
Patient-Centered Education in Wound Management:
Improving Outcomes and Adherence
Lynelle F. Callender, DNP, RN, Vice Chair, Nursing Online, Advent Health University, Orlando, Florida
Arlene L. Johnson, DNP, RN, Coordinator, Nurse Practitioner Program, Advent Health University, Orlando, Florida
Rose M. Pignataro, PhD, DPT, PT, CWS, CHES, Associate Professor, Assistant Director, Physical Therapy Program, Emory & Henry College, Marion, Virginia
CME
1 AMA PRA
Category 1 Credit
TM
ANCC
2.5 Contact Hours
GENERAL PURPOSE: To educate wound care practitioners about methods of communication that can help promote patient adherence
to wound healing recommendations.
TARGET AUDIENCE: This continuing education activity is intended for physicians, physician assistants, nurse practitioners, and nurses
with an interest in skin and wound care.
LEARNING OBJECTIVES/OUTCOMES: After participating in this educational activity, the participant will:
1. Distinguish the use of theoretical frameworks to promote patient adherence to prescribed wound healing recommendations.
2. Synthesize the principles of motivational interviewing to best encourage patients to adhere to prescribed wound healing
recommendations.
3. Select the appropriate self-care strategies for patients who have nonhealing wounds.
ABSTRACT
Patients with chronic wounds make daily decisions that affect
healing and treatment outcomes. Patient-centered education
for effective self-management decreases episodes of care
and reduces health expenditures while promoting
independence. Theoretical frameworks, including the Health
Belief Model, Theory of Planned Behavior, Social Cognitive
Theory, and Transtheoretical Model of Behavior Change, can
assist healthcare providers in identifying strategies that
enhance adherence. These strategies include the use of
motivational interviewing, a communication technique
designed to elicit patients’ perspectives regarding treatment
goals, outcome expectations, anticipated barriers, and
intentions to follow provider recommendations.
KEYWORDS: barriers, chronic wounds, education,
health behavior theory, patient outcomes,
wound management, wound healing
ADV SKIN WOUND CARE 2021;34:403–10.
DOI: 10.1097/01.ASW.0000753256.29578.6c
INTRODUCTION
Patients’ daily decisions and activities have a significant
impact on wound healing outcomes independent of the
healthcare provider.
1
Therefore, patient-centered educa-
tion for effective self-management is an essential compo-
nent of the plan of care.
2
Instrumental self-management
skills include wound cleansing, dressing changes, and
recognizing signs and symptoms of infection.
3
An under-
standing of theoretical frameworks and evidence-based
approaches to patient-centered education can assist wound
care practitioners in promoting patient adherence. The
World Health Organization defines adherence as “the extent
to which a person’sbehavior—taking medication, following
a diet, and/or executing lifestyle changes—corresponds
with agreed recommendations from the healthcare pro-
vider.”
4
It is important to note that adherence is not the
same as compliance. The term “adherence ” implies col-
laboration, in which patients actively choose to follow
the provider’s advice based on shared responsibility
for health outcomes, as opposed to “compliance,” which
connotes submission to provider directives.
5
Effective education and enhanced adherence decrease
episodes of car e, reduce health expenditur es, and prevent
serious complications.
3,6
Impediments to adherence en-
compass provider characteristics as well as patient character-
istics. Among providers, barriers include anticipated patient
nonadherence, perceived lack of education ef f ec t iv en es s,
The authors, faculty, staff, and planners in any position to control the content of this CME/NCPD activity have disclosed that they have no financial relationships with, or financial
interests in, any commercial companies relevant to this educational activity. To earn CME credit, you must read the CME article and complete the quiz online, answering at least 7 of
the 10 questions correctly. This continuing educational activity will expire for physicians on July 31, 2023, and for nurses June 7, 2024. All tests are now online only; take the test at
http://cme.lww.com for physicians and http://www.NursingCenter.com/CE/ASWC for nurses. Complete NCPD/CME information is on the last page of this article.
Clinical Management Extra
WWW.ASWCJOURNAL.COM 403 ADVANCES IN SKIN & WOUND CARE • AUGUST 2021
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
insufficient training in patient-centered education tech-
niques,
1,7
and time constraints within the clinical envi-
ronment.
1
Many providers are also hesitant to discuss
patients’ personal behaviors for fear of provoking defen-
siveness or damaging rapport.
2,7
Application of theoretical
frameworks assists providers in selecting communica-
tion techniques that incorporate patie nts ’ perspectives
to ove rcome barr iers to quality wound care.
