 (0.73, 2.85)
0.290
1.41 (0.43, 4.69)
0.571
55-64 years
2.25 (1.90, 2.67)
<.0001*
1.69 (0.83, 3.46)
0.151
1.97 (1.63, 2.37)
<.0001*
0.99 (0.53, 1.84)
0.967
1.07 (0.32, 3.62)
0.914
> 65 years
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Education
Less than high school
0.51 (0.28, 0.94)
0.030*
0.50 (0.24, 1.04)
0.062*
0.34 (0.17, 0.67)
0.002*
0.03 (0.00, 0.32)
0.004*
1.51 (0.50, 4.59)
0.466
High school or GED
0.67 (0.58, 0.79)
<.0001*
0.57 (0.43, 0.75)
<.0001*
0.59 (0.51, 0.68)
<.0001*
0.53 (0.29, 0.95)
0.033*
0.70 (0.41, 1.19)
0.187
Some college/associate’s degree
0.84 (0.75, 0.94)
0.002*
0.87 (0.69, 1.10)
0.240
0.76 (0.69, 0.84)
<.0001*
1.14 (0.76, 1.70)
0.537
1.04 (0.64, 1.68)
0.882
Bachelor’s degree or higher
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Household Income
Less than $25,000
0.50 (0.41, 0.61)
<.0001*
0.66 (0.42, 1.04)
0.073
0.61 (0.49, 0.78)
<.0001**
1.04 (0.52, 2.09)
0.906
0.97 (0.43, 2.18)
0.938
$25,000 - $34,999
0.57 (0.46, 0.7)
<.0001*
0.62 (0.38, 1.00)
0.050*
0.65 (0.53, 0.79)
<.0001*
0.69 (0.35, 1.34)
0.268
0.7 (0.29, 1.71)
0.429
$35,000 - $49,999
0.72 (0.59, 0.88)
0.001*
0.62 (0.37, 1.03)
0.065
0.69 (0.57, 0.82)
<.0001*
0.77 (0.4, 1.47)
0.423
0.94 (0.37, 2.37)
0.895
$50,000 - $74,999
0.71 (0.59, 0.85)
0.0002*
0.79 (0.46, 1.35)
0.386
0.79 (0.70, 0.90)
0.0002*
0.71 (0.36, 1.42)
0.336
1.13 (0.48, 2.64)
0.777
$75,000 - $99,999
0.86 (0.71, 1.04)
0.125
0.91 (0.44, 1.91)
0.810
0.81 (0.72, 0.92)
0.001*
0.78 (0.38, 1.6)
0.498
0.9 (0.32, 2.58)
0.850
> $100,000
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Ref**
Census Region
Northeast
0.85 (0.7, 1.02)
0.086
1.03 (0.76, 1.39)
0.866
1.24 (1.07, 1.42)
0.003*
1.42 (0.64, 3.17)
0.387
0.91 (0.39, 2.14)
0.825
South
0.66 (0.56, 0.77)
<.0001*
0.87 (0.66, 1.15)
0.325
0.98 (0.86, 1.11)
0.712
1.2 (0.65, 2.19)
0.563
0.85 (0.42, 1.71)
0.643
Midwest
0.80 (0.7, 0.93)
0.003*
1.12 (0.86, 1.45)
0.421
1.18 (1.06, 1.33)
0.003*
1.56 (0.96, 2.52)
0.073
0.79 (0.46, 1.37)
0.401
West
Ref
Ref
Ref
Ref
Ref
Ref
Ref
Ref
Ref
Ref

April 2023
ISSUE BRIEF
12
DISCUSSION
Overall, 22.0% of adults reported using telehealth in the last four weeks of the study period (from April 2021 to
August 2022), which is comparable to ASPE’s previous analysis.
1
It should be noted that the Census Pulse data
on telehealth use reported in this paper is markedly lower, most likely due to the shorter reference period of
telehealth use (four weeks only), compared to higher rates of telehealth use by adults (37.0%) in twelve
months that was reported using the 2021 National Health Interview Survey (NHIS) administered by CDC.
