2019
National Prole
of Local Health Departments

Public health is at the forefront of public attention and discourse worldwide in a way that is unparalleled in modern
times. COVID-19 brought the normally hidden work of public health into the limelight and has held it there with a
variety of fascinating results. “Epidemiologist” is now a common word, news outlets routinely discuss the merits of
population testing metrics, and for months, the nation tuned into briengs by the White House Coronavirus Task Force
headed byVice President Pence.
During the pandemic, data from the National Prole of Local Health Departments (Prole) studies have been in great
demand. The data have been highlighted by NACCHO and its national partners in communications to policymakers,
aswell as featured in newspapers, magazines, and newscasts all over the country.
Prole data are an incredible source of context for the current COVID-19 pandemic response. In fact, the Prole study
is the only longitudinal study of its kind focused on the infrastructure and practice of local health departments (LHDs).
As such, it highlights the impact of the continued underfunding of public health around the country. As health
departments tackle the largest pandemic in modern history, the workforce is strained, resources are redirected to
the response, essential services are disrupted, and leaders are faced with political pressures ranging from rings to
deaththreats.
In support of LHDs, NACCHO and its funding partners at the Centers for Disease Control and Prevention (CDC) and
the Robert Wood Johnson Foundation (RWJF) remain committed to providing evidence regarding the state of local
public health that is objective, accurate, and useful. To reinforce these eorts, NACCHO is teaming with ZS Associates
and LiveStories to create interactive products that allow LHDs to access their data, compare it to state and regional
benchmarks, and combine it with health and healthcare metrics from other national datasets to create ready-made
reports on their local public health context.
Finally, I want to give special recognition to the NACCHO Prole Team that managed the daily work of the 2019 Prole
study in challenging conditions during the pandemic. They elded hundreds of emergency requests for data; worked
from home during the stay-at-home orders; endured endless Zoom calls with kids, partners, and pets in the background;
staed NACCHO’s Incident Command System in support of the federal response; and still delivered a quality product
ontime.
Aaron Alford
Senior Director, Research & Evaluation
Acknowledgments
NACCHO | 2019 National Prole of Local Health Departments
2

NACCHO is pleased to present the 2019 National Prole of Local Health Departments (Prole) to local health
departments (LHDs), policymakers, public health researchers, and the public health community. The Prole study
is the only one of its kind that collects data about LHD infrastructure and practice at the nationallevel.
LHDs are the backbone of the nation’s public health system as the “boots on the ground” for delivery of public health
services. Our rapidly changing world and crises like the COVID-19 pandemic emphasize the need for timely information
and data to support public health practice, especially at the local level. The Prole study provides accurate and useful
information about LHDs nationwide that are essential for making data-driven decisions and engaging in evidence-based
services. Such data are especially critical today, as we face national and global challenges that aect the health and
well-being of every community. In an era of unstable funding, LHDs increasingly depend upon reliable and useful data
to help them make dicult choices under sometimes less-than-ideal operating conditions. With data from the Prole
study, the public health community can prevent and combat disease and health inequities and make sound decisions
toimprove and enhance the physical and mental health of every individual.
The key to unleashing the power of data is action. Using data to drive decision-making is one of the best recommended
uses of this Prole. NACCHO looks forward to working with all of its diverse stakeholders in public health to continue
identifying new and interesting ways to use this powerful dataset to drive additional research, inuence important
policies, educate others on the importance of local governmental public health, and demonstrate the impact of public
health in communities across our country.
Jennifer Kertanis Lori Tremmel Freeman
President, NACCHO Chief Executive Ocer, NACCHO
NACCHO | 2019 National Prole of Local Health Departments
3

Our nation’s experience with the COVID-19 pandemic
and previous public health emergencies has revealed
how critically important it is to collect inclusive
health data at the community level. NACCHO’s Prole
study provides the only comprehensive picture of
activities, workforce, funding, and priorities of local
health departments (LHDs) across the country.
These data are key for decision-makers seeking
evidence-based support to address the unique
needs of their specic communities. It’s my hope
this report will encourage policymakers to begin
collecting even more equity-focused data, with
the goal of supporting the infrastructure, funding,
stang, and programming of our nation’s LHDs in
ways that provide everyone in America a fair and just
opportunity for health andwell-being.
Richard E. Besser
President and CEO
Robert Wood Johnson Foundation (RWJF)
The Centers for Disease Control and Prevention
(CDC) is pleased to support NACCHO and its work
on the National Prole of Local Health Departments
(Prole) study. This 2019 Prole report is a valuable
resource for all public health professionals,
policymakers, federal agencies, researchers, and
others to use to understand our nation’s current local
public health infrastructure. The work of local health
departments is critical in protecting the health of
the community. I would like to commend NACCHO
and the local health departments who provided
these data, and their dedication and contribution
topublichealth.
Robert R. Redeld, MD
Director
Centers for Disease Control and Prevention (CDC)
NACCHO | 2019 National Prole of Local Health Departments
4

National Prole of Local Health Departments Workgroup Members
Betty Bekemeier, PhD, MPH, MSN, FAAN
University of Washington
Bonnie Bruesho, RN, DNP, PHN
Dakota County Public Health Department
Maggie Carlin, MPH
Association of State and Territorial Health Ocials
Glenn Czarnecki, MPA
Tennessee Department of Health, Southeast Region
Jenine Harris, PhD
Washington University in St. Louis
Alannah Kittle, MPH
Association of State and Territorial Health Ocials
Ruth Maiorana
Maryland Association of County Health Ocers
Doug Mathis, MA
Henry County Health Department
NACCHO Prole Team
Aaron Alford, PhD, MPH, PMP
Senior Director of Research & Evaluation
Debra Dekker, PhD
Director of Evaluation
Karla Feeser, MPH
Senior Research Analyst
Kellie Hall, MSOD
Senior Research & Evaluation Specialist
Shaunna Newton, MPH
Senior Research & Evaluation Specialist
Carolyn Miller, MSHP, MA
Robert Wood Johnson Foundation
Carol Moehrle, RN, BSN
Idaho Department of Health and Welfare, North Central District
Jacquelynn Orr, DrPH, MHA
Robert Wood Johnson Foundation
Sergey Sotnikov, PhD
Centers for Disease Control and Prevention
Oktawia Wójcik, PhD
Robert Wood Johnson Foundation
Susan Zahner, DrPH, RN, FAAN
University of Wisconsin
Carlos Zometa, PhD
Centers for Disease Control and Prevention
(Those acknowledged served as a workgroup member during 2018, 2019,
or 2020.)
Jonathan P. Leider, PhD
Consultant
NACCHO would also like to acknowledge the following
people for their work on the 2019 Prole study:
Nathalie Robin, MPH
Previous Senior Research Analyst
Kari O’Donnell, MA
Previous Research & Evaluation Specialist
Johnnetta Davis-Joyce, MA
Previous Senior Director of Research & Evaluation
NACCHO | 2019 National Prole of Local Health Departments
5

Contents
CHAPTER 1
Introduction ........................................................................................................................... 11
CHAPTER 2
Jurisdiction and Governance .......................................................................................... 20
CHAPTER 3
Partnerships ........................................................................................................................... 28
CHAPTER 4
Leadership .............................................................................................................................. 39
CHAPTER 5
Workforce ................................................................................................................................ 47
CHAPTER 6
Finance .................................................................................................................................... 64
CHAPTER 7
Programs and Services ...................................................................................................... 75
CHAPTER 8
Emergency Preparedness andResponse ................................................................... 97
CHAPTER 9
Assessment, Planning, andAccreditation ................................................................106
CHAPTER 10
Quality Improvement andWorkforce Development ...........................................118
CHAPTER 11
Public Health Policy ..........................................................................................................127
CHAPTER 12
Informatics............................................................................................................................137
NACCHO | 2019 National Prole of Local Health Departments
6

Figures
Chapter 1
Introduction
1.1 | Questionnaire topics, by questionnaire type and response rate .............................................................................................................. 14
1.2 | Number of LHDs in study population and number of respondents, by state ............................................................................................. 15
1.3 | Number of LHDs in study population and number of respondents, by size of population served .................................................................. 16
Chapter 2
Jurisdiction and Governance
2.1 | Size of population served by LHDs in the study population ................................................................................................................... 21
2.2 | Percent of United States population served by LHDs ............................................................................................................................ 22
2.3 | Geographic jurisdictions served by LHDs, by size of population served .................................................................................................... 23
2.4 | Type of LHD governance, by state ..................................................................................................................................................... 24
2.5 | LHDs as a part of a combined Health and Human Services Agency (HHSA), by state ................................................................................... 25
2.6 | LHDs with a local board of health (LBOH), by size of population served and type of governance ................................................................... 26
2.7 | Functions that local boards of health (LBOHs) utilize on a continuous basis .............................................................................................. 27
Chapter 3
Partnerships
3.1 | Cross-jurisdictional sharing of services, by size of population served and type of governance ...................................................................... 29
3.2 | Type of cross-jurisdictional sharing of services .................................................................................................................................... 30
3.3 | LHD partnerships and collaborations in the past year ........................................................................................................................... 31
3.4 | Formal* LHD partnerships and collaborations, over time ....................................................................................................................... 32
3.5 | Direction of information exchange between LHDs and partner organizations in the past year ...................................................................... 33
3.6 | Engagement with academic institutions in the past year, by size of population served................................................................................ 34
3.7 | Engagement with academic institutions in the past year, by degree of urbanization ................................................................................... 35
3.8 | Engagement with specic academic institutions in the past year ............................................................................................................ 36
3.9 | Number of research studies in which LHDs participated during the past year, by size of population served and degree of urbanization ............... 37
3.10 | Participation in research activities during the past year, by size of population served ................................................................................ 38
Chapter 4
Leadership
4.1 | Characteristics of LHD top executives ................................................................................................................................................ 40
4.2 | Age of LHD top executives, over time ................................................................................................................................................ 41
4.3 | Tenure of LHD top executives, over time ............................................................................................................................................ 42
4.4 | Average tenure (in years) of LHD top executives, over time and by size of population served ....................................................................... 43
4.5 | Highest degree obtained by LHD top executive, by size of population served and degree of urbanization ...................................................... 44
4.6 | Specialized degrees obtained by LHD top executive, by size of population served and degree of urbanization ................................................ 45
4.7 | Characteristics of new versus experienced LHD top executives ............................................................................................................... 46
NACCHO | 2019 National Prole of Local Health Departments
7

Figures
Chapter 5
Workforce
5.1 | Number of Full-Time Equivalents (FTEs) ............................................................................................................................................. 48
5.2 | Mean and median number of employees and Full-Time Equivalents (FTEs), by size of population served ........................................................ 49
5.3 | Full-Time Equivalents (FTEs) per 10,000 people, by size of population served ............................................................................................ 50
5.4 | Estimated size of the LHD workforce ................................................................................................................................................. 51
5.5 | Distribution of Full-Time Equivalents (FTEs), by degree of urbanization .................................................................................................... 52
5.6 | Estimated size of LHD workforce, over time ........................................................................................................................................ 53
5.7 | Full-Time Equivalents (FTEs) per 10,000 people, over time and by size of population served ......................................................................... 54
5.8 | LHD workforce that retired, over time ................................................................................................................................................ 55
5.9 | Occupations employed at LHDs, by size of population served ................................................................................................................ 56
5.10 | Stang patterns (in median Full-Time Equivalents (FTEs)) at LHDs, by size of population served ................................................................. 57
5.11 | Estimated number of Full-Time Equivalents (FTEs) in select occupations ................................................................................................. 58
5.12 | Workforce composition ................................................................................................................................................................. 59
5.13 | Estimated size of select occupations, over time.................................................................................................................................. 60
5.14 | Job losses among LHDs due to layos and/or attrition in the past year, by size of population served andtype of governance .......................... 61
5.15 | Job losses among LHDs due to layos and/or attrition, over time .......................................................................................................... 62
5.16 | Number of jobs lost and added, over time and by size of population served............................................................................................ 63
Chapter 6
Finance
6.1 | Total annual expenditures ............................................................................................................................................................... 65
6.2 | Mean and quartiles of total annual expenditures ................................................................................................................................. 66
6.3 | Median and quartiles of annual per capita expenditures and revenues, by size of population served and type of governance ............................ 67
6.4 | Overall median annual expenditures per capita, by state ....................................................................................................................... 68
6.5 | Median and mean annual per capita expenditures, over time................................................................................................................. 69
6.6 | Revenue sources ........................................................................................................................................................................... 70
6.7 | Median and mean annual per capita revenue sources, by LHD characteristics ........................................................................................... 71
6.8 | Median and mean annual per capita revenue sources, over time ............................................................................................................ 72
6.9 | Changes in LHD budgets, over time .................................................................................................................................................. 73
6.10 | Percent of LHD’s budget cut in the current scal year compared to the previous scal year ........................................................................ 74
Chapter 7
Programs and Services
7.1 | Clinical programs and services provided directly by LHDs in the past year ................................................................................................ 76
7.2 | Population-based programs and services provided directly by LHDs in the past year .................................................................................. 77
7.3 | Adult and child immunization services provided directly by LHDs in the past year, by size of population served and degree of urbanization ........ 78
7.4 | Screening and treatment for diseases and conditions provided directly by LHDs in the past year,
by size of population served and degree of urbanization ...................................................................................................................... 79
7.5 | Maternal and child health services provided directly by LHDs in the past year, by size of population served and degree of urbanization .............. 80
7.6 | Other clinical services provided directly by LHDs in the past year, by size of population served and degree of urbanization ............................... 81
7.7 | Epidemiology and surveillance services provided directly by LHDs in the past year, by size of population served and degree of urbanization ....... 82
NACCHO | 2019 National Prole of Local Health Departments
8

