
FINANCIAL RISKS DUE TO
LONG-TERM CARE
August 15, 2016
Constantijn W.A. Panis, PhD
Advanced Analytical Consulting Group, Inc.
213-784-6400
Michael J. Brien, PhD
Deloitte Transaction and Business Analytics LLP
202-378-5096

i
SUMMARY
This report characterizes the current landscape and outlook of long-term care
utilization, its costs, and its financing through out-of-pocket payments, private
insurance, and public insurance. We draw on academic and trade literature and
present new statistics based on primary research. In particular, we analyze cost
reports of skilled nursing facilities (SNFs), Form 5500 Annual Return/Report of
Employee Benefit Plan (“Form 5500”) filings, and the Health and Retirement Study
(HRS).
Approximately one-half of Baby Boomers are projected to require paid, formal long-
term care in the home, an adult day care center, an assisted living facility, or a
nursing home. Paying for care out of pocket will rapidly exhaust retirement savings
of many Americans, forcing them to eventually rely on Medicaid. Indeed, more than
one-half of nursing home patients who have been resident for five years or longer
are Medicaid beneficiaries. The size of the Baby Boom generation is expected to drive
up demand for and prices of long-term care, creating a troublesome outlook for the
elderly’s personal finances and the Medicaid program.
In light of the strained finances of Medicaid and other public payors, potential
solutions will likely involve expanded private insurance. At present, only about 7
million Americans are covered by long-term care insurance. We discuss several
options for reducing risks for insurers and consumers alike, public-private
partnerships which incentivize private insurance, and policy options to promote long-
term care insurance benefits in the workplace. However, fundamental economic
interactions between private insurance and the Medicaid program pose a challenge to
simultaneously preserving a safety net for low-income Americans and ensuring fiscal
sustainability of the Medicaid program.

ii
CONTENTS
Abbreviations ................................................................................................ ii
1. Introduction ............................................................................................. 3
2. Literature and External Statistics on Utilization and Costs ....................... 3
3. Cost Reports of Skilled Nursing Facilities ................................................. 9
4. Long-Term Care Insurance ..................................................................... 11
State Medicaid Partnership Programs .......................................................... 15
Employer-Provided Long-Term Care Benefits ................................................ 16
5. Analysis of Health and Retirement Study Data ....................................... 18
6. Policy Implications ................................................................................. 26
References .................................................................................................. 28
Appendix A. Median Prices of Long-Term Care Services, by State (2015) ... 31
Appendix B. Sample Long-Term Care Insurance policy ............................... 33
Disclaimer ................................................................................................... 37
ABBREVIATIONS
AALTCI American Association for Long-Term Care Insurance
ADL Activity of Daily Living
BLS Bureau of Labor Statistics
CBO Congressional Budget Office
CMS Centers for Medicare and Medicaid Services
HIPAA Health Insurance Portability and Accountability Act of 1996
HCRIS Healthcare Cost Report Information System
HRS Health and Retirement Study
IADL Instrumental Activity of Daily Living
LTC Long-term care
LTCI Long-term care insurance
LTSS Long-term services and support
NAIC National Association of Insurance Commissioners
NCHS National Center for Health Statistics
SNF Skilled Nursing Facility

3
1. INTRODUCTION
Caring for the elderly and the disabled in the United States is posing increasingly
large financial risks for patients, their family, and the Medicaid and Medicare
programs. Medical costs have outpaced general inflation over the past four decades
(BLS 2016) and retiring Baby Boomers are expected to increase demand for long-
term care (LTC) services.
This report documents long-term care utilization, costs, and financing mechanisms,
and reviews policy options for addressing long-term care’s financial risks. We draw
on a variety of sources including external literature and primary analyses of the cost
reports of skilled nursing facilities (SNFs), Form 5500 Annual Return/Report of
Employee Benefit Plan (“Form 5500”) filings, and the Health and Retirement Study
(HRS).
Mirroring the gradual increase in need for assistance as the body ages, long-term
care encompasses a range of services. Much of it is non-medical in nature, such as
assistance with cleaning, shopping, bathing, dressing, or eating. Services may be
provided in the home by relatives or friends, homemakers, or home health aides; at
adult day care centers; at assisted living facilities; at hospices, or at nursing homes.
1
Given the wide range of services, some authors refer to long-term care as long-term
services and support (LTSS). This document uses the two terms interchangeably.
The remainder of this report is organized as follows. Section 2 summarizes academic
and trade literature and provides external national statistics on long-term care
utilization and costs. Section 3 adds to these statistics from our own analysis of
annual cost reports that skilled nursing facilities (SNFs) submit to the Medicare
program of the Centers for Medicare and Medicaid Services (CMS). Section 4
discusses trends in long-term care insurance (LTCI) and its typical features. It also
includes our analysis of Form 5500 filings to shed a light on employer-sponsored
long-term care insurance. Section 5 presents our analysis of HRS data with respect
to long-term care utilization and its financial consequences. Section 6 concludes with
a discussion of policy implications.
2. LITERATURE AND EXTERNAL STATISTICS ON
UTILIZATION AND COSTS
In the United States, long-term care services are provided informally, by family and
friends, and formally, by about 12,200 home health agencies, 4,800 adult day
services centers, 22,200 assisted living and similar residential care communities,
15,700 nursing homes, and 3,700 hospices (NCHS 2013). On a typical day in 2011
or 2012 (NCHS 2013), approximately:
1
This document uses the terms Skilled Nursing Facility and nursing home
interchangeably. Some authors make a distinction, where SNFs are certified and
covered by Medicare and offer skilled medical and rehabilitative services, whereas
nursing homes offer custodial care. Typically, facilities offer both types of services.

4
4.7 million patients received services from home health agencies,
273,000 participants were enrolled in adult day services centers,
713,000 residents were living in residential care communities,
1.4 million residents were living in nursing homes, and
1.2 million patients received services from hospices.
Demand for LTC services in the United States is expected to grow substantially in the
coming decades, largely due to the aging of the population and increased prevalence
of disability among middle-aged populations. These factors increase the share of the
population that has functional limitations and may require assistance performing
everyday activities. The baby-boom generation, a cohort of 75 million individuals,
was born between 1946 and 1964. In 2016 the oldest baby-boomers are turning 70
years old, and by 2031, they will turn 85 years old. The aging of this generation is
causing significant shifts in the age distribution of the population (CBO 2013). In
2000, the share of the U.S. population that was 65 or older was 12%, but by 2050
that share is expected to exceed 20%. Over the same time period, the share of the
population age 85 or older is expected to grow from 1.5% to 4.1%. Functional
limitations and disability tend to increase with age. For example, from 2000 to 2010,
18% of 65-74 year olds living in the community reported difficulty performing
Activities of Daily Living (ADLs) or Instrumental Activities of Daily Living (IADLs),
while 54% of those aged 85 or older reported difficulties performing at least one of
these (CBO 2013).
2
Similarly, the Census Bureau (2012) found that, excluding those
in nursing homes, the fraction of people reporting needing assistance with activities
of daily living increased with age from 7% among 65-69 year-olds to 30% among
people age 80 or older (Table 1). As noted in their report, the magnitude of disability
estimates would likely be higher if the nursing home population were included.
Table 1. Disability Prevalence and the Need for Assistance among the Non-
Institutionalized Population by Age, 2010
2
ADLs include bathing, dressing, eating, walking, transferring out of a bed or a
chair, and using the toilet; IADLs include preparing meals, shopping, using the
telephone, managing money, and taking medications.
Age
Any
disability
Severe
disability
Needs
assistance
Under 15 8.4% 4.2% 0.5%
15 to 24 10.2% 5.3% 1.4%
25 to 44 11.0% 7.3% 2.0%
45 to 54 19.7% 13.8% 3.6%
55 to 64 28.7% 20.4% 6.0%
65 to 69 35.0% 24.7% 6.9%
70 to 74 42.6% 29.6% 10.8%
75 to 79 53.6% 37.5% 15.4%
80 and over 70.5% 55.8% 30.2%
Source: Census Bureau (2012). "Any disability"
indicates difficulty to perform ADLs/IADLs or similar
activities, and "severe disability" indicates inability
to perform such activities. For details see Figure 1 in
Census Bureau (2012).

5
While a general consensus has formed that the health of the elderly improved on
several measures throughout the 1980s and 1990s, there has been a surge in
disability among younger generations, in particular those under 50 years old
(Lakdawalla et al., 2003). While the root causes have not been fully investigated,
there is some evidence that obesity and such chronic illnesses as asthma and
diabetes may be part of the problem.
3
This will likely contribute to an even greater
increase in disability rates and institutionalization in a SNF in the coming decades
than as suggested by projected aging of the population. When analyzing cohorts
aged 65 and older in the late 1990s, Lakdawalla et al. (2004) forecast that the
younger cohorts will likely have a higher rate of disability at older ages than the
older cohorts did. This evidence aligns with increasing levels of disability among 50-
to 59-year olds between 1984 and 1996.
4
The aging of the population and the growth in disability among the middle-aged is
likely to lead to increased future demand for both informal and formal LTC services.
The Congressional Budget Office (CBO 2013) estimated that in 2011 the economic
value of informal and formal LTC services for elderly people in the United States was
$426 billion, of which $234 billion (55%) was in the form of informal care.
5
The
remaining $192 billion was spent on institutional care (31% of total) and community-
based care (14% of total).
6
While 31% of the total economic value was in
institutional care, it related to only 18% of elderly people who were receiving LTC
services in 2010. This reflects the high cost of institutional nursing care relative to
community-based care; see Table 4 below. Four-out-of-five (80%) of elderly people
who received LTC services lived in private homes, receiving informal care or
community-based care in the form of home health aides, visits to adult day care
facilities, and other non-institutional care.
Based on a microsimulation of people from around age 65 in 2015 to the end of their
lives, Favreault and Dey (2016) forecast the ADL limitations of future elderly and
their need for long-term care services. The goal of this exercise was to better
understand the near-term future trends in this area and to forecast the average level
of spending required. Specifically, the authors focused on the need for long-term
services and support because of a disability that meets the criteria set in the 1996
3
Other explanations include changes in disability insurance laws (greater incentives
to report disabilities that otherwise went unreported) and technological advances in
medicine (new treatments can delay death for those who are chronically frail and
otherwise would have died at a younger age).
4
The forecasts of Lakdawalla et al. (2003) are not without some controversy.
Manton (2003) argued that the use of certain data and assumptions in Lakdawalla et
al. (2003) resulted in an incorrect conclusion. He expected nursing home use will
continue to decline.
5
The CBO calculated this figure by multiplying the average wage earned by a home
health aide ($21 per hour) by the 11.2 billion hours of donated care extrapolated
from responses to the HRS. It did not account for forgone earnings of the caregiver
in excess of $21 per hour.
6
The CBO defines the economic value of institutional care as the cost of stays,
including room and board as well as assistive services, in skilled nursing facilities,
nursing homes, and nursing facilities housed inside continuing care retirement
communities. It defines the economic value of community-based care as the cost of
assistive services provided in all other settings, including private homes, adult day
care facilities, and facilities that are not nursing homes.