16-18
The methodology is different as well. The NHIS is a long running nationally-representative health survey that
tracks a number of health care metrics. The HPS, launched in 2020, was designed as an experimental data
collection initiative to provide near real-time national estimates based on weighting procedures and
administered as a 20-minute online survey to adults 18 years and older. Another difference to note is that the
HPS included questions on modality, (video, and audio-only), while this information cannot be obtained using
the NHIS because no questions related to telehealth modality were included in the survey.
During the COVID-19 pandemic, telehealth has emerged as an important modality for many, especially
those in underserved communities where it has resulted in a reduction of no-show rates.
19,20
Despite the
enhanced access to health care, disparities in video telehealth access continue to persist among older
patients, people of color, and those with low technology literacy.
21, 22
In addition, factors such as inadequate
infrastructure (e.g., internet connection, technology access, workflows) may impact a provider’s ability to
offer video telehealth.
23
One study found that providers in small practices from communities with high
social vulnerability
‡
were almost twice as likely as providers in communities with low social vulnerability to
use telephones as their primary telehealth modality.
24, 25
Emerging evidence suggests patient satisfaction is higher with video telehealth visits compared to audio-only
telehealth.
26, 27
Studies have also shown that consults via video telehealth are preferred by patients,
28
with
evidence of improved patient outcomes
29
and being less likely to have emergency department (ED) visits, in-
person, and hospital visits compared to those who did not use video telehealth.
30
However, there is conflicting
evidence on whether there are disparities in patient satisfaction with telehealth services among Asian
patients.
31
More evidence is needed on patient preferences of telehealth modalities (e.g., video vs. audio
telehealth) compared to each other and to usual care (in-person visits).
32
In addition, it is important to expand
on smaller studies
33
and studies outside of the U.S.
34
to assess whether there are any differences in these
preferences and patient perceptions of their care across populations in the U.S.
Our subgroup analysis found disparities in video telehealth use across payers. For example, Black, Hispanic or
Latino, and Asian individuals covered by Medicaid and private insurance were less likely to use video
telehealth; however, our model showed that only Asians were less likely to use video telehealth among those
covered by Medicare while both Hispanic or Latinos and Asians were less likely to use video telehealth among
individuals who are uninsured.
Those covered by Medicaid had the highest rate of telehealth utilization compared to individuals with other
sources of coverage, comparable to findings from a previous ASPE analysis.
1
However, based on an ASPE report
from January 2022, the status of state Medicaid telehealth flexibilities varied widely and continued to change
frequently throughout the pandemic.
4
Some states expanded the use of telehealth permanently, others
rescinded all or some of their telehealth flexibilities making some permanent through state legislation, while
others were maintained pending the expiration of their state or federal PHE declaration. Variations in state
_______________________
‡
The CDC defines social vulnerability as “the potential negative effects on communities caused by external stresses on human health.
Such stresses include natural or human-caused disasters, or disease outbreaks. Reducing social vulnerability can decrease both human
suffering and economic loss.”
23

April 2023
ISSUE BRIEF
13
Medicaid telehealth policies may impact patients’ and providers’ understanding of what types of visits will be
covered and how services should be billed. There are also numerous equity implications in a telehealth
landscape that is constantly shifting. When both federal and state PHEs expire and Medicaid redeterminations
resume starting on April 1, 2023, millions of those insured by Medicaid will be impacted through changes in
health insurance coverage and may experience changes in their access to health care services, including those
provided by telehealth.
10
The findings of our study suggest those insured by Medicare as being more likely to use telehealth and video
telehealth. These findings are consistent with our previous HPS analysis
1
and Medicare FFS claims analyses
conducted by ASPE which showed significant increases in use of telehealth by those insured by Medicare
during the pandemic.
2
However, those responding to the HPS survey may have higher digital literacy or
internet access given its administration as an online survey. Another study found individuals covered by
Medicare are less likely to use video telehealth. This study also noted that a potential reason for an overall
decrease in telehealth use among older patients may be related to their demographic and geographic
distribution, such as a higher share of older adults living in rural areas and lower rates of internet access.