Figures
7.8 | Population-based primary prevention services provided directly by LHDs in the past year, by size of population served and degree of urbanization ....... 83
7.9 | Regulation, inspection, or licensing services provided directly by LHDs in the past year, by size of population served and degree of urbanization ...... 84
7.10 | Environmental health services provided directly by LHDs in the past year, by size of population served and degree of urbanization .................. 85
7.11 | Other population-based services provided directly by LHDs in the past year, by size of population served and degree of urbanization .............. 86
7.12 | Number of services contracted out by LHDs, by size of population served .............................................................................................. 87
7.13 | Programs and services provided most frequently via contracts ............................................................................................................. 88
7.14 | Provision of population-based primary prevention services by other organizations independent of LHD funding .......................................... 89
7.15 | Programs and services more likely to be provided in rural jurisdictions .................................................................................................. 90
7.16 | Programs and services more likely to be provided in urban jurisdictions................................................................................................. 91
7.17 | Change in percent of LHDs providing clinical programs and services since 2008 ...................................................................................... 92
7.18 | Change in percent of LHDs providing population-based programs and services since 2008 ....................................................................... 93
7.19 | Changes in provision of services in the past year ................................................................................................................................ 94
7.20 | Growing, stable, and shrinking services in the past year ...................................................................................................................... 95
7.21 | Changes in provision of services, by changes in budgets in the past year ................................................................................................ 96
Chapter 8
Emergency Preparedness andResponse
8.1 | Changes in LHD budgets for emergency preparedness activities, by size of population served and census region ........................................... 98
8.2 | Funding sources for emergency preparedness activities ....................................................................................................................... 99
8.3 | Response to specic all-hazards events in the past year, over time .........................................................................................................100
8.4 | Response to specic all-hazards events in the past year, by size of population served ................................................................................101
8.5 | Response to specic all-hazards events in the past year, by census region ...............................................................................................102
8.6 | Number of LHD responses to specic all-hazards events in the past year .................................................................................................103
8.7 | Use of select volunteer groups in emergency preparedness activities .....................................................................................................104
8.8 | Use of select volunteer groups in emergency preparedness activities, over time ....................................................................................... 105
Chapter 9
Assessment, Planning, andAccreditation
9.1 | Participation over time in a community health assessment (CHA), community health improvement plan (CHIP),
and/or strategic plan (SP) within ve years ........................................................................................................................................107
9.2 | Participation in a community health assessment (CHA), community health improvement plan (CHIP), and/or strategic plan (SP)
within ve years, by size of population served .................................................................................................................................... 108
9.3 | Data included in most recent community health assessment (CHA), over time .........................................................................................109
9.4 | Use of tools for most recent community health improvement plan (CHIP) ...............................................................................................110
9.5 | Actions taken in the past three years to implement or sustain a community health improvement plan (CHIP), over time .................................. 111
9.6 | Level of collaboration with non-prot hospitals on most recent community health needs assessment(CHNA) ...............................................112
9.7 | Types of collaboration with non-prot hospitals on most recent community health needs assessment(CHNA) ..............................................113
9.8 | Level of engagement with Public Health Accreditation Board (PHAB) accreditation in 2019 ........................................................................114
9.9 | Level of engagement with Public Health Accreditation Board (PHAB) accreditation, over time ....................................................................115
9.10 | Formal engagement in Public Health Accreditation Board (PHAB) accreditation, over time and by size ofpopulation served ........................... 116
9.11 | Reasons for not pursuing Public Health Accreditation Board (PHAB) accreditation ................................................................................... 117
NACCHO | 2019 National Prole of Local Health Departments
9

Figures
Chapter 10
Quality Improvement andWorkforce Development
10.1 | Level of quality improvement (QI) implementation, over time .............................................................................................................119
10.2 | Level of quality improvement (QI) implementation, by size of population served ....................................................................................120
10.3 | Number of quality improvement (QI) projects implemented in the past year .......................................................................................... 121
10.4 | Number of quality improvement (QI) projects implemented in the past year, by level of QI implementation ................................................122
10.5 | Elements of an agency-wide quality improvement (QI) program currently in place at LHD, over time .......................................................... 123
10.6 | Use of any competency sets for workforce development, planning, and action ....................................................................................... 124
10.7 | Use of the Core Competencies for Public Health Professionals .............................................................................................................125
10.8 | Use of the Core Competencies for Public Health Professionals, over time ............................................................................................... 126
Chapter 11
Public Health Policy
11.1 | Involvement in policy areas in the past two years, by size of population served ......................................................................................128
11.2 | Involvement in select policy areas, over time....................................................................................................................................129
11.3 | Involvement in policy areas related to tobacco, alcohol, opioids, or other drugs in the past two years, bysize of population served..................130
11.4 | Involvement in policy areas related to tobacco, alcohol, opioids, or other drugs in the past two years, bydegree of urbanization .....................131
11.5 | Involvement in policy areas related to tobacco, alcohol, or other drugs, over time ...................................................................................132
11.6 | Involvement in developing new or revising existing ordinances in the past two years, byLHDcharacteristics...............................................133
11.7 | Topic areas of new or revised ordinances in the past two years ............................................................................................................134
11.8 | Engagement in assuring access to healthcare services in the past year .................................................................................................. 135
11.9 | Engagement in assuring access to healthcare services, over time ......................................................................................................... 136
Chapter 12
Informatics
12.1 | Level of activity in information technology systems ...........................................................................................................................138
12.2 | Implementation of information technology systems, by size of population served ..................................................................................139
12.3 | Implementation of information technology systems, over time ...........................................................................................................140
12.4 | Organizations involved in information management for LHDs .............................................................................................................141
12.5 | Use of communication channels for general or emergency response communications ............................................................................142
12.6 | Any use of communication channels, by size of population served ....................................................................................................... 143
12.7 | Any use of communication channels, by type of governance ..............................................................................................................144
12.8 | Any use of communication channels, by degree of urbanization ..........................................................................................................145
12.9 | Any use of communication channels, over time ................................................................................................................................146
NACCHO | 2019 National Prole of Local Health Departments
10

This chapter includes the following:
Study background and methods.
Questionnaire topics.
Number of local health departments (LHDs)
instudy population.
Denitions of LHD jurisdiction size, type of
governance, census regions, and urbanization.
Introduction
CHAPTER 1

The National Association of County and City Health Ocials (NACCHO) conducted the rst National Prole of Local
Health Departments (Prole) study from 1989 to 1990. This study helped to dene a local health department (LHD) and
describe how funding, stang, governance, and activities of LHDs vary across the United States. In the three decades
since, NACCHO has conducted an additional eight Prole studies, including in 2019. All Prole studies have been funded
by the Centers for Disease Control and Prevention (CDC); beginning in 2007, NACCHO has also received funding from
the Robert Wood Johnson Foundation (RWJF).
Purpose
The purpose of the Prole study is to develop a comprehensive and accurate description of LHD infrastructure and
practice. Data from the Prole study are used by many people and organizations across the United States. For example,
LHD sta use the data to compare their LHD to others within their state or the nation; data are used to inform public
health policy at the local, state, and federal levels and can support projects to improve local public health practice; and
data are used in universities to educate the future public health workforce about LHDs and by researchers to address
questions about public health practice. NACCHO sta use Prole data to develop programs and resources that meet
the needs of LHDs and to advocate eectively for LHDs. NACCHO also generates Geographic Information System (GIS)
shapeles and denitions of Prole study LHD jurisdictions that support visual description and denition of LHDs for
researchers and policymakers.
Study Methodology
Study population
Every Prole study uses the same denition of an LHD: an administrative or service unit of local or state government,
concerned with health, and carrying some responsibility for the health of a jurisdiction smaller than the state. There
are approximately 2,800 agencies or units that meet the Prole denition of an LHD. Some states have a public health
system structure that includes both regional and local oces of the state health agency. In those states, the state health
agency chooses to respond to the Prole survey at either the regional or local level, but not at both levels.
NACCHO uses a database of LHDs based on previous Prole studies and consults with state health agencies and State
Associations of Local Health Ocials (SACCHOs) to identify LHDs for inclusion in the study population. For the 2019
Prole study, a total of 2,459 LHDs were included in the study population. Rhode Island was excluded from the study
because the state health agency operates on behalf of local public health and has no sub-state units. For the rst time,
Hawaii wasincluded.
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
12

Sampling
All LHDs in the study population received a common set of questions, called the the Core questionnaire. A randomly
selected group of LHDs also received one of the two sets of supplemental questions (or modules). LHDs were selected
to receive the Core questionnaire only or the Core plus one of the two modules using stratied random sampling
(without replacement), with strata dened by the size of the population served by the LHD. The module sampling
process is designed to produce national estimates but not to produce state-level estimates.
Questionnaire development
The NACCHO Prole team developed both the Core and module questionnaires by rst reviewing the 2016 Prole
questionnaires to determine how each question performed among respondents and what questions should be kept,
modied, or deferred to a future Prole questionnaire. The team also reviewed questionnaires from previous years (e.g.,
2013, 2010, 2008, 2005) to identify whether any questions should be repeated in 2019. Lastly, the team developed
new questions based on current public health topics. An advisory group—comprising LHD leaders, sta from aliate
organizations, and researchers—and other subject matter experts within NACCHO provided input and feedback on new
and revised survey questions. Many questions in the Core and module questionnaires have been used in previous Prole
studies and provide an ongoing dataset for comparative analysis; most new items were placed in modules. The Prole
team piloted the questionnaire from December 2018 to January 2019 among 28 LHDs (13 completed it for a response
rate of 46%). NACCHO interviewed select LHDs to assess whether certain sections and questions performed as expected.
The Prole team revised the survey as needed and nalized it for distribution.
Questionnaire distribution
In January 2019, NACCHO sent an e-mail announcement to all 2,459 LHDs in the study population. In the e-mail,
LHDs were given the opportunity to designate another sta person as the primary contact to complete the Prole
questionnaire. NACCHO launched the nal questionnaire from March to August 2019 via an e-mail sent to the
designated primary contacts. The e-mail included a link to a web-based questionnaire, individualized with preloaded
identifying information specic to the LHD. LHDs could print a hard copy version of their Prole questionnaire by using
alink in the questionnaire introduction or could request that NACCHO sta send a copy via e-mail orU.S. mail.
The Prole team conducted extensive eorts to encourage participants to complete the questionnaire. Before and
during the administration period, NACCHO disseminated promotional materials about the survey via NACCHO’s print
and electronic publications (i.e., Public Health Dispatch, NACCHO Connect, NACCHO Voice) and social media channels.
NACCHO sta and a nationwide group of Prole study advocates conducted follow-up with non-respondents using
e-mail messages and telephone calls. NACCHO also oered technical support to survey respondents through an e-mail
address and telephone hotline. The nal response rate for the 2019 Prole study was 61%.
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
13

Figure 1.1 | Questionnaire topics, by questionnaire type and response rate
The 2019 Prole study questionnaire
included a set of questions (Core
questionnaire) sent to all LHDs in the
United States; additional supplemental
questions were grouped into
twomodules.
LHDs were randomly assigned to receive
only the Core questionnaire or the Core
plus one of the two modules.
Many questions in the Core and module
questionnaires have been used in previous
Prole studies and provide an ongoing
dataset for comparative analysis; most new
items were placed in modules.
Core Module 1 Module 2
(Core only response rate = 59%) (Core + Module 1 response rate = 61%) (Core + Module 2 response rate = 65%)
LHD top executive LHD interaction with academic institutions Jurisdiction and governance
Jurisdiction and governance Partnerships and collaboration
Community health assessment
andplanning
Workforce Cross-jurisdictional sharing of services Human resources issues
Stang changes Emergency preparedness Quality improvement
Programs and services Access to healthcare services Public health informatics
Public health policy Guide to Community Preventive Services
Community health assessment
andplanning
Evaluation of Prole
Accreditation
Funding
Changes in LHD budget
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
14

Figure 1.2 | Number of LHDs in study population and number of respondents, by state
Overall, 1,496 LHDs responded to the 2019
Prole study for a response rate of 61%.
Most states had a response rate of 50% or
more, with the exception of Connecticut,
Indiana, Iowa, Massachusetts, Mississippi,
Missouri, Montana, New Mexico,
Oklahoma, and West Virginia.
Alabama, the District of Columbia, Idaho,
Nevada, South Carolina, and Vermont had
response rates of 100%.
State
Total number
of LHDs
Number of
respondents Response rate
All 2,459 1,496 61%
Alabama 66 66 100%
Alaska 2 1 50%
Arizona 15 10 67%
Arkansas 75 71 95%
California 61 34 56%
Colorado 53 27 51%
Connecticut 67 32 48%
Delaware 2 1 50%
District of Columbia 1 1 100%
Florida 67 65 97%
Georgia 18 9 50%
Hawaii 3 2 67%
Idaho 7 7 100%
Illinois 93 76 82%
Indiana 93 34 37%
Iowa 98 44 45%
Kansas 100 52 52%
Kentucky 60 42 70%
Louisiana 10 7 70%
Maine 10 9 90%
Maryland 24 23 96%
Massachusetts 293 110 38%
Michigan 44 28 64%
Minnesota 74 55 74%
Mississippi 3 1 33%
State
Total number
of LHDs
Number of
respondents Response rate
Missouri 114 55 48%
Montana 51 12 24%
Nebraska 19 14 74%
Nevada 3 3 100%
New Hampshire 2 1 50%
New Jersey 92 54 59%
New Mexico 5 2 40%
New York 58 37 64%
North Carolina 85 59 69%
North Dakota 28 27 96%
Ohio 113 61 54%
Oklahoma 70 30 43%
Oregon 33 25 76%
Pennsylvania 16 9 56%
South Carolina 4 4 100%
South Dakota 8 7 88%
Tennessee 95 92 97%
Texas 72 36 50%
Utah 13 7 54%
Vermont 12 12 100%
Virginia 35 20 57%
Washington 35 25 71%
West Virginia 48 22 46%
Wisconsin 86 61 71%
Wyoming 23 14 61%
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
15