THEORETICAL FRAMEWORKS FOR PATIENT-CENTERED
EDUCATION
Health Belief Model
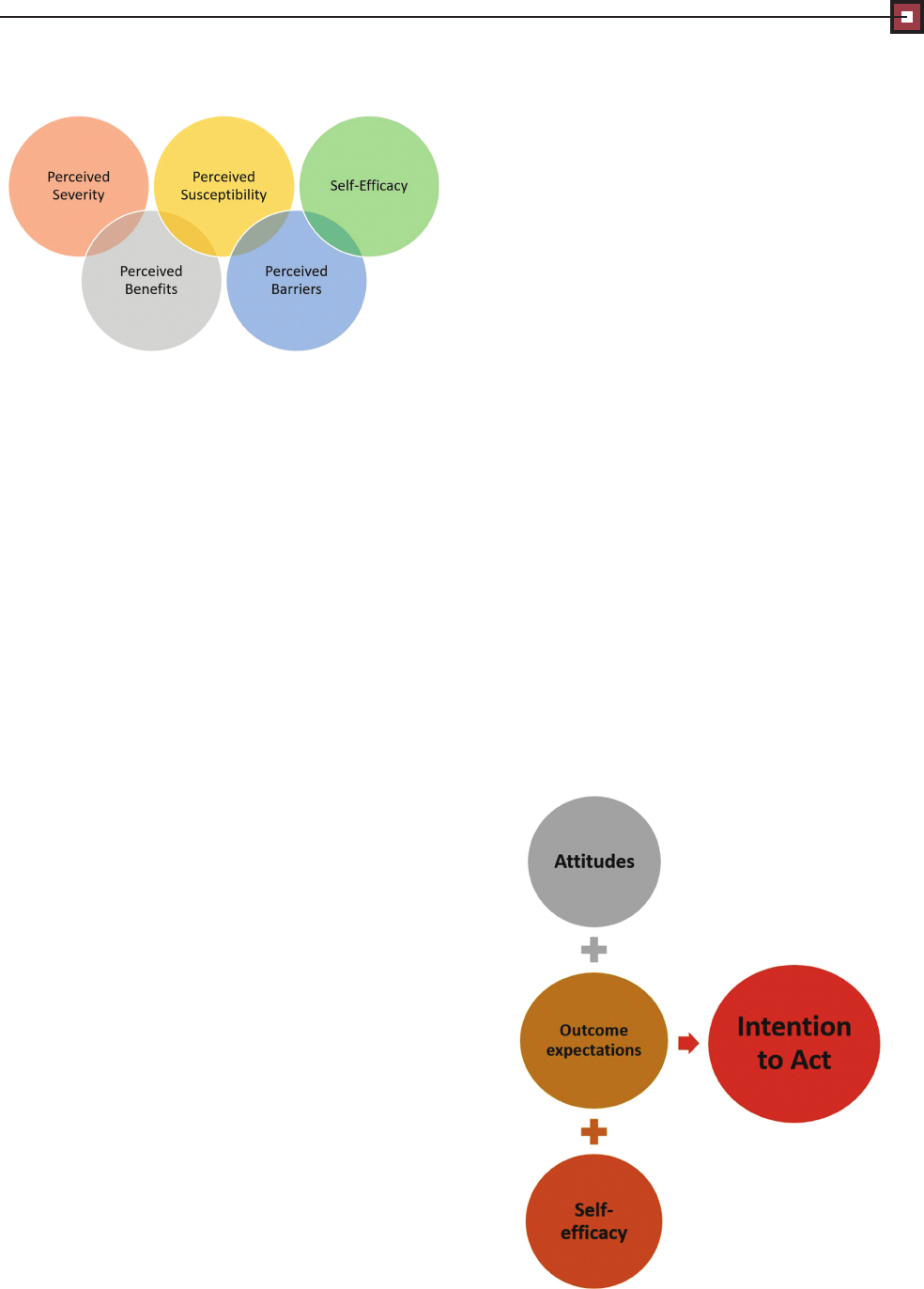
The Health Belief Model (HBM) describes factors that in-
fluence patient adherence, such as perceptions of health
risk severity, negative health outcomes, and the benefits
of recommended health behaviors.
2
The HBM also in-
corporates self-efficacy, or patient belief in their ability
to successfully enact provider recommendations and
achieve intended goals. Providers can apply the HBM
to discuss patients’ personal risks and benefits of action.
Using the HBM also helps providers understand patient
barriers to enacting treatment recommendations, includ-
ing patients’ confidence in their ability to self-manage
their condition (Figure 1).
Theory of Planned Behavior
According to the Theory of Planned Behavior (TPB), ad-
herence is primarily determined by behavioral inten-
tions. Factors that shape intentions include patients’
attitudes toward provider recommendations, as well as
outcome expectations, or the a nticipated results o f
adherence.
8
Like the HBM, the TPB also includes
self-efficacy.
2
Low self-efficacy diminishes adherence even
when patients strongly value the outcome.
8
Providers
can apply the TPB to investigate and address factors that
influence self-efficacy and outcome expectations. These
factors include personality, age, gender, education level,
health literacy, socioeconomic status, and learning pref-
erences
8
(Figure 2).
Social Cognitive Theory
Like the HBM and TPB, Social Cognitive Theory (SCT)
stresses the importance of self-efficacy. Wound care pro-
viders can apply SCT to build self-efficacy and match the
benefits of treatment recommendations with the patient’s
personal goals.
2
Long-term adherence also requires that
the patient have knowledge, skills, and the ability to
self-assess and respond to changes in their condition.
9
These changes may include signs of infection, delayed
healing, and the need for further consultation.
Transtheoretical Model of Behavior Change
The Transtheoretical Model (TTM)
2
describes patients’
readiness to engage in health behaviors:
(1) Precontemplation is when patients are not consid-
ering change. This may be attributable to a lack of
awareness, low perceived importance, or low desire to
engage in recommended health behaviors.
(2) Contemplation occurs when patients begin thinking
about adherence, or recommitment to adherence, if a
lapse in behavior has occurred.
(3) Preparation is when patients are taking steps toward
initiating adherence within the next 2 weeks.