35
Our study also found respondents reporting as Hispanic or Latino, Black, two or more races and other races
had higher overall telehealth use than White or Asian respondents. Despite higher odds of overall telehealth
use, Hispanic or Latino, Black, and Asian respondents were significantly less likely to use video telehealth—
particularly among those with Medicaid or private coverage—compared to their White counterparts. Video
telehealth use rates increased with higher income and education levels and younger age. These results are
somewhat counter to a study based on an analysis of the American Life Panel survey, which showed that video
telehealth use was highest in early 2021 among Black adults, and among those who were younger, had less
than high school education, and had lower income. In addition, the study reported respondents’ desire to use
video telehealth had increased from pre-pandemic estimates.
36
Our results are, however, similar to other studies finding disparities in video access to telehealth. For instance,
in a study of neurology patients, demographic predictors of those less likely to use video telehealth compared
to audio-only telehealth use included patients who were low-income, Black, and those insured by Medicare or
Medicaid.
30
Other studies have also shown lower success in initiating video telehealth visits among Hispanic or Latino
patients, those who had low socioeconomic status (SES), and individuals insured by Medicare or Medicaid.
21, 37,
38
Potential reasons for unsuccessful initiation of video telehealth visits may be potential technology barriers,
as evidenced in one study including those who did not activate their patient portal prior to the visit.
39
Another
study compared video telehealth utilization pre and post COVID-19 PHE and found lower video telehealth rates
among males, Asian, Black, American Indian / Alaska Native patients, patients who had limited English
proficiency, and those who were insured by Medicaid or Medicare.
40
Younger patients had a preference for
video telehealth compared to older adults.
41
In general, these patterns of disparities likely reflect structural barriers to video telehealth, such as access to
technology, devices, broadband internet, technology literacy, and structural racism.
40
Additional research is
needed on which health conditions and health services are clinically appropriate to be delivered via telehealth
as well as whether video or audio may be a clinically preferred telehealth modality. For example, video
telehealth visits may be more appropriate than audio visits for certain clinical conditions and health services
requiring visual clues and examination (e.g., dermatology and surgical wound care).
42
However, if health
services cannot be accessed in the modality (in-person, video or audio telehealth) associated with the
strongest evidence, patient populations may be limited in accessing higher quality care which may affect
health outcomes.
43
Further assessment of telehealth’s impact on health outcomes will also require

April 2023
ISSUE BRIEF
14
standardized measures such as the Health Care Effectiveness Data and Information Set (HEDIS) quality
performance measures.
44
Limitations
This analysis has several limitations including the survey’s response rate that ranges from 1.3 percent to 10.3
percent, depending on the week. Despite applying weights to mitigate non-response bias, the inherent nature
of internet-based surveys can produce a bias based on the respondents’ internet accessibility and level of
comfort and familiarity with technology. Those who have access to technology and higher levels of health
literacy in general, as well as digital literacy, are more likely to respond to online surveys such as the HPS,
which can limit its generalizability to other populations. Our analysis was not able to control for baseline
differences in overall rates of health care use. Groups reporting higher telehealth use in the last four weeks
may simply reflect groups that are more likely to use health care services. Finally, the HPS did not include data
to distinguish rural and urban geographic areas; therefore, a comparison could not be made.
Policy Implications
Recent studies showed that video telehealth utilization is associated with a clinical provider’s perception of its
quality and comparability to in-person visits,
45
as well as whether available technologies are functional and
user-friendly in supporting video telehealth.
46
Furthermore, limited technology and health literacy continue to
pose challenges for accessing telehealth services among patients with limited English proficiency (LEP). New
evidence suggests prior video visit experience may help overcome barriers to video telehealth use.
47
However,
the current state of technology and user-friendliness of remote monitoring devices that link to telehealth visits
vary, as well as its acceptance among patients, especially those requiring assistance from others initiating
telehealth visits and interventions.
48
A resource that has been studied to enhance accessibility of telehealth has been the use of patient navigators
and community health workers to support patients in a telehealth visit. In addition to improving access to
video visits, one study demonstrated a return on investment (ROI) through increased adherence to clinic visits
that offset implementation costs.
49
This suggests additional policies may be considered for patient navigators
and community health workers to assist patients with telehealth visits.