Figure 1.3 | Number of LHDs in study population and number of respondents, by size of population served
LHDs serving smaller populations had
lower response rates than did those
serving larger populations.
Because there are relatively few LHDs
serving large populations, the higher
response rates among LHDs serving larger
populations are important for ensuring
that ndings are representative for LHDs in
this category and to the analytic capacity
of the study data.
Size of population served
Total number
of LHDs
Number of
respondents
Response
rate
All 2,459 1,496 61%
<25,000 979 523 53%
25,000–49,999 510 313 61%
50,000–99,999 385 253 66%
100,000–249,999 293 203 69%
250,000–499,999 142 96 68%
500,000–999,999 100 72 72%
1,000,000+ 50 36 72%
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
16

Survey Weights and National Estimates
Unless otherwise stated, national statistics presented were computed using survey weights. NACCHO developed survey
weights for the items from the Core questionnaire to account for dierential non-response by size of population served;
survey weights used to produce statistics from modules also accounted for sampling. By using survey weights, the
Prole study provides national estimates for all LHDs in the United States. Beginning in 2019, we used post-stratication
(based on year and population size) and nite population correction; the condence intervals associated with some
statistics may dier from items published in previous years due to this change.
Longitudinal comparisons for workforce were constructed using NACCHO Prole data from 2008 through 2019. The
2008–2016 workforce estimates reported in 2019 dier from those estimates reported in previous years due to two
factors. First, a small number of LHDs were removed from the analysis over the past years to enhance comparability
through 2019. In 2020, NACCHO created a multi-year dataset to analyze trends for various reasons, including in response
to the COVID-19 crisis. As part of the process, NACCHO conducted an enhanced data review which revealed a very small
number of LHDs with ongoing reporting errors. Though few in number, these LHDs reported more employees and Full-
Time Equivalents (FTEs) than the average respondent in their population size category, thus marginally impacted the
national estimates. Second, 95% condence intervals were generated across all years using nite population correction
and post stratication, based on categories of population size served. This handles non-response adjustment by
population size and accounts for the fact that population size by category is known and limited in size.
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
17

Subgroup Analysis
Throughout this report, data are analyzed by various LHD jurisdiction characteristics, namely size of population served,
type of governance, United States census regions, and degree of urbanization.
Size of population served
Statistics are compared across LHDs serving jurisdictions of dierent population sizes. LHDs are classied as small if
they serve fewer than 50,000 people, medium if they serve between 50,000 and 500,000 people, and large if they serve
500,000 or more people. For certain statistics that are highly dependent on size of population served (e.g., nance and
workforce statistics), a larger number of population subgroups are used.
Type of governance
Statistics are compared across LHDs’ relationship to their state health department. Some LHDs are agencies of local
government (referred to as locally governed). Others are local or regional units of the state health department (referred
to as state-governed). Some are governed by both state and local authorities (called shared governance). Refer to
Chapter 2 (Jurisdiction and Governance) for more details.
United States census region
Statistics are also compared across United States census regions. All LHDs in each state are classied as being in the
North, South, Midwest, or West, per the U.S. Census Bureau (http://www.census.gov/econ/census/help/geography/
regions_and_divisions.html).
Degree of urbanization
Statistics are compared across LHD jurisdiction degree of urbanization. Each LHD in the Prole study population was
classied as serving either an urban or rural jurisdiction. This classication system used the National Center for Health
Statistics (NCHS) Urban-Rural Classication Scheme denitions (https://www.cdc.gov/nchs/data_access/urban_rural.
htm) and the Economic Research Service (ERS) Frontier and Remote Area Codes (https://www.ers.usda.gov/data-
products/frontier-and-remote-area-codes/). Each LHD was coded as urban or rural based on whether the majority of
people it served were from urban or rural settings (calculated for each census tract the LHD serves). This classication
system is new to the 2019 Prole. The estimates associated with some statistics may dier from items published in
previous years due to this change.
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
18
Study Limitations
The Prole study is a unique and comprehensive source of information on LHD nances, infrastructure, workforce,
activities, and other important characteristics. However, several limitations should be considered when using the results
of this study. Given the large scope of this study, the level of detail available does not provide extensive information
on all dimensions of the topics addressed. For example, the Prole provides information about whether or not an LHD
provides a specic program or service but does not provide any information about the scope or scale of that program or
service. All data are self-reported by LHD sta and are not independently veried. LHDs may have provided incomplete,
imperfect, or inconsistent information for various reasons.
While the Prole questionnaire includes denitions for many items, not every item or term is dened. For example, the
questionnaire does not include denitions for each of the 67 programs and services included in the Prole questionnaire.
Consequently, respondents may have interpreted questions and items dierently.
Responding to the Prole questionnaire is time-intensive; consequently, respondents may have skipped some questions
because of time restrictions. In addition, responses to some questions may have been based on estimation to reduce
burden. In particular, questions on nance were dicult for LHDs to answer and yielded large amounts of missing data.
Refer to Chapter 6 (Finance) for more details.
Comparisons with data from prior Prole studies are provided for some statistics, but these comparisons should be
viewed with caution because both the study population and the respondents are dierent for each Prole study. In
addition, comparisons are not tested for statistical signicance.
Introduction
CHAPTER
1
NACCHO | 2019 National Prole of Local Health Departments
19

This chapter includes the following:
Population sizes served by local health
departments (LHDs).
Geographic jurisdictions served by LHDs.
Governance of LHDs.
Combined Health and Human
ServicesAgencies.
Local boards of health.
Jurisdiction and Governance
CHAPTER 2

Figure 2.1 | Size of population served by LHDs in the study population
There are approximately 2,800 LHDs in
the United States, but not every unit
is included in the Prole study. LHDs
operating under a centralized government
structure may include multiple levels (e.g.,
county units and multi-county regions or
districts). The state health agency selects
one level for inclusion in the Prole.
2,459 LHDs were included in the 2019
Prole study population.
LHDs serve dierent sized jurisdictions
across the U.S. Of the 2,459 LHDs included
in the 2019 Prole study population, 61%
serve fewer than 50,000people.
Size of population served N Percent
<10,000 404 16%
10,000–24,999 575 23%
25,000–49,999 510 21%
50,000–74,999 248 10%
75,000–99,999 136 6%
100,000–199,999 238 10%
200,000–499,999 198 8%
500,000–999,999 100 4%
1,000,000+ 50 2%
Total 2,459
NACCHO | 2019 National Prole of Local Health Departments
21
CHAPTER
2 Jurisdiction and Governance

Technical note
The total population served by all LHDs included in the
study represents 98% of the total U.S. population.
61%
9%
Small (<50,000)
33%
37%
Medium (50,000–499,999)
6%
52%
Large (500,000+)
Percent of all LHDs Percent of population served by LHDs
N=2,459
Figure 2.2 | Percent of United States population served by LHDs
Throughout this report, small LHDs are
classied as those that serve populations
of fewer than 50,000 people; medium
LHDs serve populations of between 50,000
and 500,000 people; and large LHDs serve
populations of 500,000 or more people.
Although only 6% of all LHDs are classied
as large, they serve about half of the U.S.
population.
The majority of LHDs are small, but
together, they serve less than 10% of the
U.S. population.
NACCHO | 2019 National Prole of Local Health Departments
22
CHAPTER
2 Jurisdiction and Governance

*County includes city-counties
**Other includes LHDs serving multiple cities or towns
N=2,459
70%
71%
67%
70%
19%
24%
11%
6%
8%
3%
14%
23%
3%
2%
7%
1%
All LHDs
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
County*
City or town
Multi-
county Other**
Percent of LHDs
Size of population served
Figure 2.3 | Geographic jurisdictions served by LHDs, by size of population served
Approximately two-thirds of LHDs are
county-based, and an additional 8% serve
multiple counties. One-fth of LHDs serve
cities or towns.
Large LHDs are less likely to serve cities or
towns but are more likely to serve multiple
counties than small LHDs.
NACCHO | 2019 National Prole of Local Health Departments
23
CHAPTER
2 Jurisdiction and Governance

RI was excluded from the study
N=2,459
LA
ID
AZ
UT
MT
WY
NM
CO
AL
FL
SC
TN
KY
IN
OH
NC
SD
KS
NE
MN
WI
IA
IL
MO
AR
MS
OK
ND
OR
CA
NV
WA
TX
MI
GA
AK
HI
PA
ME
VA
NY
CT
WV
VT
NH
MA
DE
DC
RI
MD
NJ
Figure 2.4 | Type of LHD governance, by state
Of the 2,459 LHDs included in the 2019
Prole study population, 1,886 are locally
governed, 405 are units of the state health
agency, and 168 have shared governance.
In 30 states, all LHDs are locally
governed. These states are referred
toasdecentralized.
All LHDs in Florida, Georgia, and Kentucky
have shared governance.
All LHDs in Arkansas, Delaware, Hawaii,
Mississippi, New Mexico, and South
Carolina are units of the state health
agency. These states are referred to
ascentralized.
n Local (all LHDs in state are units of local government)
n State (all LHDs in state are units of state government)
n Shared (all LHDs in state governed by both state and local authorities)
n Mixed (LHDs in state have more than one governance type)
NACCHO | 2019 National Prole of Local Health Departments
24
CHAPTER
2 Jurisdiction and Governance

RI was excluded from the study
n=1,479
LA
ID
AZ
UT
MT
WY
NM
CO
AL
FL
SC
TN
KY
IN
OH
NC
SD
KS
NE
MN
WI
IA
IL
MO
AR
MS
OK
ND
OR
CA
NV
WA
TX
MI
GA
AK
HI
PA
ME
VA
NY
CT
WV
VT
NH
DE
DC
RI
MD
MA
NJ
MD
MA
Figure 2.5 | LHDs as a part of a combined Health and Human Services Agency (HHSA), by state
One in ve LHDs are currently part of a
combined Health and Human Services
Agency (HHSA).
More than half of LHDs in six states are
part of a combined HHSA; at least one-
third of LHDs in eight states are a part of a
combined HHSA; and fewer than one-third
of LHDs in the remaining states are a part
of a combined HHSA.
Combined Health and Human Services
Agency(HHSA)
A combined health and human services agency can be
dened as an agency that administers all programs dealing
with health and welfare. A combined health and human
services agency provides a broad range of health and social
services to promote wellness, self-suciency, and a better
quality of life by integrating health and social services
through a unied service-delivery system.
n More than 50% of LHDs
n 33%–50% of LHDs
n Less than 33% of LHDs
n DC, ID, MS, and UT had insucient data
NACCHO | 2019 National Prole of Local Health Departments
25
CHAPTER
2 Jurisdiction and Governance

20% 50% 30%
All LHDs
20% 51% 29%
Small (<50,000)
21% 50% 30%Medium (50,000–499,999)
19% 38% 43%
Large (500,000+)
33% 9% 58%
State
18% 63% 19%
Local
11% 41% 48%
Shared
Advisory
Governing No LBOH
Size of population served
Percent of LHDs with a local board of health
Type of governance
n=1,469
Figure 2.6 | LHDs with a local board of health (LBOH), by size of population served and type of governance
Seventy percent of LHDs have a local
board of health (LBOH).
A larger proportion of small LHDs have
LBOHs compared to large LHDs.
Locally governed LHDs are more likely
to have a LBOH compared to LHDs
that are state-governed or with shared
governance.
A higher proportion of LHDs have LBOHs
with a governing role compared to an
advisory role. However, state-governed
LHDs are more likely to have an advisory
LBOH than a governing body.
NACCHO | 2019 National Prole of Local Health Departments
26
CHAPTER
2 Jurisdiction and Governance

*Among LHDs with a LBOH
n=1,016
75%
Oversight
66% Policy development
61% Legal authority
49% Continuous improvement
47% Resource stewardship
47% Partner engagement
8% None of the above
Percent of LHDs* with LBOH utilizing function
Figure 2.7 | Functions that local boards of health (LBOHs) utilize on a continuous basis
The National Association for Local Boards
of Health (NALBOH) identies six functions
of public health governance.
Most LHDs have LBOHs that provide
oversight, while fewer have LBOHs that
provide resource stewardship and partner
engagementfunctions.
Local board of health functions
Oversight is to assume ultimate responsibility for public health performance
in the community by providing necessary leadership and guidance in order
to support the public health agency in achieving measurable outcomes,
such as by hiring or ring the agency head.
Policy development is to lead and contribute to the development of policies
that protect, promote, and improve public health while ensuring that the
agency and its components remain consistent with the laws and rules to
which it issubject.
Legal authority is to exercise legal authority as applicable by law and
understand the roles, responsibilities, obligations, and functions of the
governing body, health ocer, and agency sta, such as by adopting public
health regulations and imposing or enforcing quarantine or isolation orders.
Continuous improvement is to routinely evaluate, monitor, and set
measurable outcomes for improving community health status and the public
health agency’s/governing body’s own ability to meet itsresponsibilities.
Resource stewardship is to assure the availability of adequate resources to
perform essential public health services, such as by approving the LHD budget,
setting and imposing fees, imposing taxes for public health, or requesting a
public health levy.
Partner engagement is to build and strengthen community partnerships
through education and engagement to ensure the collaboration of all
relevant stakeholders in promoting and protecting the community’s health.
Refer to the 2015 Local Board of Health Prole for additional data on
these functions (available at www.naccho.org/resources/lhd-research/
national-prole-of-local-boards-of-health).
NACCHO | 2019 National Prole of Local Health Departments
27
CHAPTER
2 Jurisdiction and Governance