6
Health Insurance Portability and Accountability Act (HIPAA), namely a need for
assistance with at least two ADLs that is expected to last at least 90 days or a need
for substantial supervision for health and safety threats due to severe cognitive
impairment. The study found that 52% of people who turn 65 years old in 2015-
2019 will at some time in their lives need (informal or formal) long-term services and
support because of such a disability. Excluding informal care by relatives or friends,
47% will need formal long-term services and support, including 23% who will need it
for less than one year and 6% who will need it for five years or more (see Table 2).
Including elderly who will not need any formal care, this cohort will need formal
assistance for one year on average. Women are more likely to need assistance than
men (52% versus 42%), people with lower incomes are somewhat more likely to
need assistance than those with higher incomes, and the need for assistance is, as
expected, greater for those in poor health than those in good health at age 65.
Table 2. Projected Use of Paid LTSS for Persons Turning 65 in 2015-2019, by
Gender, Income Quintile and Self-Reported Health Status at Age 65
Favreault and Dey (2016) further projected that formal long-term services and
support will cost an average of $138,100 per person turning 65 in 2015-2019,
expressed in 2015 dollars. This average translates into $266,000 per user of formal
care. Of this amount, community-based care will cost 53% and care at nursing
facilities 47%. Assuming current finance mechanisms, the majority (52%) of formal
long-term services and support is expected to be paid out of pocket. The authors
expect Medicare to pay 10%, Medicaid 34%, and private insurance 3%.
Distribution for all
None <1 year
1.00-
1.99
years
2.00-
4.99
years
>5
years
Gender
Men 0.7 42.0 58.0 22.2 8.5 8.0 3.4
Women 1.3 52.1 47.9 23.1 9.5 11.2 8.3
Income Quintile at Age 65
Lowest 1.2 49.0 51.0 20.7 9.1 11.2 8.1
Second 1.2 48.1 52.0 21.1 8.7 11.0 7.3
Middle 1.1 48.7 51.3 22.5 9.7 9.6 6.8
Fourth 0.9 45.2 54.8 22.7 8.4 8.7 5.4
Highest 0.8 46.3 53.7 24.9 9.2 8.8 3.5
Health Status at Age 65
Excellent 1.0 46.8 53.2 24.0 7.6 9.9 5.4
Very good 0.9 46.1 53.9 23.1 8.7 9.5 4.8
Good 1.1 47.1 52.9 22.1 8.4 10.0 6.6
Fair/poor 1.1 49.0 51.0 22.0 10.8 9.4 6.7
Marital Status at Age 65
Married 0.9 45.8 54.2 23.2 8.6 8.9 5.1
Unmarried 1.2 50.0 50.0 21.5 9.9 11.2 7.5
Total 1.0 47.2 52.8 22.7 9.0 9.7 5.9
Source: Favreault and Dey (2016).
Average
years of
formal LTSS
use
Percent
with any
formal LTSS
use
7
While different sources suggest different payor mixes, financing long-term care at
nursing homes is largely through government-funded Medicaid and Medicare
programs.
7
According to a study by The Kaiser Family Foundation, Medicaid was the
primary payor for 63% of nursing facility residents in 2011, 14% were primarily
covered by Medicare, and 22% were private payors (Kaiser Family Foundation 2013).
The Kaiser study was based on the Online Survey, Certification, and Reporting
(OSCAR) system, a database that contains detailed information on Medicaid and
Medicare certified nursing facilities. Our own analysis of a different but related data
source, SNF cost reports, suggests that Medicaid was the primary payor for 53% of
resident-days in 2014, Medicare for 13%, and private payors for 34% (see Section
3), with only minor changes in this distribution since 2011.
The daily reimbursement of SNFs by Medicare tends to be higher than that by
Medicaid. Mostly depending on a patient’s care needs, Medicare payments range
from approximately $195 to $803 per day in 2016 (CMS 2015). Medicaid payments
vary by state and are typically a flat rate per day, irrespective of care needs, with
limited adjustments for cost differences across geographies. For example, in Florida
in 2015, the 10
th
and 90
th
percentiles of daily reimbursements were approximately
$203 and $257, respectively (authors’ calculations based on Florida AHCA 2015).
For formal care as a whole, CBO (2013) found that out of the $192 billion in
payments for formal care in 2011, $68 billion was paid through Medicare, $60 billion
through Medicaid, $39 billion was paid out of pocket (including beneficiaries’ cost
sharing for Medicare and Medicaid), and $12 billion was covered through private
insurance. The remaining $12 billion were from such other sources as the
Department of Defense, the Department of Veterans Affairs, and charitable
donations. See Table 3, which also shows the expenditures for community-based and
institutional settings (defined in footnote 6).
Table 3. Expenditures for Long-Term Care Services for Elderly People (2011)
Payors differ in their length of coverage. For example, Medicare and private health
insurance offer short-term coverage for post-acute care rehabilitative services in the
form of nursing home stays and home health visits (about three months coverage or
less). Medicaid and private LTC insurance offer much longer coverage periods (three-
7
Medicare offers limited coverage for skilled nursing care in a SNF. Among other
restrictions, the stay must be preceded by an acute-care hospital stay. If eligibility
conditions are met, Medicare generally pays the full cost for up to 20 days and
requires co-insurance payments of $161 per day (in 2016) for days 21-100. It does
not cover stays beyond 100 days.
Source of payment
Community-Based
($ bn)
Institutional
($ bn)
Total Care
($bn)
Medicare 31 37 68
Medicaid 20 40 60
Out of Pocket 3 36 39
Private Insurance 2 10 12
Other 1 11 12
Total 58 134 192
Source: CBO (2013).
8
to five-year terms) and will cover without a previous acute health episode.
According
to the CBO (2013), the distribution of LTC insurance and Medicaid coverage for the
elderly population living in the community varies by level of disability. Those with
three or more functional limitations are five times more likely to be covered by
Medicaid (24%, on average, from 2000 to 2010) than those with no functional
limitations (5%). While only 5% of those with no functional limitations were Medicaid
beneficiaries, 15% were covered by LTC insurance.
As shown in Table 4, the costs of long-term care can be substantial. The nationwide
median cost of in-home assistance by a homemaker or home health aide was $20
per hour in 2015 (Genworth 2015). Assuming four hours of assistance per day, five
days a week, this amounts to $20,800 annually.
8
The median rate for adult day care
was $69 per day ($17,940 per year at five days per week). An intermediate level of
personal care and health services, less extensive than in a nursing home, is offered
by assisted living facilities, which charge a median of $3,600 per month ($43,200 per
year). Finally, the median cost of nursing homes was $220 per day ($80,300 per
year) for a semi-private room and $250 per day ($91,250 per year) for a private
room. These rates reflect prices that are payable out of pocket or with private
insurance and may differ from those reimbursed by public programs.
Table 4. Nationwide Median Prices of Long-Term Care Services (2015)
According to Genworth (2015), the costs for institutionalized long-term care have
outpaced those for in-home care. From 2010 to 2015, nursing home costs increased
by 3.5%-4.0% annually, compared with 1.0%-1.6% annually for homemakers and
home health aides. Similarly, CBO (2013) reported annual nursing home cost
increases of 4.0%-4.5% between 2002 and 2012, compared with 1.6% annually for
home health aides.
Table 4 displays national median costs, but LTC costs vary widely across states.
Alaska tends to have the highest costs, with the statewide median cost of a private
room in a nursing home exceeding the national median by 208%. Other states with
very high costs include Connecticut (+74%), Massachusetts (+53%), New York
(+50%), and Hawaii (+48%), while relatively low-cost states include Oklahoma
(-34%), Missouri (-33%), Louisiana (-32%), Kansas (-28%), and Arkansas (-28%).
See Appendix A for a list of median LTC prices by state.
8
Home health care is typically provided on a part-time basis. MetLife (2012), which
compiled similar price data as Genworth (2015), assumed four hours per day, five
days per week, 52 weeks per year to annualize its figures.
Rate Annual
Nursing home, private room $250 per day $91,250
Nursing home, semi-private room $220 per day $80,300
Assisted living facility $3,600 per month $43,200
Adult day care $69 per day $17,940
Home health aid care $20 per hour $20,800
Source: Genworth (2015).
Annual rates for home care are based on 4 hours per day,
5 days per week; annual rates for adult day services are
based on 5 days per week.