(4) Action is when the person has initiated and is engaged
in adherence.
(5) Maintenance occurs when adherence is sustained for
at least 6 months.
Patients do not always progress through the stages of
change in a linear, predictable pattern. Some may lapse
Figure 1. HEALTH BELIEF MODEL
Figure 2. THEORY OF PLANNED BEHAVIOR
ADVANCES IN SKIN & WOUND CARE • AUGUST 2021 404 WWW.ASWCJOURNAL.COM
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.

into earlier stages when met with challenges. Even after
maintenance, relapse can occur despite temporary suc-
cess.
2
Provid ers can promote adherence by tailoring educa-
tion interventions to match patients’ readiness to change
(Figure 3).
PATIENT-CENTERED COMMUNICATION TECHNIQUES
Motivational interviewing (MI) is a patient-centered
communication technique designed to help patients rec-
ognize discrepancies between nonadherence and desired
treatment outcomes.
10
Providers can use this technique
to encourage patients to prioritize outcomes based on their
personal values. Further, MI enables providers and pa-
tients to collaboratively decide which recommendations
work best given patients’ lifestyle, prefer ences, and avail-
able resources.
11
During MI, providers ask open-ended
questions to gain insight into patient intentions, abilities,
and willingness to adhere to treatment recommenda-
tions.
12
Then, providers use these insights to create individu-
alized goals and tailored wound management strategies.
Wound care providers can also promote adherence by
tracking goals and acknowledging patients’ accomplish-
ments.
2
Setting small, incremental goals promotes
gradual increases in patient self-efficacy.
13
These g oals
should be SMART (specific, measurable, achievable,
relevant, and timely); otherwise, lack of attainment
can discourage adherence.
2
In addition, it is important for
patients and providers to discuss potential challenges and
collaboratively identify strategies to pr event behavioral
lapses.
2
Scheduled follow-ups help affirm positive results
and provide an opportunity to review any unexpected bar-
riers to adherence.
13
Discussing barriers helps patients
maintain positive health behaviors, strengthen commit-
ment, and identify new strategies when necessary.
13
There are two basic phases in MI: (1) eliciting “change
talk,” that is, desire, reasons, and ability to change; and
(2) p romoting commitm ent to new beh aviors.
10
The
mnemonic OARS (open-ended questions, affirmations,
reflective listening, and summarization) describes com-
munication techniques commonly used in MI. Open-
ended questions inspire introspection regarding the pros
and cons of provider recommendations and facilitate
adherence. Affirmations foster confidence in patient
ability t o engage in effective self-care and achieve
positive outcomes. Reflective listening clarifies pa-
tients’ intentions and meaning and allows providers
to emphasize positive decisional balance, including
the patients’ expressed need for adherence, potential
benefits, and ability to succeed. Summarization is a tech-
nique providers can use to wrap up the conversation or
transition to a new topic by reviewing important points
and confirming patients’ understanding and agreement
with the recommendations.
14
Frameworks to assist providers in implementing MI
include the “5As” and “5Rs.”
1
During initial conversa-
tions with patients, providers can apply the “5As:”
1
(1) Ask patients about self-care.
(2) Advise patients about the risks of nonadherence.
(3) Assess patient readiness to follow recommendations.
(4) Assist patients in creating goals and plans to imple-
ment recommendations.
(5) Arrange for follow-up support.
If patients are not yet ready to engage in recommended
health behaviors, providers can use the “5Rs:”
1
(1) Discuss the relevance of the recommendations within
the context of patient goals.
(2) Guide patients to consider risks of nonadherence.
(3) Suggest possible rewards or positive outcomes.
(4)Invite patients to share anticipated roadblocks or bar-
riers to adherence.
(5) Repetition: revisit topics during future conversations
to negotiate a healthy course of action.
When using MI, providers should respect patient auton-
omy. Acknowledging patients’ right to self-determination
reduces the likelihood of resistance and defensiveness. By
expressing empathy toward patient challenges and invit-
ing opposing viewpoints, providers can promote patient
ownership and control of their own health.
10
Time constraints are one of the greatest barriers to ap-
plying MI within clinical settings.
15
The pressures of a
busy schedule can restrict provider ability to engage in
detailed conversations with patients. Although tradi-
tional MI requires 30 to 60 minutes, brief MI can take
as little as 5 to 10 minutes.
10
Brief MI focuses on a single
goal. Once the patient and provider select this goal, the
provider can use MI techniques to guide the conversa-
tion toward specific steps designed to achieve the desired
outcomes. Conversations should focus on the following
Figure 3. TRANSTHEORETICAL MODEL OF BEHAVIOR CHANGE
WWW.ASWCJOURNAL.COM 405 ADVANCES IN SKIN & WOUND CARE • AUGUST 2021
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.

aspects: what actions patients should perform and what
is an acceptable degree of adherence (eg, how often or
how much adherence is required).
Communication throughout the course of treatment allows
providers to continue to reinforce patients’ motivations. For
patients who are not ready to follow recommendations, fur-
ther discussion of their concerns and perceived barriers
may be necessary. Often, past failures and challenges can de-
crease patient confidence and ability to engage in appropriate
self-care. Providers can help patients reframe failed attempts
as opportunities to learn about ineffective approaches to
adherence while identifying suitable alternatives.