This chapter includes the following:
Cross-jurisdictional sharing of services.
Local health department (LHD) partnerships
and collaborations.
LHD engagement with academic institutions.
Partnerships
CHAPTER 3

More than half of LHDs share resources
(such as funding, sta, or equipment) with
other LHDs on a continuous, recurring,
non-emergency basis, regardless of size.
A larger proportion of LHDs with shared
governance share resources than locally
governed LHDs.
n=369
Size of population served
Type of governance
All LHDs
55%
Small (<50,000)
56%
Medium (50,000–499,999)
54%
Large (500,000+)
54%
State
59%
Local
52%
Shared
69%
Percent of LHDs sharing services or resources with other LHD(s)
Figure 3.1 | Cross-jurisdictional sharing of services, by size of population served and type of governance
Cross-jurisdictional sharing ofservices
Cross-jurisdictional sharing of services is a phrase used
to refer to the various means by which jurisdictions work
together to provide public health services. LHDs across the
country are looking to cross-jurisdictional sharing as a way
to help them more eciently and eectively deliver public
health services. The information provided in this section
reects sharing resources on a continuous, recurring, non-
emergency basis.
NACCHO | 2019 National Prole of Local Health Departments
29
CHAPTER
3 Partnerships

n=359–363
38% LHD provides functions/services for another LHD
35% LHD receives functions/services from another LHD
33% LHD shares a sta member with another LHD
29% Another LHD shares a sta member with LHD
24% LHD shares equipment with another LHD
21% Another LHD shares equipment with LHD
Percent of LHDs sharing resource/service with other LHD(s)
Figure 3.2 | Type of cross-jurisdictional sharing of services
More than one-third of LHDs receive
functions or services from another LHD
or provide functions or services for
anotherLHD.
LHDs are more likely to share resources
with another LHD than they are to receive
them. For example, one-third of LHDs
share sta members with another LHD,
while 29% have another LHD share a sta
member with them.
Cross-jurisdictional sharing ofservices
Cross-jurisdictional sharing of services is a term used to
refer to the various means by which jurisdictions work
together to provide public health services. LHDs across the
country are looking to cross-jurisdictional sharing as a way
to help them more eciently and eectively deliver public
health services. The information provided in this section
reects sharing resources on a continuous, recurring, non-
emergency basis.
NACCHO | 2019 National Prole of Local Health Departments
30
CHAPTER
3 Partnerships

n=183–366
Percent of LHDs working with organization in any way
Percent of LHDs regularly scheduling meetings, have written agreements, or share personnel/resources with organization
84% 47%
84% 41%
78%
78%
39%
35%
77% 31%
71% 29%
35% 18%
Government partners
Criminal justice system
Local planning
Parks and recreation
Economic and community development
Housing
Transportation
Tribal government
97% 77%
94% 74%
93% 46%
92% 62%
57% 89%
74% 22%
72% 39%
Healthcare partners
Emergency responders
Hospitals
Physician practices/medical groups
Community health centers
Mental health/substance abuse providers
Veterinarians
Health insurers
25%
98%
71%
96% 21%
92% 72%
88% 62%
87% 44%
87% 48%
82% 45%
74%
Community-based partners (e.g., education, non-government)
K–12 schools
Media
Community-based non-prots
Faith communities
Colleges or universities
Businesses
Cooperative extensions
Libraries
Figure 3.3 | LHD partnerships and collaborations in the past year
LHDs work with a variety of partners in
their communities in a variety of ways,
such as sharing information, regularly
scheduling meetings, establishing
written agreements, and sharing
personnel/resources.
More than 95% of LHDs work with
some partners, including emergency
responders, K-12 schools, and the media.
Collaborations with other partners
are less universal, including tribal
governments, transportation agencies,
andhealthinsurers.
Overall, LHDs are less likely to collaborate
in ways beyond exchanging information
(i.e., regularly scheduling meetings,
establishing written agreements,
or sharing personnel/resources).
This dierence is particularly large
for the media (only 21% collaborate
beyond information exchange while
96% exchange information) and
veterinarians (only 26% collaborate
beyond information exchange while
74%exchangeinformation).
NACCHO | 2019 National Prole of Local Health Departments
31
CHAPTER
3 Partnerships

Figure 3.4 | Formal* LHD partnerships and collaborations, over time Percent of LHDs that *share personnel/resources and/or have written agreements
Healthcare partners Government partners
K–12 schools
Colleges or
universities
Community-based
non-prots
Cooperative
extensions
Faith communities
Businesses
Media
Libraries
59%
38%
49%
45%
30%
53%
34%
18%
39%
28%
10%
23%
19%
8%
19%
18%
7%
26%
13%
12%
11%
5%
16%
Community-based partners
2016 20192008
Local planning
Criminal
justice system
Parks and
recreation
Economic and
community
development
Transportation
Housing
Tribal
government
26%
10%
18%
19%
14%
25%
11%
7%
15%
9%
12%
17% 17%
2016 20192008
Emergency
responders
Hospitals
Physician
practices/
medical groups
Community
health centers
Health insurers
Mental health/
substance abuse
providers
Veterinarians
61%
39%
44%
57%
35%
2016 20192008
47%
38%
30%
26%
42%
24%
23%
32%
19%
14%
19%
34%
21%
n=414–447 n=218–483 n=183–366
Although the proportion of LHDs reporting formal
collaborations with many organization types decreased
between 2013 and 2016, it increased between 2016
and2019.
Despite these increases, the proportion of LHDs reporting
formal collaborations with many organization types
has not recovered to 2013 results. In particular, formal
partnerships with emergency responders, hospitals,
andK-12 schools saw the greatest overall declines.
Conversely, LHDs were more likely to report formal
partnerships with health insurers, colleges or universities,
and businesses in 2019, compared to 2013.
LHDs are generally less likely to have formal partnerships
with government partners than with either healthcare or
other community-based partners.
NACCHO | 2019 National Prole of Local Health Departments
32
CHAPTER
3 Partnerships

n=183–365
44%
39%
38%
36%
36%
27%
21%
36%
42%
25%
39%
33%
24%
12%
Government partners
Local planning
Criminal justice system
Parks and recreation
Economic and community development
Housing
Transportation
Tribal government
79%
58%
51%
45%
43%
37%
35%
34%
26%
57%
43%
31%
23%
35%
19%
37%
Community-based partners
Media
K–12 schools
Community-based non-prots
Businesses
Faith communities
Colleges or universities
Libraries
Cooperative extensions
Percent of LHDs sending data Percent of LHDs receiving data
63%
57%
50%
48%
46%
39%
35%
48%
49%
44%
44%
34%
34%
Healthcare partners
Physician practices/medical groups
Hospitals
Mental health/substance abuse providers
Emergency responders
Community health centers
Veterinarians
Health insurers
60%
Figure 3.5 | Direction of information exchange between LHDs and partner organizations in the past year
With most partners, a greater proportion
of LHDs sent data than received data when
sharing information in the past year. In
particular, LHDs were three times as likely
to send data to media partners than to
receive data.
In the past year, more than half of LHDs
shared data (sent and received) with
hospitals and K-12 schools.
Few LHDs shared data (sent or received)
with transportation agencies and
tribalgovernments.
NACCHO | 2019 National Prole of Local Health Departments
33
CHAPTER
3 Partnerships

Figure 3.6 | Engagement with academic institutions in the past year, by size of population served
All LHDs
Size of population served
Small
(<50,000)
Medium
(50,000–
499,999)
Large
(500,000+)
LHD accepts students from academic institutions as trainees, interns, or volunteers 76% 66% 91% 93%
LHD actively recruits graduates from academic institutions 31% 17% 50% 67%
LHD sta serve on an academic institution advisory group 28% 16% 42% 67%
LHD sta serve as faculty in academic institutions 23% 8% 40% 76%
Faculty/sta from academic institutions have served in a consulting role for LHD 23% 10% 39% 58%
Academic instruction collaborates with LHDs on research studies 22% 11% 33% 67%
LHD contracts with academic institution to provide public healthservices 11% 8% 14% 22%
LHD has formal relationship with academic institutions to provide training or
professional development for LHD sta
11% 5% 16% 35%
Academic institutions have agreements or policies on providing LHD with access
toscientic and professional journals
8% 3% 15% 25%
None of the above 21% 30% 6% 4%
Some LHDs engage and partner with
academic institutions. Three-quarters
accept students from academic
institutions (as trainees, interns, or
volunteers) but fewer actively recruit
graduates frominstitutions.
Fewer than one-third of LHDs have sta
that serve on an academic institution
advisory group or as faculty.
Medium and large LHDs are more likely
to engage in partnership activities with
academic institutions than small LHDs.
Notably, almost all larger LHDs accept
students from academic intuitions.
In 2019, LHDs were less likely to have
a formal relationship with academic
institutions to provide training or
professional development for LHD sta
than in 2016 (25%, not shown).
n=373
NACCHO | 2019 National Prole of Local Health Departments
34
CHAPTER
3 Partnerships

Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 3.7 | Engagement with academic institutions in the past year, by degree of urbanization
LHDs in urban areas are more likely to
engage with academic institutions. For
example, 41% actively recruit graduates
from academic institutions, compared to
only 20% of LHDs in rural areas. Similarly,
35% of urban LHD sta serve on faculty in
academic institutions, compared to only
11% of rural LHD sta.
All LHDs
Degree of urbanization
Urban Rural
LHD accepts students from academic institutions as trainees, interns, or volunteers 76% 80% 72%
LHD actively recruits graduates from academic institutions 31% 41% 20%
LHD sta serve on an academic institution advisory group 28% 37% 18%
LHD sta serve as faculty in academic institutions 23% 35% 11%
Faculty/sta from academic institutions have served in a consulting role for LHD 23% 33% 12%
Academic instruction collaborates with LHDs on research studies 22% 29% 14%
LHD contracts with academic institution to provide public health services 11% 14% 8%
LHD has formal relationship with academic institutions to provide training or professional development
forLHD sta
11% 14% 7%
Academic institutions have agreements or policies on providing LHD with access to scientic and
professional journals
8% 12% 4%
None of the above 21% 15% 26%
n=373
NACCHO | 2019 National Prole of Local Health Departments
35
CHAPTER
3 Partnerships

*In schools or programs other than nursing or public health
n=311
83% Schools of nursing
74%
Four-year colleges
or universities*
67%
Accredited schools or
programs of public health
45% Community colleges (two-year)*
Figure 3.8 | Engagement with specic academic institutions in the past year
LHDs are more likely to be engaged with
Schools of Nursing than other kinds of
academic institutions.
Two-thirds of LHDs partner or interact
with accredited schools or programs of
publichealth.
Less than half of LHDs engaged with two-
year community colleges in the past year.
Percent of LHDs engaging with academic institution
NACCHO | 2019 National Prole of Local Health Departments
36
CHAPTER
3 Partnerships

1%
Size of population served
24% 75%Small (<50,000)
44% 6% 50%Medium (50,000–499,999)
51% 32% 17%Large (500,000+)
Degree of urbanization
38% 6% 56%Urban
26% 3% 71%Rural
Percent of LHDs participating in research studies
32% 5% 63%All LHDs
4 or more
studies1 to 3 studies No studies
n=303
Figure 3.9 | Number of research studies in which LHDs participated during the past year, by size of population served
and degree of urbanization
One in three LHDs reported participating
in at least one research study during the
past year.
Large LHDs were more likely to participate
in research studies than small and medium
LHDs. In particular, one-third of large LHDs
participated in more than three studies
during the pastyear.
LHDs in urban areas participate in a greater
number of research studies than those in
rural areas.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
NACCHO | 2019 National Prole of Local Health Departments
37
CHAPTER
3 Partnerships

n=324
Figure 3.10 | Participation in research activities during the past year, by size of population served
More than half of LHDs did not participate
in research activities during the past
year. The most common research activity
LHDs did participate in was collecting,
exchanging, or reporting data for a study.
Large LHDs were more likely to report
participating in research activities than
small LHDs. For example, 56% of large
LHDs applied research ndings to
practices within their own organization,
compared to only 7% of small LHDs.
All LHDs
Size of population served
Small
(<50,000)
Medium
(50,000–
499,999)
Large
(500,000+)
Collecting, exchanging, or reporting data for a study 29% 19% 39% 64%
Disseminating research ndings to key stakeholders 18% 9% 30% 50%
Applying research ndings to practices within own organization 17% 7% 29% 56%
Analyzing and interpreting study data and ndings 17% 10% 24% 58%
Identifying research topics and questions that are relevant to public health practice 15% 8% 21% 50%
Recruiting study sites and/or study participants 11% 6% 13% 52%
Helping other organizations apply research ndings to practice 11% 6% 14% 39%
Developing or rening research plans and/or protocols for public health studies 9% 3% 13% 35%
None of the above 62% 74% 47% 16%
NACCHO | 2019 National Prole of Local Health Departments
38
CHAPTER
3 Partnerships