9
3. COST REPORTS OF SKILLED NURSING FACILITIES
SNFs that participate in the Medicare program are required to annually submit a cost
report to CMS. Among many other items, these cost reports list the number of
resident-days primarily paid for by Medicare, Medicaid, and all other payors
combined (mostly LTC insurance and self-payments). Hospital-based SNFs report on
the cost report of the hospital; freestanding SNFs report on a separate report.
9
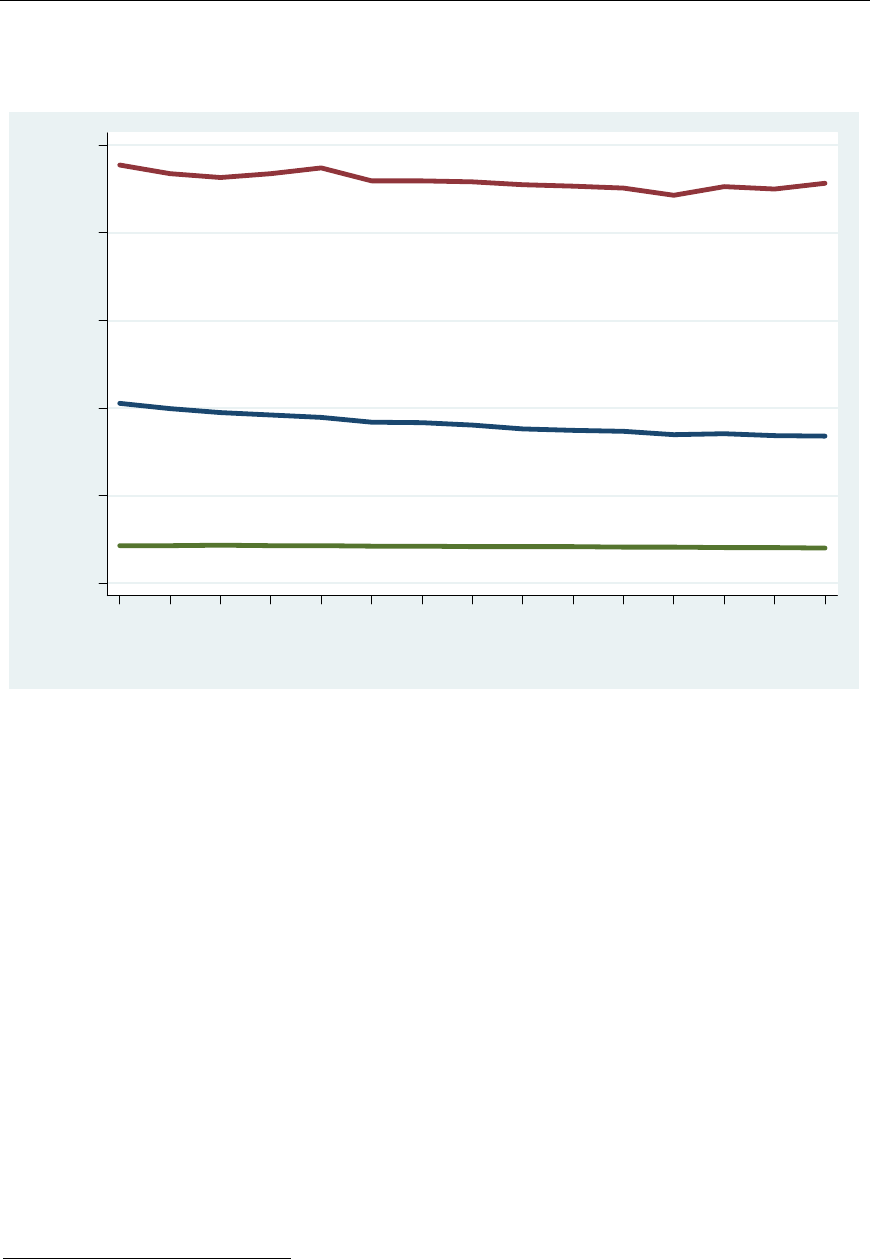
Figure 1 shows the number of resident-days reported by all freestanding SNFs in the
United States that participate in the Medicare program. The number of resident-days
is converted into resident-years to show the average number of people who are
resident at SNFs during the year. The number has been fairly stable at approximately
1.35 million from 2008 through 2014.
Figure 1. Number of Resident-Years Reported by Freestanding SNFs, by
Primary Payor and Year
The payor mix has also been fairly stable over this period. Approximately 13% of
resident-days are primarily paid by Medicare, 53% by Medicaid, and 34% by other
payors (Figure 2). These figures relate to resident-days. In terms of dollar
expenditures, CBO (2013) found Medicare paid for 28% of institutional care services,
9
Medicare cost reports are stored in the Healthcare Cost Report Information System
(HCRIS), available at https://www.cms.gov/Research-Statistics-Data-and-
Systems/Downloadable-Public-Use-Files/Cost-Reports.
Medicare
Medicaid
Other
0.0
0.3
0.6
0.9
1.2
1.5
0.0
0.3
0.6
0.9
1.2
1.5
Number of resident-years (millions)
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014
Source: CMS Healthcare Cost Report Information System.

10
Medicaid for 30%, and other sources for 43% (see the second column of Table 3
above).
Figure 2. Distribution of Primary Payor of Resident-Years Reported by
Freestanding SNFs, by Year
Figure 3 shows the average length of stay as reported by freestanding SNFs on their
Medicare cost reports.
10
As expected given Medicare’s coverage of at most 100 days,
the average length of resident stays that were primarily paid by Medicare was
shorter (39 days in 2014) than that of stays primarily paid by Medicaid (460 days in
2014). SNFs are not required to report the average length of stays that were
primarily paid for by private payors. Instead, only the average length of stay across
all primary payors is reported (165 days in 2014). Figure 3 also shows that average
lengths of stay have generally decreased somewhat since 2000.
10
Some SNFs reported implausibly short or long average lengths of stay. We
excluded the bottom and top deciles of average lengths of stay in our calculations.
The averages are weighted by reported number of resident-days.
Medicare
Medicaid
Other
0%
20%
40%
60%
80%
100%
0%
20%
40%
60%
80%
100%
200020012002200320042005200620072008200920102011201220132014
Source: CMS Healthcare Cost Report Information System.
11
Figure 3. Average Length of Stay Reported by Freestanding SNFs, by Payor
and Year
4. LONG-TERM CARE INSURANCE
As documented above, the cost of long-term care can be substantial. The average
cost for those who are projected to use formal care, $266,000 (Favreault and Dey,
2016), can exhaust the lifetime savings of many retirees. People at the high end of
the income or wealth distributions may be able to self-insure against the financial
risks of long-term care, whereas those at the low end may expect Medicaid to cover
the costs. For Americans in between, private long-term care insurance may provide a
solution.
Currently sold LTCI policies typically offer both home care and nursing home
benefits, but that was not the case for older policies. For example, 63% of policies
sold in 1990 offered nursing home benefits only and 37% offered both home care
and nursing home benefits (Cohen 2016). In 2015, 99% of policies sold offered both
types of benefits. Coverage limits are often anchored on a daily or monthly
maximum for nursing home stays and a lifetime maximum benefit, with maximums
for care outside nursing homes expressed as a percentage of the nursing home
benefit. Appendix B shows key pages from a sample policy published by Genworth.
In that example, the nursing home maximum is $4,000 per month, the residential
care facility benefit maximum is 75% or 100% of $4,000 per month,
11
and the home
11
The policy defines a residential care facility as a state-licensed Residential Care
Facility for the Elderly or similar. Such facilities provide 24-hour care to support
Medicare
Medicaid
Medicare, Medicaid, and Other
0
100
200
300
400
500
Average length of stay (days)
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014
Source: CMS Healthcare Cost Report Information System.
Average length of stay excluding reports in the bottom and top deciles.
12
and community care benefit maximum is 50% or 100% of $4,000 per month,
12
depending on the generosity of the policy purchased. The total benefit payments are
subject to a lifetime cap of $240,000. Benefit maximums may or may not be
increased over time to protect against inflation. The sample policy shows benefit
increases of 5% per year. Policies are also often subject to an elimination period,
also known as a deductible period. For example, an elimination period of 90 days can
imply that benefits are paid only after 90 days following a first covered expense
while chronically ill.
LTCI policies can be in force for decades. Most policyholders (54%) applied when
they were 55-64 years old, well before they expected to need benefits (AALTCI
2015). Policies are typically guaranteed renewable at an annual premium that is
designed to be constant for the duration of the policy contract, even with annual
benefit increases and even if a claim was made. However, while designed to be
constant for the duration of the contract, the premium may be changed for a variety
of reasons, including actual or estimated experiences of all holders of a particular
policy form. It is our understanding that premium changes require the approval of
state insurance regulators.
Premiums on individual policies may change and indeed they have changed. Most
insurers’ LTCI policies issued before the mid-2000s have seen adverse experience
when compared to their original pricing assumptions. Rising claims, low mortality
and lower than expected lapses have led to higher prices often unaffordable to a
large segment of the affected population (Karapiperis and Nordman, 2016).
According to the chief executive of Genworth Financial, which has a long-term care
insurance market share of roughly 35%, average premium increases of 50% were
needed to break even on policies issued before 2002 (Carrns 2014). State regulators
appear to have been generally receptive to proposed rate increases.
The Federal Long Term Care Insurance Program (FLTCIP) offers voluntary private
LTCI to Federal employees, who are responsible for the full premiums. It, too,
appears to have underestimated the costs of providing benefits. In November 2016,
FLTCIP premiums are scheduled to increase by an average of 83% (Davidson 2016).
Cohen (2016) documented that policies sold in 2015 offered an average daily benefit
amount for nursing homes of $159 and for home care of $152. The lifetime cap
supported, on average 3.8 years of nursing home care. Three-out-of-four policies
featured annual benefit increases to protect against inflation. The average deductible
period was 93 days. The average annual premium was $2,772. The policies generally
appear less generous than those sold during the 1990s. For example, the lifetime
cap in 1990 supported on average 5.6 years of nursing home care, the average
deductible period was 20 days, and the average premium $1,071 (about $1,942 in
2015 dollars).
needs resulting from impairment in ADLs or in cognitive ability, provide three meals
per day, have agreements to ensure that residents receive the medical care services
of a physician or nurse in case of emergency, and meet certain other criteria.
12
Under the sample policy, home and community benefit care benefits include adult
day care, nurse and therapist services, home health care, personal care services,
and homemaker services.

13
Table 5 shows average annual premiums for basic LTC insurance, by age of the
insured at the time the policy was purchased (NAIC 2013). Premiums increase with
age, roughly tripling from $4,349 for people age 50 to $13,500 for those buying at
age 75 for inflation-protected policies with a 4-year maximum benefit period.
Table 5. Average Annual Premium for Basic Long-Term Insurance, $200
Daily Benefit (2013)
Most claimants of LTC benefits are at least in their 80s when they start using covered
services. About 2% are under age 60, 9% are in their 60s, 25% in their 70s, and
64% age 80 or older (AALTCI 2015; see Table 6).
Table 6. Age of Claimant for New Claims Opened (2012)
About one-half of new claimants receive in-home care, one-in-five receive benefits
for assisted living, and about 31% moved into a nursing home (AALTCI 2015; see
Table 7).
Table 7. Newly Opened Long-Term Care Insurance Claims Paid For
According to the National Association of Insurance Commissioners (NAIC 2015), 7.2
million people were covered by LTC insurance in 2014, and the American Association
for Long-Term Care Insurance (AALTCI 2015) estimated that 8.1 million Americans
4 Years of Benefits 6 Years of Benefits Lifetime Benefits
50 $4,349 $5,083 $7,347
60 $5,331 $6,269 $8,927
70 $9,206 $10,549 $15,070
75 $13,500 $15,157 $20,930
4 Years of Benefits 6 Years of Benefits Lifetime Benefits
50 $1,294 $1,514 $1,997
60 $2,057 $2,426 $3,307
70 $4,914 $5,834 $7,777
75 $8,146 $8,291 $12,337
Source: NAIC (2013).
Age When
Buy
With Inflation Protection 5% Compounded Per Year
With No Inflation Protection—Benefit Stays at $200 per Day
Age Percent
Under 50 0.3%
50 to 59 1.9%
60 to 69 8.7%
70 to 79 25.4%
80 and over 63.7%
Source: AALTCI (2015).
Service Percent
Home Care 51.0%
Assisted Living 18.5%
Nursing Home 30.5%
Source: AALTCI (2015).