While video telehealth may be more comparable to in-person visits, audio-only telehealth continues to be
important as it provides critical health care access for marginalized populations who lack access to technology,
broadband or ability to navigate a video telehealth visit. More work needs to be done to enable equitable
access to video telehealth by addressing disparities that are further exacerbated by lack of broadband access
or limitations in high-speed access impacting those residing in rural areas the most.
50
The challenge with
adequate broadband access are being addressed through programs and grants offered by the Federal
Communications Commission (FCC) and the U.S. Department of Commerce National Telecommunications and
Information Administration (NTIA) with appropriations from the Infrastructure Investment and Jobs Act
(IIJA).
51,52,53
In the future, new alternative models for telehealth expansion may need to consider potential
access issues
54
especially among individuals who are uninsured.
19
CONCLUSION
Our study describes recent trends in the use of telehealth during the pandemic that may have implications for
policymakers as they consider whether to continue policies and flexibilities that enable access to telehealth
services. In addition, our study suggests the importance of reducing disparities in accessing telehealth services,
especially video, and highlights the need to improve access by providing more focused outreach to
communities who have lower levels of video telehealth utilization.

April 2023
ISSUE BRIEF
15
REFERENCES
1. Karimi M, Lee EC, Couture SJ, Gonzales AB, Grigorescu V, Smith SR, De Lew N, Sommers BD. National Trends in
Telehealth Use in 2021: Disparities in Utilization and Audio vs. Video Services. (Research Report No. HP-2022-04). Office
of the Assistant Secretary for Planning and Evaluation, U. S. Department of Health andHuman Services. Research Report.
February 2022. Accessed August 2, 2022.
https://aspe.hhs.gov/sites/default/files/documents/4e1853c0b4885112b2994680a58af9ed/telehealth-hps-ib.pdf
2. Samson L, Tarazi W, Turrini G, Sheingold S. Medicare Beneficiaries’ Use of Telehealth in 2020: Trends by Beneficiary
Characteristics and Location. (Issue Brief No. HP-2021-27). U.S. Department of Health and Human Services. December
2021. Accessed August 2, 2022.
https://aspe.hhs.gov/sites/default/files/documents/a1d5d810fe3433e18b192be42dbf2351/medicare-telehealth-
report.pdf
3. Chu R, Peters C, De Lew, N, and Sommers BD. State Medicaid Telehealth Policies Before and During the COVID-19 Public
Health Emergency. (Issue Brief No. HP-2021-17). U.S. Department of Health and Human Services. July 2021. Accessed
August 2, 2022. https://aspe.hhs.gov/sites/default/files/documents/eb9e147935a2663441a9488e36eea6cb/medicaid-
telehealth-brief.pdf
4. Rudich J, Conmy AB, Chu R, Peters C, De Lew N, Sommers BD. State Medicaid Telehealth Policies Before and During the
COVID-19 Public Health Emergency: 2022 Update. Office of the Assistant Secretary for Planning and Evaluation, U.S.
Department of Health and Human Services. November 2022. Accessed February 21, 2023.
https://aspe.hhs.gov/sites/default/files/documents/190b4b132f984db14924cbad00d19cce/Medicaid-Telehealth-IB-
Update-Final.pdf
5. Koonin LM, Hoots B, Tsang CA, et al. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic -
United States, January-March 2020. MMWR Morb Mortal Wkly Rep. Oct 30 2020;69(43):1595-1599.
doi:10.15585/mmwr.mm6943a3
6. HRSA. What is telehealth? Department of Health and Human Services. Accessed June 9, 2021.
https://telehealth.hhs.gov/patients/understanding-telehealth/
7. Demeke HB, Merali S, Marks S, et al. Trends in Use of Telehealth Among Health Centers During the COVID-19 Pandemic
— United States, June 26–November 6, 2020. Vol. 70.240–244. MMWR Morb Mortal Wkly Rep 2021. February 19, 2021
https://www.cdc.gov/mmwr/volumes/70/wr/mm7007a3.htm
8. FAIR HEALTH. Telehealth Utilization Fell Nearly Four Percent Nationally in June 2022. CISION PR Newswire; 2022.
September 12, 2022. https://www.prnewswire.com/news-releases/telehealth-utilization-fell-nearly-four-percent-
nationally-in-june-2022-301621770.html
9. White-Williams C, Liu X, Shang D, Santiago J. Use of Telehealth Among Racial and Ethnic Minority Groups in the United
States Before and During the COVID-19 Pandemic. Public Health Rep. Sep 16 2022:333549221123575.