Once an agreement has been reached, a written action
plan promotes adherence. As part of the plan, providers
should encourage patients to discuss feasibility and use-
fulness of the treatment recommendations.
15
The plan
should also include scheduled follow-ups in person, by
phone, and/or electronic communication.
16
Finally, providers must remember that nonadherence
can be intentional or unintentional.
17
Reasons for inten-
tional nonadherence include pain and patients’ percep-
tions regarding the feasibility and effectiveness of treatment
recommendations, as well as insufficient explanations
from clinicians regarding the rationale supporting recom-
mendations.
17
PATIENT EDUCATION
Effective patient education involves three essential com-
ponents: self-care skills, how to recognize and respond
to problems, and preventive management. Patients’ un-
derstanding of the healing process may also greatly im-
prove wound outcomes.
18
For example, patients may
not understand that wounds should heal from the base
to the surface. It is also important that patients can distinguish
“good” versus “bad” tissue. Pictures may help patients iden-
tify how “good” tissue should look as their wound begins to
heal. Healthy granulation tissue has a red, glossy appearance.
In contrast, necrotic tissue is tan, yellow, or black.
18
Providers
should also advise patients that drainage should decrease
as healing progresses
18
and “normal” drainage de-
pends on the color, consistency, amount, and odor.
Other essential self-care skills include proper hand-
washing, wound cleansing, and dressing changes. Pro-
viders should discuss appropriate cleansing solutions
and caution patients to avoid irritating or cytotoxic sub-
stances. Using the wrong cleanser may delay healing.
18
Further, many people believe that a dry wound prevents
infection; providers should proactively educate patients
and caregivers about moist wound healing. Providers
should encourage patients to seek follow-up if the wound
becomes too dry so that they can discuss the need for a
different type of dressing.
Patients and caregivers also need education on how and
when to replace dressings.
18
During each dressing change,
wounds should be cleaned and assessed.
18
Providers should
review signs and symptoms of infection so that patients and
caregiver s can seek timely medical attention.
18
Adverse
changes include increased pain or tenderness, increased exu-
date, changes in the type of exudate (eg, pus versus serous
drainage), swelling, heat, periwound discoloration, and foul
odor.
18
Patients and caregivers should also be aware of sys-
temic symptoms of infection, such as fever , chills, nausea,
and malaise.
18
Pain may interfere with patient ability and
willingness to clean wounds and change dressings.
3
There-
fore, providers may initiate patient and caregiver train-
ing in analgesic interventions, such as topical agents
and/or nonadherent dressings.
3
Ideally, providers should supplement verbal instruc-
tion with written material and demonstration.
3
Consis-
tent with theoretical frameworks for health behavior
change, providers should tailor instruction to match pa-
tients’ health literacy, language, culture, and specific
concerns. Treatment outcomes are improved when pro-
viders emphasize the relevance of the information based
on patient goals. Personalized education enhances ad-
herence, patient satisfaction, and wound healing.
3
Providers should also consider patient perceptions
that pose potential challenges to adherence. Important
factors include:
18
(1) What are patients’ beliefs regarding the cause of the
wound?
(2) What are the effects of the wound on quality of life,
ability to perform activities of daily living, and so on?
(3) What is the perceived severity of the wound? How
long do patients think it will take for their wound to
heal?
(4) How do patients think their wounds should be treated?
(5) What are the most important treatment results pa-
tients hope to achieve?
(6) What fears do patients have regard ing wound treatment?
Nutrition
Education concerning specialized nutrition requirements
is particularly important for patients with underlying
comorbidities, such as diabetes, renal disease, anemia,
or difficulty eating.
19
Dietary advice and information
concerning the use of supplements can enhance patients’
sense of control over the wound healing process.
Nutritional impediments to healing include inadequate
protein and carbohydrate intake.
19
Supplements, such
as vitamins A, C, D, and E, and minerals, such as zinc,
copper, selenium, and folic acid, may also be prescribed.
19
Prevention and Treatment of Pressure Injuries
Patients with mobility and/or sensory impairments have
an elevated risk of pressure injuries (PIs). Patient educa-
tion on skin protection, t urning and positioning, and
notifying caregivers about tender and painf ul areas
ADVANCES IN SKIN & WOUND CARE • AUGUST 2021 406 WWW.ASWCJOURNAL.COM
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.

increases autonomy by enabling patients to self-advocate
and supervise appropriate treatment interventions, even
when caregiver assistance is required to carry out provider
recommendations.
20
Patients and caregivers should be
aware of common PI locations (heels, sacrum, ischium,
and greater tuberosity), as well as intrinsic and extrinsic
factors that increase vulnerability and delayed healing,
such as incontinence and localized skin trauma.
21,22
Pa-
tients can decrease their vulnerability to tissue damage
using specialized support surfaces and strategies for po-
sitioning and pressure redistribution.
21,22
These strate-
gies should include keeping the head of the bed at or
below 30° whenever possible to decrease friction and
shear.
21
Depending on their physical abilities, patients
may be taught how to use assistive devices, such as an
overhead trapeze and/or grab bars, to perform reposi-
tioning.
23
Information regarding the characteristics of
an ideal support surface also helps equip patients to en-
sure optimal prevention and treatment.
23
Providers should also educate patients on skin assess-
ment and signs of impending damage. Even if patients
are reliant on caregivers to examine their skin, the ability
to recognize problems and seek appropriate treatment
fosters independence.