14
were insured for long-term care in 2014. About 255,000 policyholders were receiving
benefits in 2014 (NAIC 2015).
Perhaps in response to unexpected losses to insurance companies and unexpected
rate increases to consumers, the market landscape for long-term care insurance has
shifted dramatically over the past decade. There is a trend toward smaller daily
benefits, shorter benefit periods (i.e., lower lifetime benefit caps), and less inflation
protection. Many smaller carriers have exited the market (Gleckman 2013, 2015)
and sales of individual LTCI policies plummeted from a high of 754,000 in 2002 to
just 129,000 in 2014 (Cohen 2016). That said, so-called combination or hybrid
products have gained popularity. These products combine LTC benefits with either
life insurance or an annuity. In combination with life insurance, if LTC is needed, the
death benefit is accelerated. In combination with an annuity, if LTC is not needed,
there is an annuity payout. Sales of combination products rose from 273,000 in 2009
to 535,000 in 2013 (Cohen 2016).
In a series of essays, Brown and Finkelstein (2007, 2008, 2009, 2011) addressed the
relatively small size of the market for private LTCI. They pointed out that 35%-50%
of 65 year-olds will use a nursing home at some point in their remaining lives and
that, of those who use a nursing home, 10%-20% will live there more than five
years. At current median prices, five years of nursing home residency cost in excess
of $400,000 (see Table 4 above). Despite a sizable risk of large future expenditures,
private LTCI pays for only 6% of LTC expenses, whereas out-of-pocket payments
account for 20% (see Table 3 above). Brown and Finkelstein evaluated supply and
demand side factors to explain the small role of private LTCI.
Supply side issues are reflected in premiums that far exceed expected benefits and
typical benefits that only partially cover costs. On average, the present value of
benefits is only one-half of the present value of lifetime premiums (Brown and
Finkelstein 2011). Further, while pricing is unisex, men are less likely to incur LTC
expenses than women—men receive benefits of only about 34 cents per premium
dollar, compared with 64 cents received by women. The authors suggest several
supply-side factors that may be responsible for the high premiums and less-than-full
coverage. Among these are transaction and administration costs, lack of a
competitive market, adverse selection and moral hazard, and contracting issues.
Finkelstein and McGarry (2006) found that adverse selection (disproportionate
enrollment by high-risk individuals) and moral hazard (disproportionate utilization by
insured individuals) are offset by a strong taste for insurance among low-risk
individuals. (Our Table 17 below is consistent with that conclusion.) Because of the
very long-term nature of LTCI policies, contracting issues may be particularly
troublesome. While contractually adjustable, premiums are intended to be fixed in
nominal terms for the duration of the policy—typically several decades—even when
benefits are inflated annually. The insurance company may go bankrupt, creating a
risk for the policyholder that benefits may never materialize. Also, the insurance
company may not be able to pool certain risks, such as the risk that prices for long-
term care rise faster than expected or that returns on invested premiums are below
expectations.
However, even if supply side issues could be resolved and premiums would be
actuarially fair, demand side issues likely stand in the way of widespread LTC
insurance. Brown and Finkelstein (2009) cite several demand side issues. First,
consumers may underestimate the risks and costs of long-term care. Second, they
may value consumption when institutionalized less highly than when not, thus

15
reducing the incentive to smooth out consumption through insurance. Third, they
may take into account imperfect but less expensive alternatives to private insurance,
such as care provided by a spouse or other family members, financial transfers from
adult children, or Medicaid. In particular, two aspects of the structure of Medicaid
reduce demand for private LTCI: means-testing and Medicaid being the secondary
payer. Means testing implies that every dollar in private benefits postpones Medicaid
eligibility, and Medicaid being the secondary payer implies that it is not available to
top up private LTCI benefits, which typically cover only part of the costs. Brown and
Finkelstein (2008) calculated the “implicit tax” of Medicaid—the part of the LTCI
premium that goes to pay for benefits that end up duplicating benefits that Medicaid
would have paid for in the absence of a private policy—at 60% for a man at the
median of the wealth distribution. In other words, 60 cents out of every dollar of
private benefits simply serve to replace benefits that Medicaid would have provided.
For women, they estimated the implicit tax rate at 75%.
In short, Brown and Finkelstein argue that supply side issues lift premiums to levels
far above expected benefits and that demand side issues sharply reduce the net
benefits that private insurance will provide.
StateMedicaidPartnershipPrograms
In recent years many states have implemented so-called Partnership Programs
between Medicaid and private insurance companies. These programs are designed to
encourage middle-income Americans to purchase long-term care insurance. To
qualify for basic Medicaid, one generally needs to spend down assets. However,
holders of LTCI policies that meet Partnership criteria may qualify for Medicaid after
their long-term care benefits run out while preserving assets. For example, if a
policyholder needs long-term care after exhausting his lifetime maximum benefit of,
say, $300,000, he may qualify for Medicaid while retaining $300,000 in assets
beyond the usual Medicaid criteria. The California Partnership Program describes the
asset protection aspect as follows (California DHCS 2010; emphasis in original):
Medi-Cal [California’s Medicaid program] Asset Protection is available in
Partnership policies through an alliance between the State of California and
select private insurers who agree to market high-quality long-term care
insurance policies. Asset Protection guarantees you get to keep a dollar's
worth of assets for each dollar your Partnership insurance policy pays out for
long-term care services. If you use up your long-term care insurance
coverage and still need long-term care, you may apply for Medi-Cal. When
qualifying for Medi-Cal, you are entitled to keep assets Medi-Cal normally
allows, plus assets equal to the amount the Partnership policy has paid out in
benefits. This means you can purchase a Partnership policy equal to the
amount of assets you wish to protect. The State of California will also
disregard these protected assets when making a claim through Medi-Cal
Estate Recovery.
As of March 2014, 44 states and the District of Columbia had implemented a
Partnership Program. State requirements for policies to meet Partnership standards
vary, but most require inflation protection through benefits that increase
automatically over time. With the exception of California, Partnership states allow
reciprocity, i.e., they grant asset exemptions based on Partnership policies that were

16
purchased under another state’s Partnership Program (New York SPLTC 2016,
AALTCI 2016a).
By 2015, Partnership policies accounted for slightly more than two-in-five new
policies sold (Cohen 2016).
Employer‐ProvidedLong‐TermCareBenefits
Long-term care insurance coverage may be obtained through individual policies or
through employer-sponsored group policies. NAIC (2015) documented that by the
end of 2014, 7.2 million lives were covered by LTCI. Of these, 5.0 million (69%)
were individual policies and 2.2 million (31%) were certificates under group plans.
13
The National Compensation Survey indicates that 18% of civilian workers had access
to long-term care insurance through their employer (NCS 2014). In other words, the
employers of 18% of civilian workers sponsored a long-term care insurance benefit.
Although sponsored by the employer, benefits are typically fully paid for by the
employee. From the employee’s point of view, the main advantages of an employer-
sponsored plan are potential group discounts and, for larger groups, often simplified
medical underwriting (such as without a medical examination). After separating from
their employer, the policy certificate stays with the employee.
Take-up rates are very low, with different sources reporting estimates from 5%-7%
of eligible employees taking up long-term care insurance (CIPR 2016; Pincus et al.,
2013).
We conducted an analysis of Form 5500 filings to gain insights into the prevalence of
employer-sponsored long-term care coverage. The Employee Retirement Income
Security Act (ERISA) requires any administrator or sponsor of an employee benefit
plan subject to ERISA to annually report details on such plans unless exempt from
filing pursuant to regulations issued by the DOL. Welfare plans with fewer than 100
participants are generally exempt, except if they operate a trust. For the purpose of
this report, only plans with 100 or more participants are included. Non-ERISA plans,
such as governmental plans and church plans, do not need to file a Form 5500 and
are not covered by the analysis in this section.
The Form 5500 does not ask specifically about long-term care benefits. Line 8b on
the main Form asks for the plan’s benefit types, but there is no code for long-term
care benefits. Details about underlying insurance contracts, if any, are reported on
Schedules A. Line 8 of the Schedule A asks for the benefit type of the insurance
contract, but, again, there is no checkbox for long-term care benefits. However,
plans may check “Other” and write in the appropriate benefit type. We searched
these free-form text boxes for such phrases as “long-term care” and “LTC”. In recent
years roughly 2,000 plans annually indicated offering LTC benefits; see Table 8.
14
13
Technically, most employer-sponsored plans are not group plans but multi-life
policies, i.e., individual long-term care insurance policies bundled together with a
group discount (AALTCI 2016b).
14
Since these figures originate from Schedules A, they exclude long-term care
benefits offered by employers that self-insure those benefits. We are unaware of the
prevalence of self-insured long-term care benefits.

17
Table 8. Employer-Provided Long-Term Care Coverage and Annual Premiums
Table 8 suggests that the number of plans that offer LTC benefits has increased over
time, but it is unclear to what extent the increase is due to more-complete reporting.
The number of “covered persons” under the reported insurance contracts has been
between approximately 950,000 and 980,000 in 2011-2014, which corresponds to
1.3%-1.4% of all welfare plan participants.
15
As noted earlier in this section, the
number of group LTCI certificates is about 2.2 million (NAIC 2015), suggesting that
employer-sponsored long-term care insurance benefits are underreported on Form
5500 filings.
Table 8 also shows the average and median annual premium that the employer
reported paying for LTC benefits. The average annual premium in 2014 was $883
and the median was $661. These figures are well below average premiums in the
individual market (see Table 5), possibly in part because of the age composition of
plan participants, because of coverage limits, or because of discontinuation rates
upon job separation.
15
The number of covered persons is taken from Line 1e of Schedule A and the
number of welfare plan participants from Line 6d on the main Form. Some
companies file a single Form 5500 for all their welfare benefits, whereas others file
multiple Forms 5500. To prevent double counting of welfare plan participants, we
included only a single welfare plan filing per employer (as identified by Employer
Identification Number, EIN), namely the plan with the greatest number of
participants.
Year
Number of
plans
Number of
covered plan
participants
Percent of all
welfare plan
participants
Average annual
premium per
person covered
Median annual
premium per
person covered
2000 315 419,843 0.90% $575 $401
2001 523 466,378 0.72% $572 $399
2002 634 516,516 0.78% $726 $405
2003 735 618,056 0.95% $788 $430
2004 957 692,110 1.02% $631 $461
2005 1,112 735,044 1.06% $690 $497
2006 1,286 859,595 1.20% $769 $521
2007 1,409 863,228 1.18% $662 $553
2008 1,568 924,364 1.25% $665 $541
2009 1,693 829,086 1.19% $838 $597
2010 1,826 922,303 1.30% $787 $626
2011 1,918 949,141 1.33% $802 $603
2012 2,019 975,785 1.35% $858 $632
2013 2,029 982,826 1.36% $851 $638
2014 2,037 954,836 1.30% $883 $661
Source: Form 5500 filings for welfare plans with 100 or more participants.