doi:10.1177/00333549221123575
10. Department of Health and Human Services Assistant Secretary for Public Affairs.Fact Sheet: COVID-19 Public Health
Emergency Transition Roadmap. HHS Press Office; February 9, 2023, Accessed February 21, 2023.
https://www.hhs.gov/about/news/2023/02/09/fact-sheet-covid-19-public-health-emergency-transition-roadmap.html
11. United States Census Bureau. Household Pulse Survey Technical Documentation. Updated February 17, 2023. Accessed
March 16, 2023, https://www.census.gov/programs-surveys/household-pulse-survey/technical-documentation.html
12. U.S. Census Bureau. Data from: Measuring Household Experiences during the Coronavirus Pandemic. 2022.
https://www.census.gov/programs-surveys/household-pulse-survey/datasets.html.
13. Rabbani N, Chen JH. National Trends in Pediatric Ambulatory Telehealth Utilization and Follow-Up Care. Telemed J E
Health. Jan 2023;29(1):137-140. doi:10.1089/tmj.2022.0137
14. Ortega P, Shin TM, Martínez GA. Rethinking the Term "Limited English Proficiency" to Improve Language-Appropriate
Healthcare for All. J Immigr Minor Health. Jun 2022;24(3):799-805. doi:10.1007/s10903-021-01257-w
15. Uscher-Pines L, McCullough C, Dworsky MS, et al. Use of Telehealth Across Pediatric Subspecialties Before and During
the COVID-19 Pandemic. JAMA Netw Open. Mar 1 2022;5(3):e224759. doi:10.1001/jamanetworkopen.2022.4759
16. Lucas JW, Villarroel MA. Telemedicine use among adults: United States, 2021. Vol. no. 445. National Center for Health
Statistics. NCHS Data Brief. October 2022. Accessed January 9, 2023.
https://www.cdc.gov/nchs/products/databriefs/db445.htm
17. Villarroel MA, Lucas JW. QuickStats: Percentage of Persons Who Used Telemedicine During the Past 12 Months, by Age
Group — National Health Interview Survey, United States, 2021. Vol. 72.132. MMWR Morb Mortal Wkly Rep 2023.

April 2023
ISSUE BRIEF
16
February 3, 2023. Accessed March 16, 2023.
https://www.cdc.gov/mmwr/volumes/72/wr/mm7205a2.htm#suggestedcitation
18. Lucas JW, Villarroel MA, Cohen R. QuickStats: Percentage of Adults Aged 18–64 Years Who Used Telemedicine in the
Past 12 Months, by Sex and Health Insurance Coverage — National Health Interview Survey, United States 2021. Vol.
72.244. MMWR Morb Mortal Wkly Rep. March 3, 2023. Accessed March 16, 2023.
https://www.cdc.gov/mmwr/volumes/72/wr/mm7209a5.htm?s_cid=mm7209a5_w
19. Khairat S, Yao Y, Coleman C, McDaniel P, Edson B, Shea CM. Changes in Patient Characteristics and Practice Outcomes of
a Tele-Urgent Care Clinic Pre- and Post-COVID-19 Telehealth Policy Expansions. Perspect Health Inf Manag. Spring
2022;19(Spring):1k.
20. Sun CA, Perrin N, Maruthur N, Renda S, Levin S, Han HR. Predictors of Follow-Up Appointment No-Shows Before and
During COVID Among Adults with Type 2 Diabetes. Telemed J E Health. Nov 4 2022;doi:10.1089/tmj.2022.0377
21. Cousins MM, Van Til M, Steppe E, et al. Age, race, insurance type, and digital divide index are associated with video visit
completion for patients seen for oncologic care in a large hospital system during the COVID-19 pandemic. PLoS One.