23
In addition, patients and care-
giversoftenrequireinstructionregardingproperhygiene
and skin care.
23
As with other types of chronic wo u nds ,
patients with PIs benefit from education regar ding behav-
ioral risks, such as tobacco use, nutrition, hydration, ex-
ercise, and medication adherence.
23
Peripheral Arterial Disease and Treatment of Arterial Ulcers
Patients with peripheral arterial disease often underesti-
mate their risk of serious complications.
24
This may stem
from lack of knowledge or denial about the impact of
nonadherence.
24
Providers can address these issues by
reviewing factors that mitigate risks, such as tobacco cessa-
tion, exercise, and proper diet.
25
Further, providers should en-
courage patients to engage in proper self-management of
common comorbidities, such as hypertension and type
2diabetes.
25
Adherence and self-care can be enhanced
by teaching patients how to interpret their own test re-
sults (eg, total cholesterol and total triglycerides).
25
Depending on the severity of circulatory insufficiency,
it may be best to keep arterial wounds dry pending re-
vascularization. This is an exception to typical patient
education regarding moist wound healing. Providers
should explain that ischemic ulcers often involve thick,
black, leathery eschar so that patients are not tempted
to soak the wound.
25
Prevention and Treatment of Venous Leg Ulcers
One of the most damaging aspects of venous insufficiency
is venous hypertension and lower extremity swelling.
Therefore, patient education should be directed toward
strategies that promote venous return and reduce edema.
These strategies often include the use of compression stock-
ings, which patients should don immediately upon waking
when limb volume is at its lowest. Applying stockings before
placing the legs in a dependent position tends to be the most
beneficial.
18
As part of self-management, patients should
avoid crossing their legs or keeping their legs in a dependent
position for prolonged periods. Instead, patients should ele-
vate their legs above the level of the heart at various intervals
througho ut the day.
18
Because most lower extremity venous return results
from muscle activity, exercises, such as walking and an-
kle pumps, are very helpful.
18
Providers should tailor
exercise recommendations to patients’ individual fitness
levels and any physical impairments. In addition, exercise
may assist patients with weight management,
18
because
obesity also impedes venous return.
Patients with venous insufficiency often need advice
about strategies to protect against inadvertent lower
extremity trauma, dermatitis, and ulceration.
26
Effective
prevention includes the use of appropriate footwear,
18
skin cleansers, and topical agents.
26
Additional steps that
patients can take to prevent or reduce venous insufficiency
and risk of ulceration include tobacco cessation.
26
Prevention and Treatment of Diabetic/Neuropathic Foot Ulcers
In patients with peripheral neuropathy, the loss of pro-
tective sensation is a primary risk factor for wounds
and delayed healing. Therefore, protective interventions
are critical. Patients should be empowered to perform
proper foot care, including choosing socks and shoes
that prevent compression, friction, and shear.
18
Through-
out the day, patients should remove their shoes and socks
to inspect the skin for any signs of redness or irritation.
18
Timing for self-checks should be based on individual
risks. When “break ing in” new shoes, self-checks should
occur at least every 2 hours.
18
Because most neuropathic ulcers occur on the plantar
aspect of the foot, treatment for existing wounds often
includes the use of offloading devices to redistribute
pressure. Providers and patients should discuss barriers
to adherence, including low perceived susceptibility and
severity. This is exacerbated by sensory deficits that re-
sult in low or absent pain signals despite the presence
of significant integumentary damage. Wearing shoes or
slippers with closed backs and nonskid soles, even when
ambulating short distances within the home, reduces the
likelihood of inadvertent trauma. If an offloading device
is used, it must be donned whenever the patient is weight-
bearing, even if the patient is only going from the bed to
the bathroom in the middle of the night.
Treatment outcomes for neuropathic ulcers are also
heavily dependent on patients’ adherence to nutrition
recommendations, blood glucose monitoring, physical
WWW.ASWCJOURNAL.COM 407 ADVANCES IN SKIN & WOUND CARE • AUGUST 2021
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.

activity, and weight management.
27
Patient education
that includes explicit steps for diet and exercise is more
likely to achieve success than generic recommendations.
27
Self-management is influenced by patients’ cognitive
understanding, motivation level, and ability to trouble-
shoot problems and barriers.
27
In patients with diabetes,
low perceived severity of illness and its consequences may
be influenced by family history and assumptions that dia-
betesisanaturalpartofgeneticsand/oraging.
27
These as-
sumptions can reduce outcome expectations and
self-efficacy by creating the impression that diabetes and
its consequences are unavoidable.
27
Patients and pro-
viders should discuss these perceptions and promote
skills that enhance self-care, including the ability to trou-
bleshoot unanticipated problems and barriers.
27
Other
barriers to adherence may include the lack of measur-
able results for patients who are adherent yet still expe-
rience disease progression.
27
These barriers can be
mitigated by social-environmental support from family,
friends, and community resources.
28
From a cognitive perspective, the ability to record and
interpret glucose measurements, calculate medication
doses, and read nutrition labels requires a certain level of lit-
eracy and mathematical skill.
27
Providers should also assist
patients in understanding the differ ence between test results
that show immediate glycemic control (plasma glucose
level) versus long-range control (hemoglobin A
1c
;Table1).
27
CASE REPORT
Mrs H. (fictional patient) is a 60-year-old catering chef re-
ferred for outpatient wound management secondary to
a nonhealing ulcer on the plantar aspect of her left foot.