This chapter includes the following:
Characteristics of local health department
(LHD) top executives, including age, tenure,
and degrees held.
Characteristics of new versus experienced
LHDtop executives.
Leadership
CHAPTER 4
14%
9%
10%
7%
6%
2% 2% 2% 2% 2%
7%
6%
7%
8%
8%
56%
58%
60%
62%
66%
2008
n=2,229–2,298
2010
n=2,036–2,087
2013
n=1,946–1,966
2016
n=1,843–1,868
2019
n=1,463–1,465
Female
Percent of LHD top executives
Race other
than white
Part-time position
Hispanic/Latino
Figure 4.1 | Characteristics of LHD top executives
Two-thirds of top executives identify
as female; since 2008, the percentage
of female top executives has increased
steadily, from 56% in 2008 to 66% in 2019.
Fewer than 10% of top executives are
Hispanic/Latino or a race other than white,
and this percentage has remained low
since 2008.
The percentage of top executives that
are part-time positions has decreased by
more than half since 2008, from 14% to 6%
in2019.
NACCHO | 2019 National Prole of Local Health Departments
40
Leadership
CHAPTER
4

9% 9% 9%
12%
11%
25%
23%
23%
24%
27%
46%
45%
42%
39%
36%
17%
21%
23%
24%
23%
3%
2% 2% 2%
3%
2008
n=2,188
2010
n=2,005
2013
n=1,877
2016
n=1,757
2019
n=1,409
Younger than 40
40–49
50–59
60–69
Percent of LHD top executives
70 or older
Figure 4.2 | Age of LHD top executives, over time
Almost two-thirds of top executives are 50
or older, and one-quarter are 60 or older.
Eleven percent are younger than 40.
Since 2008, the proportion of top
executives in their fties has declined.
Meanwhile, the proportions of both older
(60+) and younger (less than 50) top
executives have grown.
NACCHO | 2019 National Prole of Local Health Departments
41
Leadership
CHAPTER
4

Compared to 2010 and 2013, top
executives have been in their positions for
fewer years. Since 2013, the percentage
of top executives who have been in their
positions less than ve years has increased,
while the percentage of top executives
who have been in their positions for six or
more years has decreased.
20%
20%
28%
21%
28%
27%
29%
36%
21%
23%
18%
19%
31%
30%
24%
24%
2010
n=2,033 n=1,930 n=1,759 n=1,359
2013 2016 2019
Less than 2 years
2–5 years
6–10 years
11 or more years
Percent of LHD top executives
Figure 4.3 | Tenure of LHD top executives, over time
NACCHO | 2019 National Prole of Local Health Departments
42
Leadership
CHAPTER
4

Since 2008, the average tenure for top
executives decreased from 8.7 years to 7.6
years. However, the average tenure has
remained steady over the past three years.
Although average tenure has decreased
overall since 2008 among LHDs serving
dierent population sizes, it has increased
slightly for medium and large LHDs over
the past three years.
Top executives at large LHDs remain in
their positions for fewer years on average
than top executives at medium or
smallLHDs.
2008 2010 2013 2016 2019
8.9
9.3
9.2
8.0
7.9
6.3
8.4
6.9
8.1
6.4
6.9
4.9
7.4
5.2
8.7
8.8
8.7
7.5
7.6
Medium
(50,000–499,999)
Small (<50,000)
Large (500,000+)
Mean number of years
All LHDs
n=2,207 n=2,033 n=1,930 n=1,759 n=1,359
Figure 4.4 | Average tenure (in years) of LHD top executives, over time and by size of population served
NACCHO | 2019 National Prole of Local Health Departments
43
Leadership
CHAPTER
4

8% 29% 49% 14%All LHDs
12% 39% 42% 7%Small (<50,000)
2%
17% 64% 18%Medium (50,000–499,999)
4% 40% 56%Large (500,000+)
14% 37% 42% 8%Rural
3% 22% 56% 20%Urban
Associate’s Bachelor’s Master’s Doctoral
Percent of LHD top executives
Size of population served
Degree of urbanization
n=1,422
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 4.5 | Highest degree obtained by LHD top executive, by size of population served and degree of urbanization
The highest degree held by top
executives is most often a Master’s
degree, followed by a Bachelor’s degree.
Fewer top executives hold Associate’s or
Doctoraldegrees.
Top executives at large LHDs are much
more likely to have graduate degrees
(96%) than top executives at small
LHDs(49%).
Similarly, top executives at LHDs serving
urban areas are much more likely to
have graduate degrees (76%) than
top executives at LHDs serving rural
areas(50%).
NACCHO | 2019 National Prole of Local Health Departments
44
Leadership
CHAPTER
4

30% 24% 9%All LHDs
23% 30% 5%Small (<50,000)
39% 17% 12%Medium (50,000–499,999)
40% 5% 40%Large (500,000+)
21% 33% 5%Rural
38% 16% 14%Urban
NursingPublic health Medical
Percent of LHD top executives
Size of population served
Degree of urbanization
n=1,447
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 4.6 | Specialized degrees obtained by LHD top executive, by size of population served
and degree of urbanization
Slightly less than one-third of top
executives hold a public health degree,
nearly one-quarter hold nursing degrees,
and 9% hold medical degrees.
Top executives at large LHDs are more
likely to have public health or medical
degrees than nursing degrees. On the
other hand, top executives at small LHDs
are more likely to have nursing degrees
than public health or medical degrees.
Top executives at LHDs serving rural areas
are more likely to have nursing degrees
than top executives at LHDs serving
urbanareas.
NACCHO | 2019 National Prole of Local Health Departments
45
Leadership
CHAPTER
4

n=1,300–1,337
26%
7%
Younger than 40 years old
33%
33%
9%
8%
Gender and race identity
Race other than white
Male
61%
63%
Have a graduate degree
26%
31%
6%
9%
Have a specialized degree in public health or medicine
Public health
Medical
New: Top executive for less than three years
Experienced: Top executive for three or more years
Percent of LHD top executives
Figure 4.7 | Characteristics of new versus experienced LHD top executives
In some ways, new top executives (i.e.,
top executives who have been in their
positions for less than three years) are
dierent than experienced top executives.
For example, new top executives are
more likely to be younger than 40 than
experienced top executives.
On the other hand, new top executives are
typically of similar gender identity and race
as experienced top executives, i.e., mostly
white females.
New top executives are also slightly less
likely to have a graduate degree or a
specialized degree in public health or
medicine than their more experienced
counterparts.
NACCHO | 2019 National Prole of Local Health Departments
46
Leadership
CHAPTER
4

This chapter includes the following:
Current numbers of local health department
(LHD) sta (employees and Full-Time
Equivalents (FTEs)).
Changes in numbers of LHD sta
(2008to2009).
Annual LHD job losses and gains.
Employees retiring from LHD workforce.
Occupations employed by LHDs.
Technical note
Statistics were calculated using all valid data available, regardless of missing information
inother occupations, total employees, and total FTEs.
Workforce
CHAPTER 5

17%
Fewer than 5
19%
5–9.9
26%
10–24.9
15%
25–49.9
11%
50–99.9
6%
100–199.9
6%
200 or more
Percent of LHDs
n=1,468
Figure 5.1 | Number of Full-Time Equivalents (FTEs)
Almost all LHDs employ less than 50 FTEs,
with 35% employing less than 10 FTEs and
41% employing between 10 and 50 FTEs.
Only 10% of LHDs employ between 50
and 100 FTEs, and 12% employ 100 or
moreFTEs.
NACCHO | 2019 National Prole of Local Health Departments
48
CHAPTER
5 Workforce

Figure 5.2 | Mean and median number of employees and Full-Time Equivalents (FTEs), by size of population served
On average, LHDs employ 62 employees
or 56 FTEs.
However, these numbers vary greatly by
the size of population served by the LHD.
While LHDs that serve less than 25,000
people employ 12 employees or 10 FTEs
on average, LHDs that serve over one
million people employ 846 employees or
769 FTEs on average.
Size of population served
Number of employees Number of FTEs
Mean Median Mean Median
All LHDs 62 20 56 17
<25,000 12 8 10 6
25,000–49,999 23 15 20 13
50,000–99,999 38 30 34 26
100,000–249,999 70 60 64 54
250,000–499,999 155 114 143 104
500,000–999,999 304 255 269 218
1,000,000+ 846 489 769 456
n(employees)=1,467
n(FTEs)=1,468
NACCHO | 2019 National Prole of Local Health Departments
49
CHAPTER
5 Workforce

4.1
All LHDs
Size of population served
7.7
<10,000
7.0
10,000–24,999
5.4
25,000–49,999
4.8
50,000–999,999
4.1
100,000–199,999
4.2
200,000–499,999
3.9
500,000–999,999
3.5
100,000,000+
Number of FTEs
Technical note
The number of LHD FTEs per 10,000 people served by the
LHD is a useful way to measure overall workforce capacity
and facilitates comparisons across LHDs serving dierent
jurisdiction sizes. These statistics are computed by summing
the FTE sta (for all LHDs or for LHDs in specic jurisdiction
size categories), dividing by the total population of those
jurisdictions, and multiplying by 10,000.
n=1,468
Figure 5.3 | Full-Time Equivalents (FTEs) per 10,000 people, by size of population served
Among all LHDs, the overall workforce
capacity is 4.1 FTEs per 10,000 people.
LHDs that serve smaller populations
employ a greater number of FTEs per
10,000 people than LHDs that serve
largerpopulations.
NACCHO | 2019 National Prole of Local Health Departments
50
CHAPTER
5 Workforce

Technical note
The condence intervals reect the uncertainty
oftheseestimates.
153,000
136,000
Total employees
n=1,467
Total Full-Time
Equivalents (FTEs)
n=1,468
140,000 166,000
125,000 147,000
Estimated size 95% Condence intervals
Figure 5.4 | Estimated size of the LHD workforce
Approximately 153,000 employees or
136,000 FTEs are employed by LHDs.
NACCHO | 2019 National Prole of Local Health Departments
51
CHAPTER
5 Workforce

n=1,468
Urban
82%
Rural
18%
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 5.5 | Distribution of Full-Time Equivalents (FTEs), by degree of urbanization
More than three-quarters of LHD FTEs
(82%, or 112,000 FTEs) are employed by
LHDs that serve urban areas. Only 18% of
LHD FTEs (24,000 FTEs) are employed by
LHDs that serve rural populations.
Percent of LHD FTEs
NACCHO | 2019 National Prole of Local Health Departments
52
CHAPTER
5 Workforce
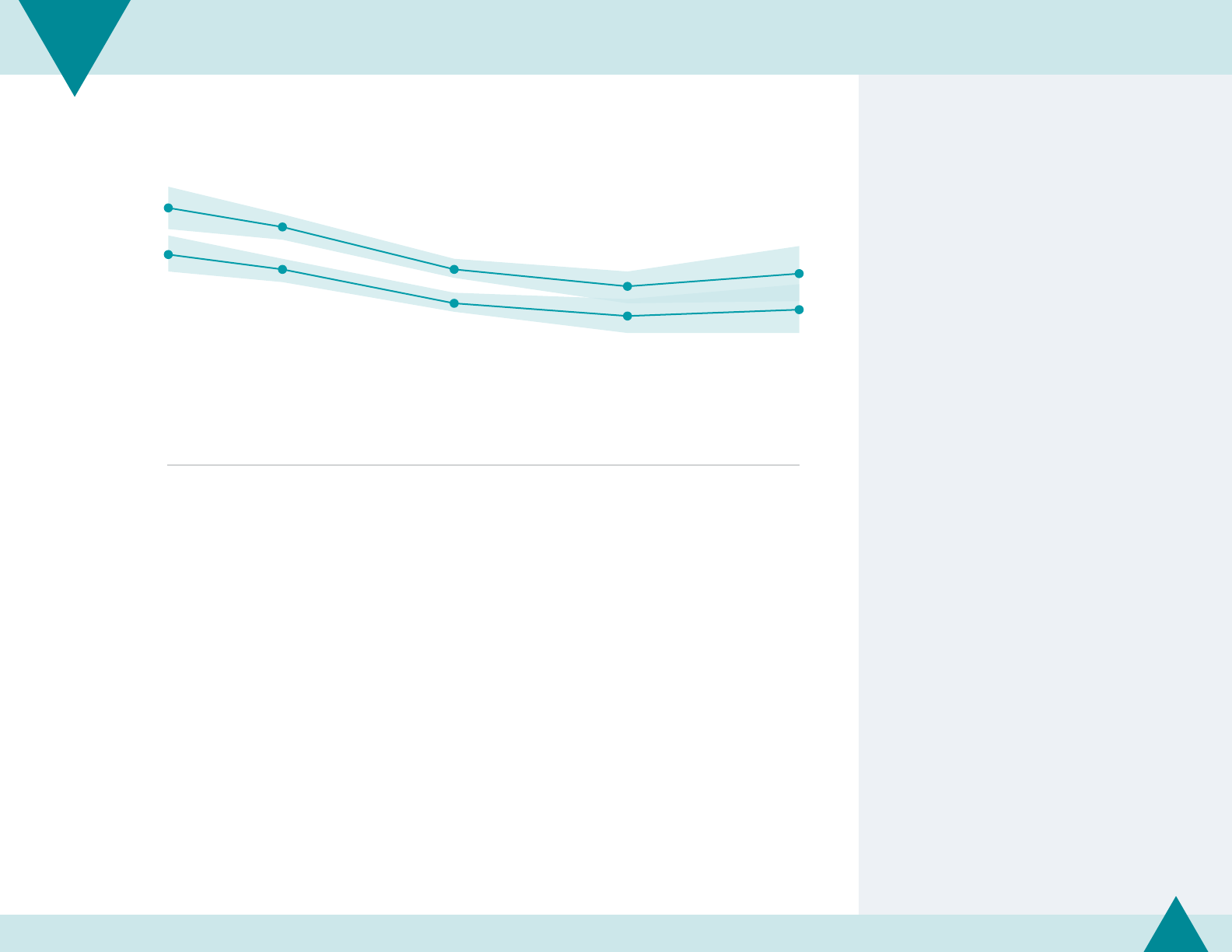
Technical note
Estimates for 2008–2013 workforce are dierent from
previous reports due to new weighing and cleaning
methodologies. Refer to page 17 for more information on
the methodology.
The condence intervals reect the uncertainty of these
estimates (because of incomplete data and great variability
in numbers of LHD sta ).
Light teal shading depicts 95% Condence Interval.
184,000
175,000
155,000
147,000
153,000
162,000
155,000
139,000
133,000
136,000
Total employees
Total Full-Time
Equivalents (FTEs)
2008 2010 2013 2016 2019
n=2,203–2,232 n=1,969–2,031 n=1,920–1,940 n=1,743–1,827 n=1,467–1,468
Figure 5.6 | Estimated size of LHD workforce, over time
Since 2008, the estimated number of LHD
employees has decreased from 184,000
in 2008 to 153,000 in 2019—a decrease
of17%.
Similarly, the estimated number of FTEs
employed by LHDs has decreased from
162,000 in 2008 to 136,000 in 2019—a
decrease of 16%.
NACCHO | 2019 National Prole of Local Health Departments
53
CHAPTER
5 Workforce