18
5. ANALYSIS OF HEALTH AND RETIREMENT STUDY
DATA
For an analysis of the financial consequences of long-term care, we turn to the HRS.
The HRS is a longitudinal survey of Americans over the age of 50, and their spouses.
It collects information about health, certain types of health care utilization (including
home health care and nursing home stays), informal care by relatives, insurance
coverage, out-of-pocket medical expenses, assets, and income. The HRS sample is
drawn from the non-institutionalized population, but respondents are followed even if
they move into a nursing home or other health care facility.
16
Since most
respondents enter the survey when they are 51 to 61 years old, the exclusion of
institutionalized individuals from its sampling frame is presumably not a major
limitation.
The HRS started in 1992 with a sample of individuals aged 51-61, and their spouses.
Insofar possible, they have been re-interviewed every other year. In 1993, a cohort
of individuals age 70 and older, and their spouses, was added to the HRS. Insofar
possible, they were re-interviewed in 1995, 1998, and every other year thereafter.
In 1998, 2004, and 2010 new cohorts of individuals aged 51-61, and their spouses,
were added. Therefore, the age distribution was unusual in the early years of the
HRS, but the sample became more representative of the older population in later
years. To mitigate effects of an incomplete age distribution, we present results based
on the 1998 and later waves only. Our analysis incorporates HRS waves through
2012. The sample size is approximately 17,000-22,000 respondents (12,000-15,000
households) per wave.
Table 9 shows the distribution of HRS respondents by age and sex, for the eight
waves from 1998 to 2012. Approximately 59% of respondents are women. Most
respondents are in their 50s or 60s, but 20% are in their 70s, 11% in their 80s, and
2% are age 90 or older.
Table 9. Distribution of Respondents by Age and Sex
16
The HRS uses the following definition: “A nursing home or other health facility
provides all of the following services for its residents: dispensing of medication, 24-
hour nursing assistance and supervision, personal assistance, and room & meals”
(see Section A of HRS questionnaires, such as the 2012 version at
http://hrsonline.isr.umich.edu/modules/meta/2012/core/qnaire/online/01hr12A.pdf).
Female Male Total
Age Freq. Percent Freq. Percent Freq. Percent
<50 4,128 0.1% 1,060 0.0% 5,188 0.1%
50-59 23,302 33.8% 16,304 36.8% 39,606 35.1%
60-69 27,409 29.6% 21,353 32.4% 48,762 30.9%
70-79 22,107 21.3% 17,616 20.4% 39,723 20.9%
80-89 12,371 12.6% 7,744 9.1% 20,115 11.0%
90+ 2,963 2.7% 1,174 1.3% 4,137 2.1%
Total 92,280 100.0% 65,251 100.0% 157,531 100.0%
Source: 1998-2012 HRS.
Note: Percentages are weighted.

19
Table 10 tabulates utilization of home health care and nursing homes during the two
years between survey interviews, by year. In this table and subsequent HRS-based
tables, frequency counts reflect the raw number of respondents (possibly in multiple
interview waves) and percentages are weighted by respondent weights.
17
Roughly
7%-8% of respondents had utilized home health care and 4% had stayed at least
one night in a nursing home. In addition, the last two columns show that roughly 2%
of respondents were resident at a nursing home at the time of the survey.
Table 10. Utilization of Home Health Care and Nursing Homes in the Past 2
Years, Nursing Home Residency at the Time of the HRS Interview, by Year
Similar to Table 10, Table 11 tabulates utilization of home health care and nursing
homes during the two years between survey interviews, but by age of the
respondent rather than by year. As expected, use of LTC services increased with age.
Table 11. Utilization of Home Health Care and Nursing Homes in the Past 2
Years, Nursing Home Residency at the Time of the HRS Interview, by Age
Figure 4 and Table 12 show the prevalence of LTC insurance among HRS
respondents aged 51-69. LTC insurance coverage has remained approximately
unchanged at about 9%-10% since 2002. A small fraction of policies cover in-home
17
Regular respondent weights are zero for institutionalized respondents. From 2000-
2010, the HRS provided respondent weights for institutionalized respondents. Where
available, we used such institutional weights. Where unavailable, we imputed
weights based on respondent weights in prior or subsequent interview waves.
Year
Utilized Home
Health Care
Stayed in
Nursing Home
Institutionalized
at Interview
1998 7.1% 3.0% 1.8%
2000 6.5% 3.7% 2.5%
2002 6.8% 4.4% 2.4%
2004 5.9% 3.4% 1.9%
2006 7.1% 4.0% 1.9%
2008 7.5% 4.0% 1.9%
2010 7.9% 3.7% 1.4%
2012 7.9% 4.2% 1.8%
Total 7.1% 3.8% 1.9%
Source: 1998-2012 HRS.
Age
Utilized Home
Health Care
Stayed in
Nursing Home
Institutionalized
at Interview
<50 1.0% 1.1% 0.0%
50-59 3.2% 0.6% 0.1%
60-69 5.4% 1.6% 0.6%
70-79 9.6% 4.6% 1.9%
80-89 16.6% 13.5% 7.5%
90+ 29.3% 31.3% 22.5%
Total 7.1% 3.8% 1.9%
Source: 1998-2012 HRS.

20
care or nursing home care only, but most cover both. This is consistent with Cohen
(2016).
Figure 4. Prevalence and Type of Long-Term Care Insurance
(Respondents Aged 51-69 in 1998-2012)
Table 12. Prevalence and Type of Long-Term Care Insurance
(Respondents Aged 51-69 in 1998-2012)
As documented by Cohen (2016) and discussed on page 11 above, currently sold
policies tend to cover both in-home and nursing home care, but older policies were
more restrictive. Recognizing that older policies tend to be held by older birth
cohorts, Table 13 shows benefit types by age of the HRS respondent. About 87%
(9.8%/11.2%) of policies held by 60-69 year-olds covered both in-home and nursing
0%
2%
4%
6%
8%
10%
12%
1998 2000 2002 2004 2006 2008 2010 2012
Source: HRS respondents age 51-69
Other
In-home care only
Nursing home care only
Both
Year
Nursing Home
and Home Care
Nursing Home
Care Only
Home
Care Only Other Total
1998 6.0% 1.1% 0.8% 0.1% 8.0%
2000 6.6% 0.7% 0.6% 0.0% 7.9%
2002 8.1% 0.9% 0.3% 0.2% 9.5%
2004 8.6% 0.7% 0.4% 0.1% 9.9%
2006 8.7% 0.6% 0.3% 0.0% 9.6%
2008 9.5% 0.7% 0.3% 0.1% 10.6%
2010 8.9% 0.6% 0.3% 0.1% 9.8%
2012 8.8% 0.6% 0.4% 0.0% 9.8%
Source: HRS Respondents aged 51-69.

21
home care. That fraction decreases with age to 81% among 70-79 year-olds, 69%
among 80-89 year-olds, and 57% among respondents age 90 or older.
Table 13. Prevalence and Type of Long-Term Care Insurance, by Age (1998-
2012)
Table 14 and Table 15 show the distribution of cumulative number of days spent in a
nursing home, by age of the respondent.
18
The days may have been spent
consecutively or over multiple nursing home stays. Table 14 shows the distribution
for the individual respondent. Most people never stayed in a nursing home, but the
fraction who did increases, as expected, with age. Among respondents who are age
90 or older, 11% had stayed 1-30 days, 6% 31-100 days, 6% 101 days to one year,
5% more than one year but less than two years, 10% two to four years, and 2% five
years or longer. Table 15 is similar to Table 14 but accounts for nursing home stays
of both the respondent and his or her partner.
Table 14. Cumulative Duration Spent in a Nursing Home, by Age
18
Cumulative number of days insofar reported in the HRS. Any stays prior to
entering the HRS sample are excluded. However, since most HRS respondents are in
their 50s when they enter the HRS, we believe this limitation to be mild. The tables
uses eight HRS waves (1998-2012), i.e., individual respondents can contribute
multiple times to the tables.
Age
Nursing Home
and Home Care
Nursing Home
Care Only
Home
Care Only Other Total
<50 2.5% 0.0% 1.0% 0.0% 3.5%
50-59 6.9% 0.5% 0.4% 0.1% 7.9%
60-69 9.8% 1.0% 0.4% 0.0% 11.2%
70-79 10.9% 1.9% 0.5% 0.1% 13.4%
80-89 7.8% 2.6% 0.8% 0.1% 11.3%
90+ 4.1% 2.4% 0.5% 0.1% 7.1%
Source: 1998-2012 HRS.
Age
Duration <50 50-59 60-69 70-79 80-89 90+ All
Zero days 98.9% 99.2% 97.3% 92.8% 80.5% 60.3% 94.4%
1-30 days 0.0% 0.5% 1.5% 3.9% 8.4% 11.0% 2.6%
31-100 days 1.1% 0.1% 0.4% 1.3% 3.4% 5.6% 0.9%
101-364 days 0.0% 0.1% 0.3% 0.7% 2.4% 5.9% 0.7%
1 year 0.0% 0.0% 0.1% 0.5% 2.0% 4.8% 0.5%
2-4 years 0.0% 0.0% 0.2% 0.7% 2.8% 10.2% 0.8%
5+ years 0.0%0.0%0.1%0.1%0.5%2.3%0.2%
Source: 1998-2012 HRS.

22
Table 15. Cumulative Duration Spent in a Nursing Home by Self or Partner,
by Respondent Age
Table 16 shows the fraction of individuals who reported Medicaid enrollment, by
duration spent in a nursing home. As expected, the longer someone was a resident
at a nursing home, the more likely he or she was receiving Medicaid benefits. More
than one-half (56%) of respondents who had spent five years or longer in a nursing
home reported Medicaid enrollment, compared with only 8% among those who had
never stayed in a nursing home. A likely explanation is that private assets and other
sources of payment become sufficiently depleted for a respondent to become eligible
for Medicaid.
Table 16. Medicaid Enrollment by Cumulative Duration Spent in Nursing
Home
Table 17 shows utilization of long-term care by age and by long-term care insurance
status. Table 11 above already showed that use of services increases with age; Table
17 documents that utilization among people with insurance is generally lower that
among their uninsured counterparts. Theoretically, adverse selection and moral
hazard could lead to the opposite pattern: people who expect to need long-term care
are more likely to purchase insurance protection, and people with insurance
coverage are more likely to use services because the net cost is lower for them.
However, for long-term care utilization those forces are outweighed by such other
factors as better health among LTCI policyholders. This finding is consistent with
Finkelstein and McGarry (2006), who concluded that in the market for long-term care
insurance individuals with a strong taste for purchasing insurance tend to be low-risk
and outnumber individuals with private information that they are high-risk.
Age
Duration <50 50-59 60-69 70-79 80-89 90+ All
Zero days 98.3% 98.6% 95.7% 89.0% 74.3% 54.8% 92.1%
1-30 days 0.0% 0.9% 2.4% 5.9% 11.0% 12.6% 3.8%
31-100 days 1.3% 0.2% 0.7% 2.0% 4.7% 6.7% 1.4%
101-364 days 0.4% 0.2% 0.5% 1.2% 3.3% 6.8% 1.0%
1 year 0.0% 0.0% 0.2% 0.6% 2.4% 5.2% 0.6%
2-4 years 0.0% 0.1% 0.4% 1.1% 3.7% 11.3% 1.0%
5+ years 0.0%0.0%0.1%0.2%0.6%2.7%0.2%
Source: 1998-2012 HRS.
Durat ion
Medicaid
Enrollment
Zero days 7.6%
1-30 days 11.7%
31-100 days 14.8%
101-364 days 26.1%
1 year 30.9%
2-4 years 37.4%
5+ years 55.9%
Total 8.7%
Source: 1998-2012 HRS.