The wound has been present for more than 19 weeks
and has increased in depth since onset. Clinical presentation
includes peripheral neuropathy with loss of protective
sensation, poor glycemic management, and a history of
tobacco use and sedentary lifestyle.
The patient is experiencing barriers to performing prior
recommendations for wound cleansing, use of a hydrogel
dressing, and left non-weight-bearing using a knee scooter.
The following represents a dialogue between Mrs H. and
her doctor of physical therapy (DPT)/certified wound
management specialist. The conversation exemplifies the
use of MI techniques and theoretical frameworks.
DPT: Mrs H., thank you for agreeing to meet with me
to discuss your plan of care. I understand that you are
concerned about the lack of healing in your foot. I agree
that we need to talk about what we can change to make
sure that your wound improves.
Mrs H.:Ijustdon’t see the point in coming here. This
wound keeps getting bigger no matter what I do.
DPT: I am sure that must be very frustrating for you. I
see that you are not using the knee scooter today. Are
you having trouble with it?
Mrs H.: It makes my other leg very tired, and my back
gets sore.
DPT: Thank you for telling me. We certainly don’twant
to cause any other problems for you. We can definitely
talk about some other ideas besides the scooter. First,
can you tell me about some of the things you have been
doing at home in between visits?
Mrs H.: Well, my husband helps me take the ban-
dage off so that I can soak my foot every night. I make
sure I dry it really well, and then we put a new piece
of gauze on it.
DPT: What type of shoes have you been wearing?
Mrs H.: I usually wear these plastic clogs because they
are easy to slip on and off.
DPT: Because this wound is on the bottom of your
foot, one of the things that could help it heal is to take
some of the pressure off the area with a special walking
boot. Is that something you might be interested in?
Mrs H.: Well, it w ould d epend on how hard it is to
get the boot on by myself. My husband leaves for work
before I get dressed in the morning, and it’shardforme
to bend.
DPT: Well, the type of boot I am thinking of slides on
and closes with Velcro. Can we try one on to see what
you think? [produces walking boot]
Mrs H.: Oh man, that thing looks bulky and heavy.
DPT: It is kind of bulky, but I think you have enough
strength and balance to move around using the boot. It
may not be as heavy as you think. [Hands Mrs H. the walk-
ing boot]
Mrs H.: [makes a face and shakes her head] I think I
would rather stick with my clogs.
DPT: Would it be all right if I explained a little more
about why I think the walking boot will be so helpful?
Table 1. ESSENTIAL SELF-MANAGEMENT KNOWLEDGE
AND SKILLS
• Cause of the wound and contributing factors
• Anticipated healing time
• Moist wound healing principles (assuming there is adequate blood
supply for healing)
• Characteristics of a healthy wound bed
• Wound cleansing techniques and timing
• How and when to change wound dressing
• Signs and symptoms that indicate need for urgent medical attention
• Guidelines and techniques for treating the wound cause (eg, turning,
positioning, and pressure redistribution for pressure injuries)
• Activity modifications and rationales
• How to monitor and manage comorbidities
• Medication dosing and reason for each medication
• Nutrition recommendations, including proper hydration
ADVANCES IN SKIN & WOUND CARE • AUGUST 2021 408 WWW.ASWCJOURNAL.COM
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.

If you still don’t agree, I will respect your decision. I just
want you to have all the necessary information to make
good choices.
Mrs H.: [sighs] OK, I am listening.
DPT: Imagine you cut your finger here on the knuckle
while you were working in the kitchen. Every time you bend
your finger , it puts strain on that cut and stops it from healing.
What’s happening now with your foot is that every time you
stand or walk, it puts the same type of strain on the wound
and makes it harder for the body to repair it.
Mrs H.: That makes sense, but I can’t sit around and
put my feet up. I need to stand and walk to do my job,
and we can’t afford to have me out of work.
DPT: I understand that would be very difficult. In-
stead of having you stay out of work, this walking boot
would help redistribute the pressure on the bottom of
your foot while the wound is healing. You could use it
to stand and move around the kitchen while you are fill-
ing your catering orders.
Mrs H.: OK, I am willing to try it.
DPT: Great! There are several dif ferent options for
redistributingthepressure.Thisisthetypeofbootweuse
with most of our patients, but if it isn’tcomfortable,oryou
have trouble putting it on or taking it off by yourself, I want
you to let us know so that we can work together to find
something else that will work for you. How does that sound?
Mrs H.: That sounds reasonable.
The conversation continues after a brief session of gait
training using the walking device/pressure redistribu-
tion boot:
DPT: What do you think of the boot now that we have
tried it out?
Mrs H.: It’s OK, but it looks ugly.
DPT: I agree, I don’t think we will be starting any fash-
ion trends with this one! On a serious note, how impor-
tant is the look of this boot compared with your ability to
continue to work while your foot heals? Do you think
you can make that compromise?
Mrs H.: Of course—I mean, we aren’t really dressing
for looks while we are working in the kitchen.
DPT: OK, great. For this to work, it will be important
for you to put it on whenever you are on your feet, even
if you are just going from the bed to the bathroom in the
morning when you first wake up. Aside from the ap-
pearance, is there anything else that might make it diffi-
cult for you to wear the walking boot?