2022;17(11):e0277617. doi:10.1371/journal.pone.0277617
22. Lau KHV, Anand P, Ramirez A, Phicil S. Disparities in Telehealth use During the COVID-19 Pandemic. J Immigr Minor
Health. Dec 2022;24(6):1590-1593. doi:10.1007/s10903-022-01381-1
23. Ranganathan C, Balaji S. Key Factors Affecting the Adoption of Telemedicine by Ambulatory Clinics: Insights from a
Statewide Survey. Telemed J E Health. Feb 2020;26(2):218-225. doi:10.1089/tmj.2018.0114
24. Chang JE, Lai AY, Gupta A, Nguyen AM, Berry CA, Shelley DR. Rapid Transition to Telehealth and the Digital Divide:
Implications for Primary Care Access and Equity in a Post-COVID Era. Milbank Q. Jun 2021;99(2):340-368.
doi:10.1111/1468-0009.12509
25. Centers for Disease Control and Prevention. CDC/ATSDR Social Vulnerability Index. Updated November 16, 2022.
Accessed March 14, 2023, 2023. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
26. Chen K, Lodaria K, Jackson HB. Patient satisfaction with telehealth versus in-person visits during COVID-19 at a large,
public healthcare system. J Eval Clin Pract. Sep 22 2022;doi:10.1111/jep.13770
27. Hays RD, Skootsky SA. Patient Experience with In-Person and Telehealth Visits Before and During the COVID-19
Pandemic at a Large Integrated Health System in the United States. J Gen Intern Med. Mar 2022;37(4):847-852.
doi:10.1007/s11606-021-07196-4
28. Srinivasulu S, Manze MG, Jones HE. "I totally didn't need to be there in person": New York women's preferences for
telehealth consultations for sexual and reproductive healthcare in primary care. Fam Pract. Sep 19
2022;doi:10.1093/fampra/cmac102
29. Graetz I, Huang J, Muelly ER, Hsueh L, Gopalan A, Reed ME. Video Telehealth Access and Changes in HbA1c Among
People With Diabetes. Am J Prev Med. May 2022;62(5):782-785. doi:10.1016/j.amepre.2021.10.012
30. Kummer BR, Agarwal P, Sweetnam C, et al. Trends in the Utilization of Teleneurology and Other Healthcare Resources
Prior to and During the COVID-19 Pandemic in an Urban, Tertiary Health System. Front Neurol. 2022;13:834708.
doi:10.3389/fneur.2022.834708
31. Acoba JD, Yin C, Meno M, et al. Racial Disparities in Patient-Provider Communication During Telehealth Visits Versus
Face-to-face Visits Among Asian and Native Hawaiian and Other Pacific Islander Patients With Cancer: Cross-sectional
Analysis. JMIR Cancer. Dec 9 2022;8(4):e37272. doi:10.2196/37272
32. Huang J, Graetz I, Millman A, et al. Primary care telemedicine during the COVID-19 pandemic: patient's choice of video
versus telephone visit. JAMIA Open. Apr 2022;5(1):ooac002. doi:10.1093/jamiaopen/ooac002
33. Knaus ME, Kersey K, Ahmad H, et al. Both sides of the screen: Provider and patient perspective on telemedicine in
pediatric surgery. J Pediatr Surg. Aug 2022;57(8):1614-1621. doi:10.1016/j.jpedsurg.2022.03.015
34. Rasmussen B, Perry R, Hickey M, et al. Patient preferences using telehealth during the COVID-19 pandemic in four
Victorian tertiary hospital services. Intern Med J. May 2022;52(5):763-769. doi:10.1111/imj.15726
35. Ng BP, Park C, Silverman CL, Eckhoff DO, Guest JC, Díaz DA. Accessibility and utilisation of telehealth services among
older adults during COVID-19 pandemic in the United States. Health Soc Care Community. Sep 2022;30(5):e2657-e2669.