23
Table 17. Utilization of Long-Term Care, by Age and LTC Insurance Status
The HRS does not ask about out-of-pocket expenses related to nursing home stays.
In an attempt to gauge the financial consequences of nursing home stays, Table 18
captures asset depletion between HRS interviews for households with and without
nursing home stays. The unit of analysis is a household interview that was preceded
by another interview. The analysis excludes households with any wage earnings. It
shows the distribution of financial assets (top panel) and net worth (bottom panel)
for households whose members never stayed in a nursing home throughout the time
that they were in the HRS and for households who reported at least one overnight
stay by either partner.
19
The latter group is further distinguished between
households who did or did not report a stay during the past two years. The
hypothesis is that the assets of households who reported a stay in the past two years
are more likely to deplete than those of other groups. Indeed the mean change in
assets is negative, but the magnitude of the average change would typically pay for
only a short nursing home stay.
19
Financial assets include checking accounts, savings accounts, stock holdings,
bonds, mutual funds, investment trusts, certificates of deposit, other savings (money
owed by others, a valuable collection for investment purposes, an annuity, or rights
in a trust or estate), and IRA holdings. Net worth further includes housing and other
real estate equity (net of mortgages) and the value of vehicles. Neither metric
includes defined contribution pension balances.
Used Home Health
Care in the Past 2
Years
Stayed in Nursing
Home in the Past 2
Years
In nursing home at
time of interview
LTC insurance at
interview?
LTC insurance at
interview?
LTC insurance at
interview?
AgeNoYes NoYes NoYes
<50 1.1% 0.0% 1.1% 0.0% 0.0% 0.0%
50-59 3.1% 4.0% 0.5% 0.6% 0.1% 0.1%
60-69 5.4% 4.8% 1.7% 1.3% 0.6% 0.4%
70-79 10.0% 7.2% 4.8% 3.1% 2.0% 0.9%
80-89 16.8% 14.5% 13.8% 10.1% 7.7% 4.8%
90+ 28.9% 31.9% 30.9% 30.7% 22.4% 17.8%
Total 7.1% 6.7% 3.8% 3.1% 2.0% 1.2%
Source: 1998-2012 HRS.

24
Table 18. Distribution of Change in Financial Assets, Total Assets in Past
Two Years
We turn to a mutivariate analysis of wealth changes between HRS interviews to
measure the financial impact of nursing home stays net of public or private insurance
coverage. As in the previous table, the analysis excludes households with any wage
earnings. It also excludes households with Medicaid beneficiaries, since their out-of-
pocket expenses are likely low. We distinguish between short stays (up to 30 days)
and long stays (more than 30 days), because short stays are often associated with
hospital stays and likely covered by Medicare or private health insurance. Our
hypothesis is that long stays pose the greatest financial risks, and that those risks
are mitigated if (either partner in) a household has private long-term care insurance.
See Table 19.
We are interested in wealth changes. However, wealth levels and their changes vary
widely across households, and outliers may drive results. We therefore measure
wealth through an inverse hyperbolic sine transformation. The inverse hyperbolic
sine is similar to a logarithmic transformation, but allows negative values.
20
Table 19
presents two specifications, for financial assets and net worth.
20
Formally, sinh
√
1. The inverse hyperbolic sine is point-
symmetric around the origin: sinh
sinh
.For positive wealth values w that
are not close to zero, sinh
2
, and for negative values not close to zero,
sinh
2
. For wealth levels that are both positive or both negative in the
current and prior interview, changes in the inverse hyperbolic sine may be
interpreted similar to changes in logarithms, i.e., as relative changes.
Change in Financial Assets (Incl. IRAs)
Subsample
25th
Percentile Median
75th
Percentile
Mean (excl. top
and bottom
deciles)
Never in Nursing Home -26,000 0 41,000 7,045
Ever in Nursing Home -28,000 0 37,000 5,159
Not in Past Two Years -21,326 500 45,000 11,302
During Past Two Years -36,000 -50 29,500 -1,113
Change in Net Worth
25th
Percentile Median
75th
Percentile
Mean (excl. top
and bottom
deciles)
Never in Nursing Home -52,400 4,682 91,000 18,505
Ever in Nursing Home -51,100 1,000 68,000 8,421
Not in Past Two Years -35,800 5,500 84,700 23,265
During Past Two Years -71,000 -1,000 56,500 -7,186
Source: 1998-2012 HRS.

25
Table 19. Wealth Change between HRS Surveys as a Function of Nursing
Home Stays and Insurance Coverage
(Outcome variable: Difference between waves of inverse hyperbolic sine of
wealth)
Consistent with our hypothesis, short nursing home stays did not have a statistically
significant effect on changes in wealth before and after the stay. However, stays in
excess of 30 days had a negative effect, except if the household had long-term care
insurance coverage. Not shown in the table is that the parameter estimates were
sensitive to the model specification, sample selection, and treatment of negative
wealth values. In other words, while the results are consistent with expectations,
direct measurement of out-of-pocket expenses may be preferable to measurement of
wealth changes. Unfortunately, the HRS currently does not offer such direct
measurement.
Finally, Table 20 shows probit regression results of the likelihood of Medicaid
enrollment. The unit of observation is a household interview and the outcome is an
indicator for whether (either partner in) a household reported being covered by
Medicaid. As expected, net worth is strongly negatively related to Medicaid
enrollment. In contrast to Table 19, nursing home stays are measured cumulatively,
with indicators for whether all nursing home stays by either partner prior to the
interview summed to 1-30 days or longer. Both short and long stays increased the
likelihood of Medicaid enrollment, but the effect of long stays was much greater.
Being covered by long-term care insurance reduced the chances of Medicaid
enrollment, presumably because of its association with sufficient means to pay for
such insurance. Contrary to our expectations, the effect of long stays was not
mitigated by long-term care insurance coverage.
Change in inverse hyperbolic sine of:
Financial Assets Net Worth
Short stay (<=30 days) -0.085 -0.085
(0.231) (0.142)
Long stay (>30 days) -0.674 ** -0.491 ***
(0.293) (0.180)
LTC insurance coverage -0.028 -0.048
(0.103) (0.064)
Long stay * LTC insurance 1.198 * 0.955 **
(0.675) (0.415)
Constant 0.054 0.053 *
(0.045) (0.027)
Number of observations 16,485 16,485
Standard errors in parentheses.
Significance: ***=1%, **=5%, *=10%.
Analysis sample excludes households with Medicaid beneficiaries.

26
Table 20. Household Medicaid Coverage as a Function of Cumulative Nursing
Home Stays
6. POLICY IMPLICATIONS
Approximately one-half of Baby Boomers are projected to require paid, formal long-
term care in the home, an adult day care center, an assisted living facility, or a
nursing home (Favreault and Dey, 2016). Paying for care out of pocket could rapidly
exhaust retirement savings of many Americans, prompting them to eventually rely
on Medicaid. Indeed, Medicaid enrollment is about 8% among HRS respondents who
have never stayed in a nursing home and rises to 26% after 101-364 days in a
nursing home and 56% after five years in a nursing home (see Table 16 above). The
size of the Baby Boom generation is expected to drive up demand for and prices of
long-term care, creating a troublesome outlook for the elderly’s personal finances
and the Medicaid program.
Given the high cost of long-term care, workable solutions could involve risk pooling
through public or private insurance. Only about 7 million people are currently
covered by private long-term care insurance, which suggests room for growth.
However, as argued by Brown and Finkelstein (2007, 2008, 2009, 2011) and
summarized above, both insurance companies and consumers face impediments to
more widespread adoption of private LTCI. Among these are uncertainty over the
adequacy of coverage and uncertainty over future premiums. Indeed, the insurance
is designed to be in force for several decades, and past experience shows costs that
outpaced general inflation and substantial premium increases on policies that were
issued prior to the mid-2000s. The uncertainties affect consumers and insurance
companies alike. Some options that may alleviate the uncertainties of both
consumers and the industry are:
Insurance products in which benefits and premiums adjust in tandem with
inflation. Inflation tends to affect the cost of care, wages, and nominal
investment returns in the same direction, so incorporating a link between
benefit levels and premiums should greatly reduce inflation uncertainty. Many
current products offer automatic benefit increases of 3% or 5% annually, but
Probit
Net worth -0.078 ***
(inverse hyperbolic sine)
(0.003)
Short stay(s) 0.164 **
(0<cumulative SNF nights<=30)
(0.066)
Long stay(s) 0.757 ***
(Cumulative SNF nights>30)
(0.057)
LTC insurance coverage -0.502 ***
(0.049)
Long stay(s) * LTC insurance 0.027
(0.147)
Constant -0.489 ***
(0.036)
Number of observations 26,797
Standard errors in parentheses.
Significance: ***=1%, **=5%, *=10%.

27
those increases may be too low or too high. Most products are designed to
charge the same annual premium for the life of the policy, which makes them
relatively expensive early on. Expecting income to keep pace with inflation,
prospective policyholders may be receptive to lower initial premiums that
escalate over time.
Products that combine long-term-care insurance with life insurance and/or
annuities. Longevity risks affect individual products differently, but a
combination product may be easier to price, require less complex
underwriting standards, and offer more comprehensive protection against
financial risks in old age.
State-based reinsurance pools designed to alleviate individual insurers’ risks
and boost consumer confidence that their policies will eventually pay out, if
needed.
Consumers may hesitate to purchase private insurance because some of the
premiums pay for benefits that Medicaid would provide in the absence of private
insurance. Two Medicaid features, in particular, create an implicit tax on private
insurance: (1) private benefits postpone the time at which the asset test for Medicaid
eligibility is met, and (2) Medicaid is secondary payor, i.e., pays only for services
that other insurance do not cover. Public-private partnerships may offer solutions,
such as expansion of state Medicaid Partnership Programs (see Section 4 above).
State Medicaid Partnership Programs make it easier to qualify for Medicaid for
people with high-quality long-term care insurance. Should all benefits under
private long-term care insurance become exhausted, the policyholder may
retain assets equal to benefits paid and still qualify for Medicaid. This modified
asset test addresses the first Medicaid feature responsible for an implicit tax
on private insurance. Under State Medicaid Partnership Programs, the
Medicaid program faces reduced expenditures on long-term care and
consumers can maintain a higher consumption level or leave a bequest.
Similarly, a solution may lie in high-deductible, catastrophic LTCI with private
front-end expense coverage for a set period (1-2 years), and public back-end
coverage paid for the remainder of the LTC need. This would address the
second Medicaid feature responsible for an implicit tax.
While State Medicaid Partnership Programs and high-deductible LTCI policies each
address Medicaid features responsible for an implicit tax on private insurance, few if
any options appear available that fully eliminate the tax while simultaneously
preserving a safety net for low-income Americans and ensuring fiscal sustainability of
the Medicaid program.
Finally, incentives to expand private insurance could be introduced in the workplace.
Allow withdrawals from employer-sponsored retirement plans for LTC
expenses or the purchase of LTCI without early-distribution penalties.
Promote employer-sponsored long-term insurance by allowing plans to be
tax-qualified, so that premiums can be paid through pre-tax payroll
deductions.
To alleviate fiduciary liability and other employer concerns, an alternative
may be to create a publicly run marketplace in which private insurers offer
long-term care insurance that workers may purchase through payroll
deductions. Such an initiative could be modeled on recent state initiatives
with respect to auto-enrollment IRAs.