Mrs H.: Well, I do feel a little uneven when I walk in
this thing, like one leg is longer than the other.
DPT: Good point; one leg is essentially longer than the
other because of the height difference between your clog
and the walking boot. Let’s have you put on the sneakers
you brought in when you came for your last visit. We
should be able to place a small lift inside your other shoe
to help make the height a little more even.
Mrs H.: I think that would really help. Is there any-
thing else we can do to help this stupid foot heal faster?
I am really getting tired of this.
DPT: Yes, there are definitely other changes we can
talk about. Because you are coming back in 2 days, let’s
see how the walking boot works for you first. Then, if you are
open to it, my recommendation would be for us to start
thinking about how you can improve your blood sugar
levels, which is another common barrier to healing.
Mrs H.: You’re not going to lecture me about losing
weight, are you?
DPT: I am not a big fan of lecturing another adult, but
it is something I would like to discuss. Just like every-
thing else we talk about, please let me know if you feel
like I am crossing the line, and I will back off.
Mrs H.: I really appreciate how you give me a say in
things. Thank you.
DPT: Thank you for trusting me and telling me what
you really think! If we are going to get this wound to
close, it’s very important that you and I work together
as a team. I will see you in a couple of days. Please call
if you have any questions in the meantime.
CONCLUSIONS
Providers can become frustrated by patient nonad-
herence and its effects on chronic wound outcomes.
Reexamining reasons for nonadherence enables providers
to respond productively.
18
Patients may feel overwhelmed
by the physical and psychological changes caused by
chronic wounds. Self-management can also feel over-
whelming because of the number and complexity of
treatment recommendations.
5
The likelihood of adherence is improved when clinicians
link recommendations to individual outcome expectations
and goals.
17
Despite patient willingness to follow recom-
mendations, unintentional nonadherence may still occur,
particularly if provider instructions are not clear.
18
Collab-
orative communication strategies, such as MI, can help
providers detect and address problems with comprehen-
sion or other unforeseen barriers. Providers should also
consider patient readiness to change. Successful wound
management often takes time, patience, and effort to de-
velop a deeper rapport before patients can adhere to
provider recommendations.
18
PRACTICE PEARLS
• Patient education on wound management skills,
such as cleansing, dressing changes, and recognizing
infection, can significantly improve treatment outcomes.
• A collaborative approach to wound prevention and
management also optimizes treatment outcomes.
• Theory-based assessment helps providers work with
patients to determine the patient’s readiness to change,
need for information, and perceived barriers to adherence.
WWW.ASWCJOURNAL.COM 409 ADVANCES IN SKIN & WOUND CARE • AUGUST 2021
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.

• Asking open-ended questions, such as in MI, allows
providers to better understand patient perspectives.
• Important questions to ask include: What caused this
wound?Howdoesthiswoundaffectyourday-to-day
life? How long do you think it will take for your wound
to heal? How do you think this wound should be
treated? What are the most important results
you hope to achieve with treatment? What fears
or concerns do you have about your treatment?
•
REFERENCES
1. Krist A, Tong S, Aycock R, Longo D. Engaging patients in decision-making and behavior change to
promote prevention. Stud Health Technol Inform 2017;240:284-302.
2. Allen C. Supporting effective lifestyle behavior change interventions. Nurs Stand 2014;28(24):51-8.
3. Chen Y, Wang Y, Chen W, Smith M, Huang H, Huang L. The effectiveness of a health education
intervention on self-care of traumatic wounds. J Clin Nurs 2013;22(17-18):2499-508.
4. World Health Organization. Adherence to long-term therapies: evidence for action. 2003. www.who.
int/chp/knowledge/publications/adherence_full_report.pdf. Last accessed April 28, 2021.
5. Price P. How can we improve adherence? Diabetes Metab Res Rev 2016;32(Suppl 1):201-5.
6. Chan L, Lai C. The effect of patient education with telephone follow-up on wound healing in adult
patients with clean wounds: a randomized controlled trial. J Wound Ostomy Continence Nurs 2014;
41(4):345-55.
7. Chisolm A, Hart J, Lam V, Peters S. Current challenges of behavior change talk for medical
professionals and trainees. Patient Educ Couns 2012;87(3):398-94.
8. Ajzen I. The Theory of Planned Behavior : reactio ns and reflections. Psychol Healt h 2011;
26(9):1113-27.
9. Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31(2):143-64.
10. Pignataro R, Huddleston J. The use of motivational interviewing in physical therapy education and
practice: empowering patients through effective self-management. J Phys Ther Educ 2015;29(2):62-71.
11. Miller W, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY:
Guilford Press; 2013.
12. Fisher L, Polonsky W, Hessler D, Potter M. A practical framework for encouraging and supporting
positive behavior change in diabetes. Diabet Med 2017;34(12):1658-66.
13. Greene J, Hibbard J, Alvarez C, Overton V. Supporting patient behavior change: approaches used by
primary care physicians whose patients have an increase in activation levels. Ann Fam Med 2016;
14(2):148-54.
14. Welch J. Building a foundation for brief motivational interviewing: communication to promote health
literacy and behavior change. J Contin Educ Nurs 2014;45(12):566-72.
15. Jerant A, Lichte M, Kravitz R, et al. Physician training in self-efficacy enhancing interviewing
techniques (SEE-IT): effects on patient psychological health behavior change mediators. Patient Educ
Couns 2016;99(11):1865-72.