doi:10.1111/hsc.13709
36. Fischer SH, Predmore Z, Roth E, Uscher-Pines L, Baird M, Breslau J. Use Of And Willingness To Use Video Telehealth
Through The COVID-19 Pandemic. Health Aff (Millwood). Nov 2022;41(11):1645-1651. doi:10.1377/hlthaff.2022.00118
37. Odukoya EJ, Andino J, Ng S, Steppe E, Ellimoottil C. Predictors of Video versus Audio-Only Telehealth Use among
Urological Patients. Urol Pract. May 2022;9(3):198-204. doi:10.1097/upj.0000000000000301
38. Webber EC, McMillen BD, Willis DR. Health Care Disparities and Access to Video Visits Before and After the COVID-19
Pandemic: Findings from a Patient Survey in Primary Care. Telemed J E Health. Aug 27 2021;doi:10.1089/tmj.2021.0126

April 2023
ISSUE BRIEF
17
39. Shee K, Liu AW, Yarbrough C, Branagan L, Pierce L, Odisho AY. Identifying Barriers to Successful Completion of Video
Telemedicine Visits in Urology. Urology. Nov 2022;169:17-22. doi:10.1016/j.urology.2022.07.054
40. Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-
19 pandemic. JAMIA Open. Jul 2021;4(3):ooab056. doi:10.1093/jamiaopen/ooab056
41. Pasquinelli MM, Patel D, Nguyen R, et al. Age-based disparities in telehealth use in an urban, underserved population in
cancer and pulmonary clinics: A need for policy change. J Am Assoc Nurse Pract. May 1 2022;34(5):731-737.
doi:10.1097/jxx.0000000000000708
42. Chen J, Li KY, Andino J, et al. Predictors of Audio-Only Versus Video Telehealth Visits During the COVID-19 Pandemic. J
Gen Intern Med. Apr 2022;37(5):1138-1144. doi:10.1007/s11606-021-07172-y
43. Lori Uscher-Pines LS. Rethinking The Impact Of Audio-Only Visits On Health Equity. Health Affairs Forefront. DECEMBER
17, 2021 2021;doi:10.1377/forefront.20211215.549778
44. Baughman DJ, Jabbarpour Y, Westfall JM, et al. Comparison of Quality Performance Measures for Patients Receiving In-
Person vs Telemedicine Primary Care in a Large Integrated Health System. JAMA Netw Open. Sep 1 2022;5(9):e2233267.
doi:10.1001/jamanetworkopen.2022.33267
45. Gately ME, Quach ED, Shirk SD, Trudeau SA. Understanding Variation in Adoption of Video Telehealth and Implications
for Health Care Systems. Med Res Arch. Jun 1 2022;10(5)doi:10.18103/mra.v10i5.2751
46. Connolly SL, Miller CJ, Gifford AL, Charness ME. Perceptions and Use of Telehealth Among Mental Health, Primary, and
Specialty Care Clinicians During the COVID-19 Pandemic. JAMA Netw Open. Jun 1 2022;5(6):e2216401.
doi:10.1001/jamanetworkopen.2022.16401
47. Hsueh L, Huang J, Millman AK, et al. Disparities in Use of Video Telemedicine Among Patients With Limited English
Proficiency During the COVID-19 Pandemic. JAMA Netw Open. Nov 1 2021;4(11):e2133129.