28
REFERENCES
AALTCI. 2015. “Long-Term Care Insurance Facts – Statistics.” American Association
for Long-Term Care Insurance. Available at http://www.aaltci.org/long-term-
care-insurance/learning-center/fast-facts.php.
AALTCI. 2016a. “Long Term Care Insurance Partnership Plans.” American Association
for Long-Term Care Insurance. Available at http://www.aaltci.org/long-term-
care-insurance/learning-center/long-term-care-insurance-partnership-plans.php.
AALTCI. 2016b. “Types of Group Long-Term Care Insurance Coverage.” American
Association for Long-Term Care Insurance. Available at
http://www.aaltci.org/group-long-term-care-insurance-plans/true-group-ltc.php.
AARP. 2012. “Long-Term Care Insurance: 2012 Update.” AARP Public Policy Institute,
Fact Sheet 261, June 2012. Available at
http://www.aarp.org/content/dam/aarp/research/public_policy_institute/ltc/2012
/ltc-insurance-2012-update-AARP-ppi-ltc.pdf.
BLS. 2016. Consumer Price Index, All Urban Consumers, series CUUR0000SA0 (All
Items) and CUUR0000SAM (Medical Care). Bureau of Labor Statistics. Available
at http://www.bls.gov/data/#prices.
Brown, Jeffrey R. and Amy Finkelstein. 2007. “Why is the Market for Long-Term Care
Insurance So Small?” Working Paper, National Bureau of Economic Research.
http://users.nber.org/~afinkels/papers/Brown_Finkelstein_Small_Feb07.pdf.
Brown, Jeffrey R. and Amy Finkelstein. 2008. “The Interaction of Public and Private
Insurance: Medicaid and the Long-Term Care Insurance Market.” American
Economic Review 98(3): 1083–1102.
Brown, Jeffrey R. and Amy Finkelstein. 2009. “The Private Market for Long-Term
Care Insurance in the United States: A Review of the Evidence.” Journal of Risk
and Insurance, 76(1): 5-29.
Brown, Jeffrey R. and Amy Finkelstein. 2011. “Insuring Long-Term Care in the United
States.” Journal of Economic Perspectives, Volume 25(4): 119–142.
California DHCS. 2010. “Asset protection: A Special Benefit Created for Californians.”
California Department of Health Care Services. Available at http://www.dhcs.ca.
gov/services/ltc/Documents/CPLTC%20Print%20Locks/Asset_2010.pdf.
Carrns, Ann. 2014. “Premiums Rise for Long-Term Care Insurance. Keep It or Drop
It?” New York Times, March 21, 2014.
CBO. 2013. “Rising Demand for Long-Term Services and Supports for Elderly
People.” Congressional Budget Office, June 2013. Available at
https://www.cbo.gov/sites/default/files/113th-congress-2013-
2014/reports/44363-LTC.pdf.
Census Bureau. 2012. “Americans with Disabilities: 2010.” U.S. Census Bureau,
Household Economic Studies. July 2012. Available at
http://www.census.gov/prod/2012pubs/p70-131.pdf.
CIPR. 2016. “The State of Long-Term Care Insurance: The Market, Challenges and
Future Innovations.” Eric Nordman (ed). National Association of Insurance
Commissioners and The Center for Insurance Policy and Research, May 2016.

29
Available at http://www.naic.org/documents/cipr_current_study_160519_
ltc_insurance.pdf.
CMS. 2015. Final Rule, Prospective Payment System and Consolidated Billing for
Skilled Nursing Facilities (SNFs) for FY 2016. August 4, 2015. Federal Register
Vol. 80, No. 149, pages 46390-46477.
Cohen, Marc. 2016. “The State of the Long-Term Care Insurance Market.” Included
in CIPR (2016).
Davidson, Joe. 2016. “Costs Skyrocket for Feds’ Long-Term-Care Insurance.” The
Washington Post, July 21, 2016.
Favreault, Melissa and Judith Dey. 2016. “Long-Term Services and Supports for
Older Americans: Risks and Financing.” U.S. Department of Health and Human
Services, Office of the Assistant Secretary for Planning and Evaluation, Office of
Disability, Aging and Long-Term Care Policy. ASPE Issue Brief, February 2016.
Available at https://aspe.hhs.gov/sites/default/files/pdf/106211/ElderLTCrb-
rev.pdf.
Finkelstein, Amy and Kathleen McGarry. 2006. “Multiple Dimensions of Private
Information: Evidence from the Long-Term Care Insurance Market.” The
American Economic Review 96(4): 938-958.
Florida AHCA. 2015. “Medicaid Reimbursement Per Diem Rates.” Florida Agency for
Health Care Administration. January 1, 2015. Available at
http://ahca.myflorida.com/Medicaid/cost_reim/pdf/2015_01_Rate_Letters.pdf.
Genworth. 2015. “Genworth 2015 Cost of Care Survey.” Genworth Financial, Inc.
Available at https://www.genworth.com/dam/Americas/US/PDFs/Consumer/
corporate/130568_040115_gnw.pdf.
Gleckman, Howard. 2013. “More Bad News for Long-Term Care Insurance: A Major
Carrier Reassess the Business amidst More Rate Hikes.” Forbes, August 8, 2013.
Available at http://www.forbes.com/sites/howardgleckman/2013/08/08/more-
bad-news-for-long-term-care-insurance-a-major-carrier-reassess-the-business-
amidst-more-rate-hikes.
Gleckman, Howard. 2014. “What Does Genworth’s Bad News Mean for the Future of
Long-Term Care Insurance?” November 19, 2014. Available at
http://howardgleckman.com/2014/11/genworths-terrible-news-mean-future-
long-term-care-insurance.
Gleckman, Howard. 2015. “The Long-Term Care Insurance Industry Ponders Its
Future: Seven Trends to Watch.” Forbes, April 9, 2015. Available at
http://www.forbes.com/sites/howardgleckman/2015/04/09/the-long-term-care-
insurance-industry-ponders-its-future-seven-trends-to-watch.
HCRIS. Various years. Healthcare Cost Report Information System. Centers for
Medicare and Medicaid Services. Available at https://www.cms.gov/Research-
Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Cost-Reports.
Kaiser Family Foundation. 2013. “Overview of Nursing Facility Capacity, Financing,
and Ownership in the United States in 2011.” Available at
https://kaiserfamilyfoundation.files.wordpress.com/2013/06/8456-overview-of-
nursing-facility-capacity.pdf.
Karapiperis, Dimitris and Eric Nordman. 2016. “Forward” and “Long-Term Care
Insurance Study Conclusion.” Included in CIPR (2016).

30
Lakdawalla, Darius, Dana Goldman Jayanta Bhattacharya. 2004. “Are the Young
Becoming More Disabled?” Health Affairs, 23(1): 168-176.
Lakdawalla, Darius, Dana Goldman, Jayanta Bhattacharya, Michael Hurd, Geoffrey
Joyce, and Constantijn Panis. 2003. “Forecasting the Nursing Home Population,”
Medical Care, 41(1): 8-20.
Manton, Kenneth. 2003. “Forecasting the Nursing Home Population: Point.” Medical
Care 41(1): 21-24.
MetLife. 2012. "Market Survey of Long-Term Care Costs: The 2012 MetLife Market
Survey of Nursing Home, Assisted Living, Adult Day Services, and Home Care
Costs." MetLife Mature Market Institute, November 2012. Available at
https://www.metlife.com/assets/cao/mmi/publications/studies/2012/studies/mmi
-2012-market-survey-long-term-care-costs.pdf.
NAIC. 2013. “A Shoppers Guide to Long-Term Care Insurance.” National Association
of Insurance Commissioners. Revised 2013. Available at
http://www.naic.org/documents/prod_serv_consumer_ltc_lp.pdf.
NAIC. 2016. “Long-Term Care.” National Association of Insurance Commissioners.
February 5, 2016. Available at
http://www.naic.org/cipr_topics/topic_long_term_care.htm.
NCHS. 2013 “Long-Term Care Services in the United States: 2013 Overview.”
National Center for Health Statistics. Available at
http://www.cdc.gov/nchs/data/nsltcp/long_term_care_services_2013.pdf.
New York SPLTC. 2016. “State Partnership Programs and Reciprocity.” New York
State Partnership for Long-Term Care. Available at
http://www.nyspltc.org/reciprocitymap.htm.
Pincus, Jeremy, Katherine Wallace-Hodel, and Katey Brown. 2013. “Size of the
Employer and Self-Employed Markets Without Access to Long-Term Care
Coverage Options.” The SCAN Foundation. Available at
http://www.thescanfoundation.org/sites/default/files/tsf_ltc-financing_size-
employer-market_pincus_3-20-13.pdf.
Wolf, Adam. 2014. “Surprise! Your long-term care insurance won’t cover it.”
MarketWatch, February 3, 2014. Available at
http://www.marketwatch.com/story/surpise-your-long-term-care-insurance-
wont-cover-it-2014-02-03.