16. Kivela K, Elo S, Kaariainen M. The effects of health coaching on adult patients with chronic diseases:
a systematic review. Patient Educ Couns 2014;97(2):147-57.
17. Moffatt C, Murray S, Keeley V, Aubeeluck A. Non-adherence to treatment of chronic wounds: patient
versus professional perspectives. Int Wound J 2017;14(6):1305-12.
18. London F. Teaching patients about wound care. Home Healthc Nurse 2007;25(8):497-500.
19. Green L, Ratcliffe D, Masters K, Story L. Educational intervention for nutrition education in patients
attending an outpatient wound care clinic: a feasibility study. J wound Ostomy Continence Nurs
2016;43(4):365-68.
20. Robineau S, Nicolas B, Mathieu L, et al. Assessing the impact of a patient education
programme on pressure ulcer prevention in patients with spinal cord injuries. J Tissue Viability
2019;28(4):167-72.
21. Wound, Ostomy and Continence Nurses Society—Wound Guidelines Task Force. WOCN 2016
guideline for prevention and management of pressure injuries (ulcers): an executive summary.
J Wound Ostomy Continence Nurs 2017;44(3):241-6.
22. Latimer S, Chaboyer W, Gillespie B. Patient participation in pressure injury prevention: giving patient’s
a voice. Scand J Caring Sci 2014;28(4):648-56.
23. McInnes E, Chaboyer W, Murray E, Allen T, Jones P. The role of patients in pressure injury
prevention: a survey of acute care patients. BMC Nurs 2014;13(1):41.
24. McDermott M, Mandapat A, Moates A, et al. Knowledge and attitudes regarding cardiovascular
disease risk and prevention in patients with coronary or peripheral arterial disease. Arch Intern Med
2003;163(18):2157-62.
25. Bonham P, Flemister B, Droste L, et al. 2014 guideline for management of wounds in patients with
lower-extremity arterial disease (LEAD): an executive summary. J Wound Ostomy Continence Nurs
2016;43(1):23-31.
26. Kelechi T, Johnson J, WOCN Society. Guideline for the management of wounds in patients with
lower-extremity venous disease: an executive summary. J Wound Ostomy Continence Nurs 2012;
39(6):598-606.
27. Aweko J, De Man J, Absetz P, et al. Patient and provider dilemmas of type 2 diabetes
self-management: a qualitative study in socioeconomically disadvantaged communities in Stocklolm.
Int J Environ Res Public Health 2018;15(9):1810.
28. King D, Glasgow R, Toobert D, et al. Self-efficacy, problem solving, and social-environmental support
are associated with diabetes self-management behaviors. Diabetes Care 2010;33(4):751-3.
For more th an 158 additional continuing professional development articles related to Skin and Wound Care topics,
go to NursingCenter.com/CE.
CME
Nursin
g
Continuin
g
Professional Develo
p
men
t
CONTINUING MEDICAL EDUCATION INFORMATION FOR PHYSICIANS
Lippincott Continuing Medical Education Institute, Inc., is accredited by the
Accreditation Council for Continuing Medical Education to provide
continuing medical education for physicians.
Lippincott Continuing Medical Education Institute, Inc., designates
this journal-based CME activity for a maximum of 1 AMA PRA Category
1Credit
TM
. Physicians should claim only the credit commensurate with
the extent of their participation in the activity.
PROVIDER ACCREDITATION INFORMATION FOR NURSES
Lippincott Professional Development will award 2.5 contact hours for this
continuing nursing education activity.
LPD is accredite d as a pro vider of nurs ing continui ng prof essional dev elopment
by the American Nurses Crede ntialing Center's Commission on A ccredit ation.
This activity is also provider approv ed by the California Board of Registered
Nursing, Provider Number CEP 11749 for 2.5 contact hours . LPD is also an
appro v ed provider of continuing nursing education by the District of Columbia,
Georgia, and Florida CE Brok er #50-1223. Your certificate is valid in all states.
OTHER HEALTH PROFESSIONALS
This activity provides ANCC credit for nurses and AMA PRA Category 1
Credit
TM
for MDs and DOs only. All other healthcare professionals
participating in this activity will receive a certificate of participation that
may be useful to your individual profession's CE requirements.
CONTINUING EDUCATION INSTRUCTIONS
• Read the article beginning on page 403. For nurses who wish to take the
test for NCPD contact hours, visit www.NursingCenter.com/ce/ASWC. For
physicians who wish to take the test for CME credit, visit http://cme.lww.
com. Under the Journal option, select Advances in Skin and Wound Care
and click on the title of the CE activity.
• You will need to register your personal CE Planner account before taking
online tests. Your planner will keep track of all your Lippincott Professional
Development online NCPD activities for you.
• There is only one correct answer for each question. A passing score for
this test is 7 correct answers. If you pass, you can print your certificate of
earned contact hours or credit and access the answer key. Nurses who fail
have the option of taking the test again at no additional cost. Only the first
entry sent by physicians will be accepted for credit.
Registration Deadline: July 31, 2023 (physicians); June 7, 2024 (nurses).
PAYMENT
The registration fee for this CE activity is $24.95 for nurses; $22.00 for
physicians.
ADVANCES IN SKIN & WOUND CARE • AUGUST 2021 410 WWW.ASWCJOURNAL.COM
Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved.