doi:10.1001/jamanetworkopen.2021.33129
48. Marsh Z, Teegala Y, Cotter V. Improving diabetes care of community-dwelling underserved older adults. J Am Assoc
Nurse Pract. Oct 1 2022;34(10):1156-1166. doi:10.1097/jxx.0000000000000773
49. Mechanic OJ, Lee EM, Sheehan HM, et al. Evaluation of Telehealth Visit Attendance After Implementation of a Patient
Navigator Program. JAMA Netw Open. Dec 1 2022;5(12):e2245615. doi:10.1001/jamanetworkopen.2022.45615
50. O'Shea AMJ, Baum A, Haraldsson B, et al. Association of Adequacy of Broadband Internet Service With Access to Primary
Care in the Veterans Health Administration Before and During the COVID-19 Pandemic. JAMA Netw Open. Oct 3
2022;5(10):e2236524. doi:10.1001/jamanetworkopen.2022.36524
51. Infrastructure Investment and Jobs Act, Public Law 117-58 (Rep. DeFazio PA 2021). November 15, 2021. Accessed
October 12, 2022. https://www.congress.gov/bill/117th-congress/house-bill/3684
52. National Telecommunications and Information Administration. NTIA’s Role in Implementing the Broadband Provisions of
the 2021 Infrastructure Investment and Jobs Act. Accessed October 12, 2022,
https://broadbandusa.ntia.doc.gov/news/latest-news/ntias-role-implementing-broadband-provisions-2021-
infrastructure-investment-and
53. National Telecommunications and Information Administration. Grants: Infrastructure Investment and Jobs Act
Overview. Accessed November 6, 2022, https://www.ntia.doc.gov/category/grants
54. Tang M, Chernew ME, Mehrotra A. How Emerging Telehealth Models Challenge Policymaking. Milbank Q. Sep 28
2022;doi:10.1111/1468-0009.12584
April 2023
ISSUE BRIEF
18
APPENDIX
Appendix exhibit 1. Table of telehealth utilization percentage (%) from each HPS survey period weeks 28-48 (April
2021 – August 2022)
DATES
Adults
Children
Apr 14 – Apr 26, 2021
26.9
24.1
Apr 28 – May 10, 2021
26.1
23.4
May 12 – May 24, 2021
25.9
23.2
May 26 – Jun 7, 2021
25.3
22.7
Jun 9 – Jun 21, 2021
24.5
22.6
Jun 23 – Jul 5, 2021
24.6
22.1
Jul 21 – Aug 2, 2021
20.6
16.2
Aug 4 – Aug 16, 2021
20.2
15.3
Aug 18 – Aug 30, 2021
20.5
15.8
Sep 1 – Sep 13, 2021
20.6
16.5
Sept 15 – Sep 27, 2021
20.9
16.5
Sep 29 – Oct 11, 2021
20.9
16.8
Dec 1 – Dec 13, 2021
19.7
15.8
Dec 29 – Jan 10, 2022
20.2
16.2
Jan 26 – Feb 7, 2022
22.0
16.4
Mar 2 – Mar 14, 2022
21.2
15.9
Mar 30 – Apr 11, 2022
20.7
15.2
Apr 27 - May 9, 2022
20.5
15.1
Jun 1 - Jun 13, 2022
24.1
16.7
Jun 29 - Jul 11, 2022
24.2
16.0
Jul 27 - Aug 8, 2022
22.8
15.5

April 2023
ISSUE BRIEF
19
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
Office of the Assistant Secretary for Planning and Evaluation
200 Independence Avenue SW, Mailstop 447D
Washington, D.C. 20201
For more ASPE briefs and other publications, visit:
aspe.hhs.gov/reports
ABOUT THE AUTHORS
Euny C. Lee is a Social Science Analyst in the Office of Health Policy at ASPE.
Violanda Grigorescu is a Senior Health Scientist in the Office of Health Policy at ASPE.
Idia Enogieru is an ORISE Fellow in the Office of Health Policy at ASPE.
Scott R. Smith is the Division Director in the Office of Health Policy at ASPE.
Lok Wong Samson is a Health Policy Analyst in the Office of Health Policy at ASPE.
Ann B. Conmy is a Social Science Analyst in the Office of Health Policy at ASPE.
Nancy De Lew is the Acting Deputy Assistant Secretary, Health Policy, at ASPE.
SUGGESTED CITATION
Lee, E.C., Grigorescu, V., Enogieru, I., Smith, S.R., Samson, L.W., Conmy, A., De Lew,
N. Updated National Survey Trends in Telehealth Utilization and Modality: 2021-
2022 (Issue Brief No. HP-2023-09). Office of the Assistant Secretary for Planning
and Evaluation, U. S. Department of Health and Human Services. April 2023.
COPYRIGHT INFORMATION
All material appearing in this report is in the public domain
and may be reproduced or copied without permission;
citation as to source, however, is appreciated.
DISCLOSURE
This communication was printed, published, or produced and
disseminated at U.S. taxpayer expense.
___________________________________
Subscribe to ASPE mailing list to receive
email updates on new publications:
https://list.nih.gov/cgi-bin/wa.exe?SUBED1=ASPE-HEALTH-POLICY&A=1
For general questions or general
information about ASPE:
aspe.hhs.gov/about
HP-2023-09