2008 2010 2013 2016 2019
n=2,203 n=1,969 n=1,920 n=1,743 n=1,468
6.8
7.4
5.0
6.1
4.5
4.1
3.6
4.5
3.8
4.5
6.8
4.7
6.2
4.3
4.9
3.6
5.2
4.1
Medium
(50,000–499,999)
Small (<50,000)
Large (500,000+)
All LHDs
Number of FTEs per 10,000 people
Figure 5.7 | Full-Time Equivalents (FTEs) per 10,000 people, over time and by size of population served
Overall, LHDs lost 21% of their workforce
capacity since 2008. While 5.2 FTEs per
10,000 people were employed at LHDs in
2008, only 4.1 FTEs per 10,000 people were
employed in 2019.
Large LHDs have experienced a
greater loss in workforce capacity
thansmallerLHDs.
Technical notes
This gure shows changes in overall LHD workforce capacity
(measured in FTEs per 10,000 people) between 2008 and
2019. See notes on Figure 5.3 for more information on how
these statistics are computed.
Estimates for 2008–2013 workforce are dierent from
previous reports due to new weighing and cleaning
methodologies. Refer to page 17 for more information on
the methodology.
NACCHO | 2019 National Prole of Local Health Departments
54
CHAPTER
5 Workforce

2008 2010 2013 2016 2019
n=421 n=385 n=456 n=394 n=385
2.5%
2.6%
2.9%
2.7%
2.5%
Percent of LHD workforce
Figure 5.8 | LHD workforce that retired, over time
Less than 3% of the total LHD workforce
retired in 2019.
Overall, the percentage of the LHD
workforce that is retiring has not changed
since 2008. However, it did peak in
2013 and has been decreasing steadily
sincethen.
NACCHO | 2019 National Prole of Local Health Departments
55
CHAPTER
5 Workforce

Figure 5.9 | Occupations employed at LHDs, by size of population served
Almost all LHDs employ registered nurses
and oce and administrative support
sta. Fewer LHDs employ animal control
workers, behavioral health sta, or
laboratoryworkers.
Large LHDs are much more likely than
small LHDs to employ epidemiologist/
statisticians, information systems
specialists, public information
professionals, and public health
physicians. The proportion of LHDs
employing oce and administrative
support sta and nursing or home health
aides is approximately the same across
jurisditction sizes.
Size of population served
All LHDs <25,000
25,000–
49,999
50,000–
99,999
100,000–
249,999
250,000–
499,999
500,000–
999,999 1,000,000+
Agency leadership 83% 73% 84% 87% 94% 97% 94% 100%
Animal control worker 9% 4% 8% 14% 10% 11% 24% 14%
Behavioral health sta 16% 8% 11% 21% 18% 33% 55% 46%
Business and nancial operations sta 53% 38% 49% 54% 72% 79% 90% 100%
Community health worker 35% 23% 28% 44% 47% 70% 73% 71%
Environmental health worker 74% 60% 77% 86% 87% 91% 90% 74%
Epidemiologist/statistician 28% 9% 14% 26% 55% 85% 94% 100%
Health educator 59% 38% 59% 68% 83% 87% 93% 91%
Information systems specialist 18% 3% 10% 14% 37% 60% 70% 74%
Laboratory worker 16% 4% 8% 17% 28% 42% 54% 89%
Licensed practical or vocational nurse 33% 24% 31% 33% 38% 50% 62% 77%
Nursing aide and home health aide 21% 20% 23% 19% 21% 20% 23% 34%
Nutritionist 49% 28% 48% 59% 71% 84% 85% 89%
Oce and administrative support sta 90% 85% 87% 96% 97% 96% 99% 100%
Oral healthcare professional 20% 10% 14% 26% 29% 35% 48% 71%
Preparedness sta 62% 45% 60% 70% 80% 94% 96% 97%
Public health physician 30% 15% 22% 34% 47% 67% 80% 94%
Public information professional 23% 9% 13% 20% 38% 67% 75% 86%
Registered nurse 94% 90% 95% 95% 98% 100% 96% 100%
n=1,473
NACCHO | 2019 National Prole of Local Health Departments
56
CHAPTER
5 Workforce

n=1,114–1,468
Figure 5.10 | Stang patterns (in median Full-Time Equivalents (FTEs)) at LHDs, by size of population served
Stang patterns of LHDs vary by the size of
population served.
LHDs serving the smallest jurisdictions typically
employ registered nurses, oce support sta, a top
executive, and environmental health workers.
LHDs serving medium-sized jurisdictions typically
also employ some additional occupations,
including health educators, preparedness sta,
nutritionists, business and nancial operations
sta, epidemiologists, public health physicians, and
community health workers.
LHDs serving jurisdictions over one million people
typically employ nearly 500 FTEs including nearly 50
registered nurses, more than 75 oce support sta,
and many employees in specialized occupations,
including information systems specialists, public
information professionals, laboratory workers, and
oral healthcaresta.
<10,000 10,000–24,999 25,000–49,999 50,000–99,999
4 Total FTEs 8 Total FTEs 14 Total FTEs 28 Total FTEs
1 Registered nurse 2 Registered nurses 3.8 Registered nurses 6 Registered nurses
1 Oce and administrative support sta 2 Oce and administrative support sta 3 Oce and administrative support sta 5 Oce and administrative support sta
0.9 Agency leadership 1 Agency leadership 1 Agency leadership 1 Agency leadership
1 Environmental health worker 1.4 Environmental health worker 3 Environmental health workers
0.6 Health educators 1 Health educator
0.5 Preparedness sta 1 Preparedness sta
0.2 Nutritionist 1 Nutritionist
1 Business and nancial operations sta
100,000–249,999 250,000–499,999 500,000–999,999 1,000,000+
60 Total FTEs 119 Total FTEs 238 Total FTEs 480 Total FTEs
10 Registered nurses 17 Registered nurses 29.5 Registered nurses 48 Registered nurses
10 Oce and administrative support sta 18.5 Oce and administrative support sta 30.8 Oce and administrative support sta 75 Oce and administrative support sta
3 Agency leadership 6 Agency leadership 7.5 Agency leadership 10 Agency leadership
7 Environmental health workers 14 Environmental health workers 25 Environmental health workers 36 Environmental health workers
2 Health educators 3 Health educators 6 Health educators 12 Health educators
1 Preparedness sta 2 Preparedness sta 3 Preparedness sta 5 Preparedness sta
2 Nutritionists 4.1 Nutritionists 8 Nutritionists 19 Nutritionists
2 Business and nancial operations sta 4 Business and nancial operations sta 8 Business and nancial operations sta 21 Business and nancial operations sta
0.5 Epidemiologist 1 Epidemiologist/statistician 3 Epidemiologist/statisticians 8 Epidemiologist/statisticians
0.1 Public health physician 1 Public health physician 1 Public health physician 3 Public health physicians
2.4 Community health worker 6.5 Community health workers 14 Community health workers
1 Information systems specialist 2 Information systems specialist 5 Information systems specialists
1 Public information professional 1 Public information professional 1 Public information professional
0.2 Licensed practical or vocational nurse 2 Licensed practical or vocational nurse 4 Licensed practical or vocational nurse
1.8 Laboratory worker 10 Laboratory worker
1 Behavioral health sta 2.7 Oral healthcare sta
NACCHO | 2019 National Prole of Local Health Departments
57
CHAPTER
5 Workforce

Technical note
Numbers do not add to totals because listed occupational
categories were not exhaustive of all LHD occupations.
n=1,110–1,129
Figure 5.11 | Estimated number of Full-Time Equivalents (FTEs) in select occupations
Approximately 23,100 FTEs are oce
andadministrative support sta and
21,200 FTEs are registered nurses.
Only 1,000 FTEs are animal control
workers and 600 FTEs are public
informationprofessionals.
Occupation Number of FTEs 95% Condence intervals
Agency leadership 5,800 5,500 6,100
Animal control worker 1,000 800 1,200
Behavioral health sta 6,700 4,500 8,900
Business and nancial operations sta 8,900 5,900 11,900
Community health worker 5,600 4,800 6,300
Environmental health worker 14,500 12,500 16,500
Epidemiologist/statistician 2,900 2,000 3,800
Health educator 7,500 5,100 9,900
Information systems specialist 2,200 1,300 3,100
Laboratory worker 2,100 1,500 2,700
Licensed practical or vocational nurse 3,600 1,900 5,400
Nursing aide and home health aide 2,200 1,800 2,600
Nutritionist 5,100 4,700 5,500
Oce and administrative support sta 23,100 20,800 25,500
Oral healthcare professional 2,200 1,900 2,500
Preparedness sta 2,300 2,100 2,400
Public health physician 1,300 900 1,600
Public information professional 600 550 700
Registered nurse 21,200 18,800 23,700
NACCHO | 2019 National Prole of Local Health Departments
58
CHAPTER
5 Workforce

Technical note
This diagram depicts the overall composition of the LHD
workforce across the United States. The area of each box
corresponds to the fraction of the LHD workforce that
comprises the occupation. Estimates for overall workforce
composition are approximated using occupational
categories that were included in the survey questionnaire,
which is not exhaustive of all LHD occupations.
Figure 5.12 | Workforce composition
More than one-third of the LHD workforce
is composed of oce and administrative
support sta or registered nurses.
Twelve percent of the LHD workforce is
environmental health workers.
A total of less than 15% of the LHD
workforce comprises oral healthcare
professionals, information systems
specialists, epidemiologists/statisticians,
preparedness sta, public health
physicians, laboratory workers,
animal control workers, and public
informationprofessionals.
n=1,110–1,129
Agency leadership
5%
Community health worker
5%
Behavioral health sta
6%
Business and nancial operations sta
7%
Epidemiologist/
statistician
2%
Information systems
specialist
2%
Licensed practical
or vocational nurse
3%
Environmental health worker
12%
Animal
control
0.8%
Public
info pro
0.5%
Laboratory worker
2%
Registered nurse
18%
Nutritionist
4%
Nursing aide and home
health aide
2%
Oral health care
professional
2%
Oce and administrative support sta
19%
Health educator
6%
Preparedness sta
2%
Public health
physician
1%
NACCHO | 2019 National Prole of Local Health Departments
59
CHAPTER
5 Workforce

2008 2010 2013 2016 2019
n=1,942 n=1,825 n=1,680 n=1,596 n=1,114
33,200
28,300
25,800
23,600
21,200
Registered nurses
2008 2010 2013 2016 2019
n=1,831 n=1,766 n=1,272 n=1,627 n=1,128
7,900
5,800
3,700 3,700
6,700
Behavioral health sta
2008 2010 2013 2016 2019
n=1,731 n=1,627 n=1,219 n=1,610 n=1,126
1,300
2,000
1,800
2,600
2,900
Epidemiologist/statistician
2008 2010 2013 2016 2019
n=1,942 n=1,645 n=1,349 n=1,565 n=1,105
1,100
2,900
2,900
2,200
2,300
Preparedness sta
Number of Full-Time Equivalents (FTEs)
Figure 5.13 | Estimated size of select occupations, over time
The estimated number of registered nurses
decreased by 36% from 2008 to 2019.
In 2013 and 2016, the estimated number of
behavioral sta decreased by more than half,
compared to 2008. However, this occupation
experienced some growth in 2019, with an
estimated 3,000 FTEs added since 2016.
The estimated number of epidemiologists and
preparedness sta more than doubled from 2008
to2019.
NACCHO | 2019 National Prole of Local Health Departments
60
CHAPTER
5 Workforce