31
APPENDIX A. MEDIAN PRICES OF LONG-TERM CARE
SERVICES, BY STATE (2015)
Nursing home room Assisted
private
($/day)
semi-
private
($/day)
living
facility
($/month)
Adult day
care
($/day)
Home health
aid care
($/hour)
Alabama 209 191 3,075 36 17
Alaska 771 771 5,703 122 26
Arizona 233 192 3,418 80 20
Arkansas 180 155 3,063 80 17
California 285 245 3,750 77 23
Colorado 256 230 3,750 65 22
Connecticut 435 400 5,575 78 22
Delaware 323 300 5,745 69 22
District of Columbia 270 270 7,838 99 22
Florida 265 240 3,150 65 19
Georgia 195 183 2,880 60 18
Hawaii 370 342 4,000 66 25
Idaho 243 228 3,240 116 20
Illinois 204 178 4,050 68 22
Indiana 250 215 3,693 80 20
Iowa 187 175 3,500 60 23
Kansas 180 165 4,188 80 20
Kentucky 239 208 3,350 67 19
Louisiana 170 155 3,010 63 16
Maine 295 275 4,800 108 22
Maryland 302 278 3,900 79 20
Massachusetts 382 353 5,300 65 25
Michigan 272 249 3,250 80 21
Minnesota 263 231 3,468 78 25
Mississippi 220 205 3,150 35 17
Missouri 167 153 2,525 80 19
Montana 220 210 3,560 95 23
Nebraska 218 197 3,628 56 23
Nevada 270 236 3,238 70 22
New Hampshire 335 316 5,103 65 24
New Jersey 350 320 5,725 85 21
New Mexico 234 205 3,500 99 20
New York 374 361 4,100 85 23
North Carolina 225 206 3,000 51 18
North Dakota 288 275 3,239 75 27
Ohio 235 210 3,890 55 20
Oklahoma 165 146 3,345 60 20
Oregon 280 263 3,880 89 23

32
Nursing home room Assisted
private
($/day)
semi-
private
($/day)
living
facility
($/month)
Adult day
care
($/day)
Home health
aid care
($/hour)
Pennsylvania 310 289 3,555 60 21
Rhode Island 283 255 5,325 67 25
South Carolina 206 190 3,125 55 19
South Dakota 212 199 3,023 72 23
Tennessee 207 192 3,395 62 18
Texas 188 140 3,545 35 19
Utah 210 175 3,000 89 21
Vermont 288 280 4,020 124 22
Virginia 254 221 3,933 65 19
Washington 289 266 4,625 68 24
West Virginia 295 282 3,500 72 16
Wisconsin 273 247 3,980 65 22
Wyoming 245 220 3,900 50 22
USA 250 220 3,600 69 20
Source: Genworth (2015).

33
APPENDIX B. SAMPLE LONG-TERM CARE INSURANCE
POLICY
This appendix reproduces three key pages of a sample long-term care insurance
policy that Genworth publishes for California. The full sample policy document may
be found at https://www.genworth.com/dam/Americas/US/PDFs/Consumer/Product/
LTC/7052CA_061713_gnw.pdf.
SAMPLE
7052 CA 3
SCHEDULE
Insured Policy Number Policy Effective Date
[John Q. Doe] [XXXXXXX] [7/01/2013]
[Apt #1234]
[1234 Main Street] Issue State
[Anytown, CA 99999] California
COVERAGE FEATURES AND LIMITS
Coverage is provided for Covered Expenses that are incurred after the Elimination Period has been
satisfied. Payment is subject to the limits determined below and all other provisions of the Policy.
Changes in Your Schedule may be made by Rider.
Elimination Period: [[30][90] days of Covered Care]
[The Elimination Period is satisfied by days You incur a Covered Expense while You are Chronically Ill.]
OR [[30][90] calendar days]
[The Elimination Period is satisfied by days You are Chronically Ill beginning with the first day You incur a
Covered Expense.]
[There is no Elimination Period for the Home and Community Care Benefit. In addition, days for which
payment is made under that Benefit will count toward satisfying the Elimination Period.]
Coverage Maximum Nursing Facility Maximum Benefit Increases
[$240,000] [$4,000 per calendar month] [5% Compound]
[See below]
[The Coverage Maximum and amounts based on the Nursing Facility Maximum are: (a) increased when
Benefit Increases apply; and (b) exhausted only when the total of all Benefits paid equals the then
applicable maximum amount. Benefit Increases that apply are not affected by any Benefits paid for
Covered Expenses incurred prior to the date the applicable maximum is exhausted.]
[5%, 3%] Compound Benefit Increases: On each anniversary of the Policy Effective Date Your then
current Nursing Facility Maximum and the current amounts of other dollar maximums will each increase
by the selected percentage.
These Benefit Increases will be automatic; will not require proof of good health; and will be made
without a corresponding increase in Premium. They will continue without regard to Your age, Claim
status or Claim history, or length of time You have been insured under the Policy.
Benefit Increases cease when: (a) the applicable maximum has been exhausted; (b) they are
terminated by You; or (c) the Policy ends.]
[5% Simple Benefit Increases: On each anniversary of the Policy Effective Date Your then current
Nursing Facility Maximum and the current amounts of other dollar maximums will each increase by 5%
of their respective amounts in effect on the Policy Effective Date. Calculation of the increased amounts
is not affected by Benefit payments.
These Benefit Increases will be automatic; will not require proof of good health; and will be made
without a corresponding increase in Premium. They will continue without regard to Your age, Claim
status or Claim history, or length of time You have been insured under the Policy.
Benefit Increases cease when: (a) the applicable maximum has been exhausted; (b) they are
terminated by You; or (c) the Policy ends.]
[5% Future Purchase Options: These provide a way to increase Your Benefit maximums on every 3rd
anniversary of the Policy Effective Date. Increases will not be available or effective, and may be revoked
or rescinded, if You are Chronically Ill or otherwise eligible for Benefits on the date the offer is accepted.
You will be given the option to purchase additional coverage equal to 5% compounded annually for the
3 year period (an approximate increase of 15.8%). The increases will apply to Your then current Nursing
Facility Maximum and the current amounts of other dollar maximums. The additional Premium for an
increase will be based on: (1) the amount of the increase; and (2) Your age and the Premium in effect
for the Policy on the date the increase takes effect.
Offers and Benefit Increases cease when: (a) You have refused/declined three consecutive options to
increase Benefit maximums; (b) the applicable maximum has been exhausted; (c) they are terminated
by You; or (d) the Policy ends. ]
SAMPLE COPY
SAMPLE
7052 CA 3A
SCHEDULE
(Continued)
We Pay [the Covered Percentage of]
Covered Expenses Up to these Limits
Benefits and Services Provided (except where otherwise noted)
Privileged Care Coordination Services ...................... Not subject to coverage limits
Nursing Facility Benefit .............................................. Nursing Facility Maximum per [day][calendar month]
Residential Care Facility Benefit ................................ [[75%][100%] of the] Nursing Facility Maximum
per [day][calendar month]
Bed Reservation Benefit ............................................ 60 days per calendar year
Home and Community Care Benefit .......................... [[50%][100%] of the] Nursing Facility Maximum
per [day] [calendar month]]
Home Assistance Benefit ........................................... A Policy total payment maximum equal to
(Equipment, modifications & training) [[3 times Monthly][90 times Daily] the Nursing
Facility Maximum]
Hospice Care Benefit ................................................. Included
Respite Care Benefit .................................................. 30 days per calendar year
International Coverage Benefit .................................. As stated in the Benefit
Waiver of Premium Benefit ........................................ Included
The Waiver of Premium applies only during periods for which Benefits are payable under the: Nursing
Facility Benefit; Residential Care Facility Benefit; Bed Reservation Benefit; Home and Community
Care Benefit; or Hospice Care Benefit.
[This also applies when Your Spouse or Partner for Shared Coverage qualifies for Waiver of Premium
under this Policy or his or her Policy.]
Your Right To Request Payment
For Alternative Care ............................................ Payment subject to mutual agreement
Contingent Nonforfeiture Benefit ................................ Included
The following Riders are attached to, and included in, the Policy.
[Nonforfeiture Benefit ................................................. Included]
[Shared Coverage Benefit .......................................... Included with Joint Waiver]
[Restoration Benefit .................................................... Included]
[Transition Benefit ...................................................... A Policy total payment maximum equal to
[5 times][20% of] the Nursing Facility Maximum]
The maximum total amount payable for all Covered Expenses incurred [on a day] [in a calendar month] is
limited to the Nursing Facility Maximum. This does not apply to the Home Assistance Benefit and Benefits
paid for requested alternative care.
SAMPLE COPY

SAMPLE
7052 CA 3B
SCHEDULE
(Continued)
PREMIUM DATA
Annual Premium
Basic Policy Coverage ............................................................................................... $XXX.XX
[Nonforfeiture Benefit Rider .......................................................................................... $XX.XX]
[Shared Coverage Rider ............................................................................................... $XX.XX
Spouse or Partner for Shared Coverage Mary Jane Doe]
[Restoration Benefit Rider ............................................................................................ $XX.XX]
[Transition Benefit Rider ............................................................................................... $XX.XX]
[Premium Credit for Replacement of Prior Coverage With Us ..................................... $XX.XX]
Total Annual Premium ............................................................................................... $XXX.XX]
First Premium Premium Payment Mode Modal Premium
[$aaa.aa] [Quarterly] [$bbb.bb]
Premium for Premium Payment Modes other than annual are the following percentage of the Annual
Premium:
Semi-Annual = 51%; Quarterly = 26%; Monthly = 9%
The following table shows the Modal Premium and total yearly cost for the available Premium Payment
Modes for the Annual Premium that applies on the Policy Effective Date. These costs will change when
there is a change in Your Premium. See the Modal Premium Disclosure for additional information.
Total First Year Premium Payment Options (including all optional Coverage)
Annual
Semi-Annual
Quarterly
Monthly
Modal Premium
$[XXX.XX]
$[XXX.XX]
$[XXX.XX]
$[XXX.XX]
Total Yearly Cost for First Year
Premium
$[XXX.XX]
$[XXX.XX]
$[XXX.XX]
$[XXX.XX]
Premium Payment Period: Lifetime
Rating: [Standard] [with [Insured] Couples Discount]
SAMPLE COPY

37
This document is the Final Report, Deliverable 2c pursuant to Task Order
DOL-OPS-15-T-00168 (Long-Term Care Study) under Contract DOL-OPS-14-D-0021.
DISCLAIMER
The views, opinions, and/or findings contained in this report are those of the authors
and should not be construed as an official Government position, policy or decision,
unless so designated by other documentation issued by the appropriate
governmental authority.
We call your attention to the possibility that other professionals may perform
procedures concerning the same information or data and reach different findings
than Advanced Analytical Consulting Group, Inc. (AACG) and Deloitte Financial
Advisory Services LLP (Deloitte) for a variety of reasons, including the possibilities
that additional or different information or data might be provided to them that was
not provided to AACG and Deloitte, that they might perform different procedures
than did AACG and Deloitte, or that professional judgments concerning complex,
unusual, or poorly documented matters may differ.
This document contains general information only. AACG and Deloitte are not, by
means of this document, rendering business, financial, investment, or other
professional advice or services. This document is not a substitute for such
professional advice or services, nor should it be used as a basis for any decision or
action. Before making any decision or taking any action, a qualified professional
adviser should be consulted. AACG and Deloitte, its affiliates, or related entities shall
not be responsible for any loss sustained by any person who relies on this
publication.