23%
18%
30%
37%
27%
20%
37%
All LHDs
Size of population served
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
Type of governance
State
Local
Shared
Percent of LHDs reporting jobs lost
n=1,451
Figure 5.14 | Job losses among LHDs due to layos and/or attrition in the past year, by size of population served
andtype of governance
Twenty-three percent of LHDs reported
at least one job lost during calendar year
2018, due to layos and/or attrition.
A larger proportion of large and medium
LHDs reported losing at least one job
compared to small LHDs.
Similarly, LHDs with shared governance
were more likely to report losing at least
one job compared to state-governed or
locally governed LHDs.
Technical note
The 2019 Prole included questions about loss of LHD sta
(by layos or attrition) during calendar year 2018. Similar
questions have been included in 12 other NACCHO surveys
administered periodically since the beginning of the Great
Recession. Figures 5.14 through 5.16 present ndings based
on these data from 2019 and earlier surveys.
NACCHO | 2019 National Prole of Local Health Departments
61
CHAPTER
5 Workforce

n=432–437 n=1,895–1,938 n=620–631 n=646–664 n=1,780–1,778 n=555–570 n=563 n=1,451
44%
36%
38%
34%
27%
34%
32%
23%
2011 20142013 2015 2016 2017 2018 2019
Percent of LHDs reporting jobs lost
Figure 5.15 | Job losses among LHDs due to layos and/or attrition, over time
Since 2011, the percentage of LHDs
reporting at least one job lost due to
layos and/or attrition has decreased.
While 44% of LHDs reported losing at least
one job during the 2010 calendar year,
23% of LHDs reported losing at least one
job during the 2018 calendaryear.
Technical notes
N’s vary because questions regarding layos and attrition
were asked in separate questions with dierent numbers
ofobservations across survey years.
The 2019 Prole included questions about loss of LHD sta
(by layos or attrition) during calendar year 2018. Similar
questions have been included in 12 other NACCHO surveys
administered periodically since the beginning of the Great
Recession. Figures 5.14 through 5.16 present ndings based
on these data from 2019 and earlier surveys.
NACCHO | 2019 National Prole of Local Health Departments
62
CHAPTER
5 Workforce

Technical notes
This gure summarizes data on numbers of LHD positions
added and eliminated during ve calendar years. The
net change is the number of positions added, minus the
number of positions eliminated. Net loss gures are
shown in orange and net gain gures in green.
The 2019 Prole included questions about loss of LHD sta
(by layos or attrition) during calendar year 2018. Similar
questions have been included in 12 other NACCHO surveys
administered periodically since the beginning of the Great
Recession. Figures 5.14 through 5.16 present ndings based
on these data from 2019 and earlier surveys.
NACCHO estimated 2011 statistics using data from two
surveys in which LHDs reported jobs lost and added: in
January through June 2011 (labeled as Jun 2011) and July
through December (labeled as Jan 2012).
Estimates for 2008–2013 workforce are dierent from
previous reports due to new weighing and cleaning
methodologies. Refer to page 17 for more information on
the methodology.
Only LHDs who reported values for all variables on job cuts
and additions are included in the analysis.
n(Jun 2011)=604 n(Jan 2012)=617 n(2012)=1,773 n(2015)=1,261 n(2017)=545 n(2018)=1,424
Figure 5.16 | Number of jobs lost and added, over time and by size of population served
Among all LHDs, there was a net loss
of 6,270 jobs in the 2011 calendar year;
the net job loss decreased to 410 jobs in
2012. In 2018, the number of jobs added
exceeded the number of jobs eliminated,
for a net increase of 2,150 jobs across
allLHDs.
During 2018, small and large LHDs showed
net gains of 200 and 990 sta, respectively.
Meanwhile, medium LHDs showed a net
loss of 500 sta.
Number of positions eliminated Number of positions added Net change
All LHDs
Change in 2011 9,970 3,700 -6,270
Change in 2012 4,090 3,680 -410
Change in 2015 2,720 3,570 850
Change in 2017 730 900 170
Change in 2018 2,590 4,740 2,150
Small LHDs (<50,000)
Change in 2011 2,200 600 -1,600
Change in 2012 820 620 -200
Change in 2015 620 720 100
Change in 2017 110 90 -20
Change in 2018 540 740 200
Medium (50,000–499,999)
Change in 2011 4,500 1,350 -3150
Change in 2012 2,030 1,650 -380
Change in 2015 1,460 1,640 180
Change in 2017 380 320 -60
Change in 2018 900 400 -500
Large (500,000+)
Change in 2011 3,270 1,740 -1,530
Change in 2012 1,240 1,400 160
Change in 2015 640 1,210 570
Change in 2017 250 490 240
Change in 2018 1,150 2,140 990
NACCHO | 2019 National Prole of Local Health Departments
63
CHAPTER
5 Workforce

Finance
CHAPTER 6
This chapter includes the following:
Total annual local health department
(LHD)expenditures.
Annual per capita LHD expenditures
andrevenues.
LHD revenue sources.
Annual per capita LHD revenue sources.
Changes in LHD budgets over time.

4% <$250,000
5% $250,000–$499,999
4% $500,000–$749,999
4% $750,000–$999,999
11% $1,000,000–$2,499,999
7% $2,500,000–$4,999,999
5% $5,000,000–$9,999,999
3% $10,000,000–$24,999,999
3% $25,000,000+
53% Not reported
Percent of LHDs
n=1,496
Figure 6.1 | Total annual expenditures
Total annual LHD expenditures range from
less than $250,000 to $25 million or more.
Seventeen percent of LHDs report annual
expenditures of less than $1 million; 3%
ofLHDs report expenditures of $25 million
ormore.
More than half of LHDs were not able
toreport their annual expenditures.
NACCHO | 2019 National Prole of Local Health Departments
65
CHAPTER
6 Finance

n=712
Figure 6.2 | Mean and quartiles of total annual expenditures
On average, LHDs spend $8.4 million per
year, or a median of almost $1.7 million
peryear.
Comparing the 25th and 75th percentiles
for each population category illustrates
the great diversity in funding levels among
LHDs serving jurisdictions of similar sizes.
Size of population served Mean 25th percentile
50th percentile
(Median) 75th percentile
All LHDs $8,380,000 $600,000 $1,660,000 $5,270,000
<25,000 $800,000 $270,000 $530,000 $980,000
25,000–49,999 $1,850,000 $680,000 $1,220,000 $2,350,000
50,000–99,999 $3,100,000 $1,330,000 $2,750,000 $3,920,000
100,000–249,999 $6,850,000 $3,400,000 $5,500,000 $8,250,000
250,000–499,999 $16,100,000 $8,040,000 $11,650,000 $20,390,000
500,000–999,999 $46,900,000 $17,110,000 $28,100,000 $52,630,000
1,000,000+ $174,000,000 $45,560,000 $62,500,000 $102,400,000
NACCHO | 2019 National Prole of Local Health Departments
66
CHAPTER
6 Finance

n(expenditures)=712
n(revenue)=701
Figure 6.3 | Median and quartiles of annual per capita expenditures and revenues,
by size of population served and type of governance
Median annual per capita expenditures
were similar to annual per capita revenues
across LHDs.
On average, LHDs serving the smallest
populations (fewer than 25,000 people)
have higher per capita revenues
and expenditures than LHDs serving
largerpopulations.
LHDs with a shared governance structure
receive and spend more on average
than LHDs with exclusively local or
stategovernance.
Expenditures Revenue
25th
percentile Median
75th
percentile
25th
percentile Median
75th
percentile
All LHDs $23 $41 $68 $22 $40 $67
Size of population served
<25,000 $23 $51 $78 $22 $53 $85
25,000–49,999 $21 $37 $66 $20 $36 $64
50,000–99,999 $22 $38 $58 $19 $38 $54
100,000–249,999 $24 $37 $53 $22 $35 $53
250,000–499,999 $23 $34 $62 $21 $36 $63
500,000–999,999 $24 $41 $68 $25 $41 $62
1,000,000+ $29 $37 $53 $27 $31 $53
Type of governance
State $22 $33 $53 $20 $31 $48
Local $21 $40 $67 $20 $39 $63
Shared $46 $73 $101 $22 $39 $66
NACCHO | 2019 National Prole of Local Health Departments
67
CHAPTER
6 Finance

Technical notes
Statistics presented in this map are computed by
summing the expenditures reported by LHDs in each
state and dividing by the total population of the reporting
jurisdictions. This reects the overall level of LHD
expenditures in the state and is a weighted average that
takes into account the population of eachjurisdiction.
State estimates were not computed using weights to
account for non-response.
LA
ID
UT
MT
WY
NM
CO
AL
FL
TN
KY
OH
NC
SD
KS
MN
IA
IL
MO
AR
OK
ND
CA
NV
WA
TX
MI
GA
HI
PA
ME
VA
VT
NH
MA
DE
DC
RI
AZ
SC
IN
NE
WI
MS
OR
AK
NY
CT
WV
MD
NJ
RI was excluded from the study
Figure 6.4 | Overall median annual expenditures per capita, by state
Overall annual LHD expenditures per
capita vary greatly by state, with LHDs in
New Mexico and Arizona spending less
than $5 per person and LHDs in Maryland,
Maine, and the District of Columbia
spending more than $100 per person.
Annual LHD expenditures per capita were
less than $30 in 17 states, $30 to $50 in 15
states, $50 to $70 in four states, and more
than $70 in eight states and the District
ofColumbia.
n <$30 n $30–$49.99 n $50–$69.99 n $70+ n Insucient expenditure data
NACCHO | 2019 National Prole of Local Health Departments
68
CHAPTER
6 Finance

Technical notes
In 2019, we used an updated post-stratication weighting
method to improve upon estimates from previous years.
This will result in some minor discrepancies between
2016 reporting of prior year data and 2019 reporting of
the samedata. Refer to page 17 for more information on
themethodology.
Additionally, the statistics for 2008, 2010, 2013, 2016 are
reestimated to reect 2019 ination rates based on the
Bureau of Labor Statistics’ Consumer Price Index. This will
also result in some discrepancies between 2019 reporting
on prior year data and 2016 reporting on prior year data.
*Ination adjusted estimates with post-stratication weights, outliers are not excluded.
2008 2010 2013 2016 2019
n=2,097 n=1,710 n=1,517 n=1,287 n=712
$44
$50
$43
$42
$41
$80
$69
$62
$59
$56
Mean
Median
Figure 6.5 | Median and mean* annual per capita expenditures, over time
Over time, average LHD expenditures per
capita have decreased 30%, from $80 in
2008 to $56 in 2019.
On the other hand, median per capita
expenditures increased between 2008
and 2010 (from $44 to $50), but then
decreased 18% between 2010 and 2019
(from $50 to $41).
NACCHO | 2019 National Prole of Local Health Departments
69
CHAPTER
6 Finance
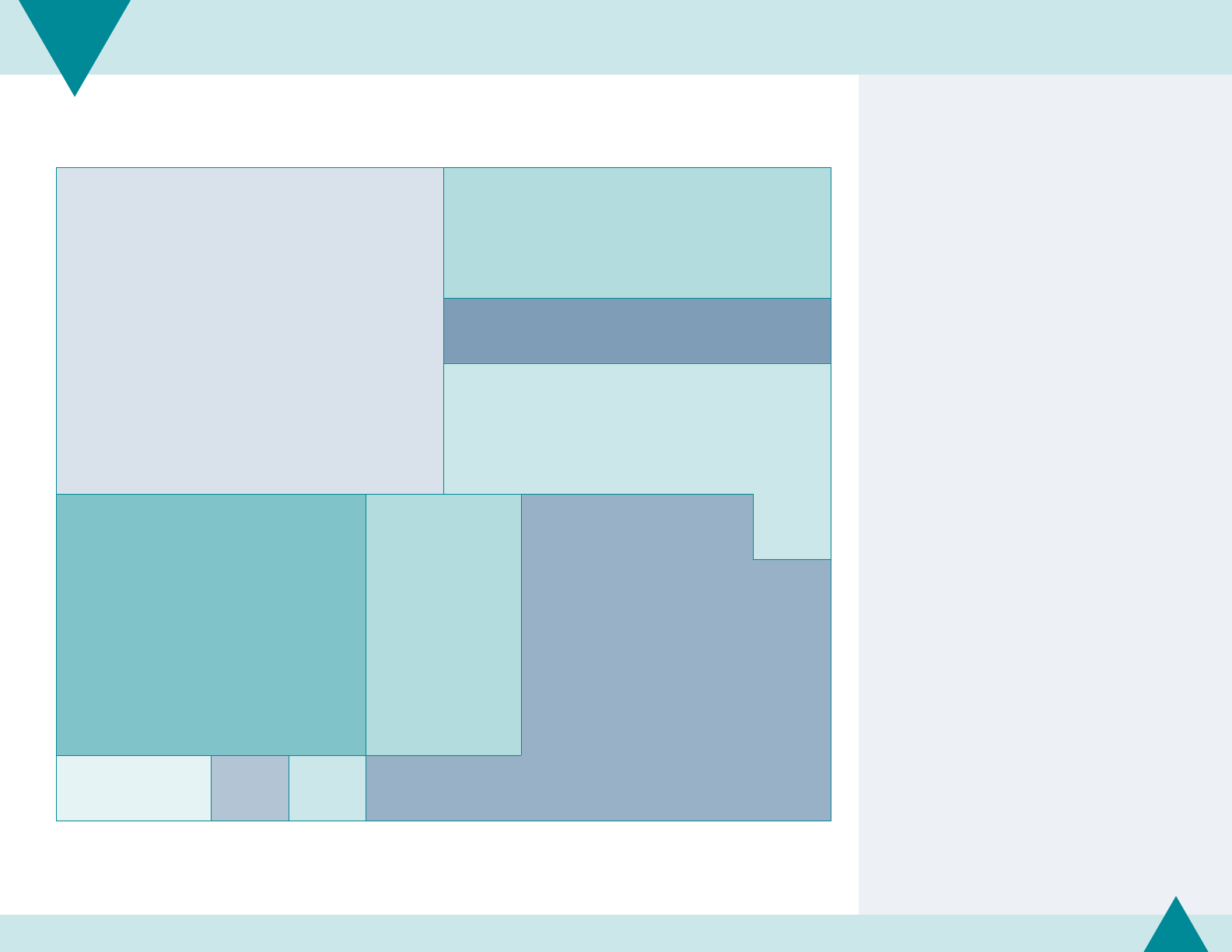
Technical note
This diagram depicts the overall composition of LHD
revenue sources. The area of each box corresponds to
thefraction of all revenues that source provides.
n=391–597
Figure 6.6 | Revenue sources
LHDs receive funding from a variety
ofsources, including local, state, federal,
andclinical sources.
One-fourth of LHD revenues come
from local sources, and 21% come from
statesources.
Thirteen percent of LHD revenues are
payments for clinical services (Medicare,
Medicaid, private insurers, or patient
personal fees).
Local sources
25%
Medicaid/Medicare
10%
Other
5%
Federal direct
11%
Federal pass-through
16%
Non-clinical
fees/nes
8%
State sources
21%
Private health insurance
2%
Private
foundations
1%
Patient fees
1%
NACCHO | 2019 National Prole of Local Health Departments
70
CHAPTER
6 Finance

*Includes Medicaid/Medicare, private health insurance, and patient personal fees.
n=365–510
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 6.7 | Median and mean annual per capita revenue sources, by LHD characteristics
On average, small LHDs receive more
per capita from non-federal sources than
medium and large LHDs.
LHDs with shared governance receive
more per capita from non-local sources
than LHDs with exclusively local or state
governance. Locally governed LHDs
receive more per capita from local sources
than state-governed LHDs or LHDs with
shared governance.
Rural LHDs receive more per capita from
allsources than urban LHDs. The dierence
in clinical revenues among rural and urban
LHDs is particularly striking (mean of $21
per capita for rural jurisdictions versus $6
per capita for urban jurisdictions).
LHDs in the South receive less per capita
from local sources than LHDs in other
regions; LHDs in the West receive more per
capita from state and federal sources than
LHDs in other regions. LHDs in the South
and Midwest receive more per capita from
clinical sources than LHDs in the Northeast
or West.
Local State
Federal direct
andpass-through Clinical*
Median Mean Median Mean Median Mean Median Mean
All LHDs $11 $18 $6 $14 $8 $13 $4 $13
Size of population served
Small (<50,000) $13 $20 $7 $16 $9 $17 $8 $18
Medium (50,000–499,999) $9 $14 $6 $10 $8 $10 $3 $8
Large (500,000+) $9 $19 $6 $11 $10 $19 $2 $7
Type of governance
State $1 $3 $5 $9 $8 $12 $4 $6
Local $13 $21 $5 $12 $8 $13 $3 $12
Shared $12 $15 $13 $26 $14 $24 $8 $25
Degree of urbanization
Urban $10 $17 $5 $9 $7 $10 $2 $6
Rural $12 $19 $9 $19 $11 $19 $9 $21
Census region
Northeast $18 $18 $2 $7 $1 $3 $0 $2
Midwest $21 $21 $4 $8 $8 $13 $5 $16
South $14 $14 $9 $16 $10 $17 $6 $19
West $19 $19 $7 $33 $15 $25 $2 $7
NACCHO | 2019 National Prole of Local Health Departments
71
CHAPTER
6 Finance

Technical notes
In 2019, we used an updated post-stratication weighting
method to improve upon estimates from previous years.
This will result in some minor discrepancies between 2016
reporting of prior year data and 2019 reporting of the
samedata.
Additionally, the statistics for 2008, 2010, 2013, 2016 are
reestimated to reect 2019 ination rates based on the
Bureau of Labor Statistics’ Consumer Price Index. This will
also result in some discrepancies between 2019 reporting
on prior year data and 2016 reporting on prior year data.
$19
23
$17
$13
$13
$5
$6
$5
$4
$4
2008 2010 2013 2016 2019
n=1,622–1,664 n=1,408–1,533 n=1,387–1,549 n=1,098–1,251 n=356–510
Clinical*
$14
Mean
Median
Mean
Median
Mean
Median
Mean
Median
State
$10
$14
$14
$8
$7
$6
$6
2008 2010 2016 2019
n=1,622–1,664 n=1,408–1,533 n=1,098–1,251 n=356–510
$8
$12
Federal direct and pass-through
$13
$12
$9
$8
$8
$13
2008 2010 2016 2019
n=1,622–1,664 n=1,408–1,533 n=1,098–1,251 n=356–510
$14
$15
$15
$15
$18
$9
$11
$9
$10
$11
2008 2010 2013 2016 2019
n=1,622–1,664 n=1,408–1,533 n=1,387–1,549 n=1,098–1,251 n=356–510
Local
*Includes Medicaid/Medicare, private health insurance, and patient personal fees.
Figure 6.8 | Median and mean annual per capita revenue sources, over time
Average per capita revenues from local sources
remained relatively consistent between 2008 and 2016.
Between 2016 and 2019, average per capita revenues
from these sources increased by 20%.
For state and federal sources (direct and passed
through by state agencies), average per capita revenues
in 2019 were similar to those in 2008.
On the other hand, average per capita revenues from
clinical sources have decreased by 32% since 2008.
NACCHO | 2019 National Prole of Local Health Departments
72
CHAPTER
6 Finance

27%
45%
44%
45%
41%
27%
28%
23%
23%
23%
21%
15%
26%
16%
25%
11% 11%
25%
19%
21%
29%
20%
23%
33%
Percent of LHDs reporting a lower budget in the current scal year
Percent of LHDs reporting a higher budget in the current scal year
2008 2010 2013 2016 2019
n=1,079
2009
n=608 n=687–
1,891
2011
n=663
2012
n=651 n=1,886
2014
n=621
2015
n=666 n=1,665
2017
n=588
2018
n=567 n=1,364
Technical note
The 2019 Prole included questions about budget changes
relative to the previous scal year. Similar questions have
been included in 12 other NACCHO surveys administered
periodically since the beginning of the Great Recession.
Figures 6.9 and 6.10 present ndings based on those data.
Figure 6.9 | Changes in LHD budgets, over time
NACCHO has tracked changes in budgets
at LHDs since 2008. From 2009 and 2012,
between 41% and 45% of LHDs reported
having a lower budget compared to the
previous scal year. In recent years, fewer
LHDs have reported budget cuts; 15%
of LHDs reported having a lower budget
in2019.
On the other hand, the percent of LHDs
reporting a higher budget compared to
the previous scal year has slowly started
to increase over time. While only 11%
reported a higher budget in 2011 and
2012, 33% of LHDs reported a higher
budget in 2019.
NACCHO | 2019 National Prole of Local Health Departments
73
CHAPTER
6 Finance

85% No budget cut
6% 1–2.9% of budget cut
3% 3–4.9%
2% 5–9.9%
3% 10% or more of budget cut
Percent of LHDs
n=1,361
Figure 6.10 | Percent of LHD’s budget cut in the current scal year compared to the previous scal year
While most LHDs did not report a lower
budget compared to the previous scal
year, 5% of LHDs reported their budget
was cut by at least 5%.
Technical notes
The data reported in this chapter should be interpreted with
some caution. Collecting error-free data on LHD nancing
across the United States remains challenging. Large
amounts of missing data from the 2019 Prole study led to
a greater degree of approximation than was necessary for
other chapters of this report.
Five states (Delaware, Hawaii, Mississippi, South Dakota,
Vermont) had insucient nance data, so reliable state-level
estimates cannot be developed for per capita expenditures.
Data for the District of Columbia were not included in the
analysis of total expenditures, total revenues, and revenues
from various sources, because its status as both a local and
state health department results in extreme values relative to
other LHDs.
Comparisons with statistics from past Prole studies should
be made with caution, especially for subgroups (e.g., state-
governed LHDs, LHDs from certain states, or LHDs serving
large jurisdictions). Some of the observed dierences from
year-to-year result from a large dierence in the group of
LHDs that provided nancial data in each Prole year.
The 2019 Prole included questions about budget changes
relative to the previous scal year. Similar questions have
been included in 12 other NACCHO surveys administered
periodically since the beginning of the Great Recession.
Figures 6.9 and 6.10 present ndings based on those data.
NACCHO | 2019 National Prole of Local Health Departments
74
CHAPTER
6 Finance

This chapter includes the following:
Clinical and population-based programs
andservices provided in the past year.
Programs and services most likely to be
provided in rural or urban jurisdictions.
Programs and services provided by more
or fewer local health departments (LHDs)
compared with 2008.
Change in level of LHD service provision
in the past year.
Programs and Services
CHAPTER 7

n=1,226–1,461
Figure 7.1 | Clinical programs and services provided directly by LHDs in the past year
LHDs provide many dierent types of
clinical programs and services directly,
including adult and child immunizations,
screening and treatment for chronic and
communicable diseases or conditions,
andmaternal and child health services.
Adult and child immunizations are the
clinical services most often provided
byLHDs.
The proportion of LHDs providing
other clinical services varies greatly;
only 11% provide comprehensive
primary care services, while 86% provide
tuberculosisscreening.
Program/service % of LHDs
Immunization
Childhood immunizations 88%
Adult immunizations 88%
Screening for diseases/conditions
Tuberculosis 86%
Other STDs 70%
HIV/AIDS 62%
High blood pressure 56%
Body Mass Index (BMI) 52%
Diabetes 39%
Cancer 31%
Cardiovascular disease 25%
Treatment for communicable diseases
Tuberculosis 83%
Other STDs 52%
HIV/AIDS 46%
Program/service % of LHDs
Maternal and child health services
Women, Infants, and Children (WIC) 68%
Early and periodic screening, diagnosis, and treatment 38%
Well child clinic 30%
Prenatal care 30%
Other clinical services
Oral health 30%
Home health care 15%
Substance abuse 15%
Behavioral/mental health 12%
Comprehensive primary care 11%
NACCHO | 2019 National Prole of Local Health Departments
76
CHAPTER
7 Programs and Services

Technical notes
School health programs may include both clinical services
and populated-based prevention programs.
LHD laboratories may test clinical or environmental
specimens; the Prole questionnaire includes a single item
intended to include both types.
n=1,136–1,466
Figure 7.2 | Population-based programs and services provided directly by LHDs in the past year
LHDs also provide many dierent types
of population-based programs and
services directly, including epidemiology
and surveillance; primary prevention;
regulation, inspection, or licensing; and
environmental health services.
The most common population-based
programs and services provided across
LHDs include communicable/infectious
disease surveillance, environmental
health surveillance, population-based
tobacco prevention services, regulation
of food service establishments, food
safety education, and population-based
nutritionservices.
Program/service
% of
LHDs
Epidemiology and surveillance
Communicable/infectious
disease
90%
Environmental health 84%
Maternal and child health 70%
Syndromic surveillance 65%
Chronic disease 51%
Behavioral risk factors 47%
Injury 37%
Population-based primary prevention
Tobacco 78%
Nutrition 75%
Chronic disease programs 60%
Physical activity 59%
Opioids 45%
Injury 40%
Substance abuse
(other than opioids)
37%
Mental illness 18%
Program/service
% of
LHDs
Regulation, inspection, and/or licensing
Food service establishments 78%
Schools/daycare 72%
Septic systems 68%
Recreational water (e.g., pools,
lakes, beaches)
66%
Body art (e.g., tattoos, piercings) 58%
Private drinking water 56%
Children’s camps 55%
Hotels/motels 55%
Lead inspection 52%
Campgrounds & RVs 49%
Health-related facilities 42%
Tobacco retailers 41%
Food processing 41%
Public drinking water 37%
Housing (inspections) 33%
Milk processing 11%
Program/service
% of
LHDs
Other environmental health services
Food safety education 78%
Public health nuisance
abatement
72%
Vector control 55%
Indoor air quality 32%
Hazmat response 23%
Land use planning 19%
Air pollution 19%
Radiation control 16%
Noise pollution 16%
Other population-based services
School health 37%
Laboratory services 33%
School-based clinics 29%
Animal control 17%
Emergency medical services 4%
NACCHO | 2019 National Prole of Local Health Departments
77
CHAPTER
7 Programs and Services

n=1,451–1,461
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 7.3 | Adult and child immunization services provided directly by LHDs in the past year, by size of population
served and degree of urbanization
Most LHDs provide adult and child
immunizations, regardless of jurisdiction
size or degree of jurisdiction urbanization.
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Childhood immunizations 88% 86% 92% 90% 81% 96%
Adult immunizations 88% 86% 91% 92% 80% 93%
NACCHO | 2019 National Prole of Local Health Departments
78
CHAPTER
7 Programs and Services

n=1,411–1,447
Figure 7.4 | Screening and treatment for diseases and conditions provided directly by LHDs in the past year,
by size of population served and degree of urbanization
LHDs are more likely to provide screening
for chronic and communicable diseases/
conditions than treatment. For example,
62% of LHDs screen for HIV/AIDS, while
46% provide treatment services for
HIV/AIDS.
Medium and large LHDs are more likely to
provide screening and treatment services,
with the exception of screening for high
blood pressure and BMI.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Screening for diseases/conditions
Tuberculosis 86% 83% 89% 95% 91% 81%
Other STDs 70% 64% 75% 95% 65% 74%
HIV/AIDS 62% 54% 71% 92% 59% 65%
High blood pressure 56% 59% 51% 59% 51% 61%
Body Mass Index (BMI) 52% 52% 50% 61% 45% 58%
Diabetes 39% 37% 40% 50% 37% 41%
Cancer 31% 28% 34% 43% 31% 31%
Cardiovascular disease 25% 24% 27% 32% 26% 25%
Treatment for communicable diseases
Tuberculosis 83% 81% 86% 91% 77% 90%
Other STDs 52% 62% 73% 91% 63% 71%
HIV/AIDS 46% 43% 50% 55% 41% 51%
NACCHO | 2019 National Prole of Local Health Departments
79
CHAPTER
7 Programs and Services

n=1,226–1,455
Figure 7.5 | Maternal and child health services provided directly by LHDs in the past year, by size of population
served and degree of urbanization
Many LHDs provide WICservices. However,
the proportion of LHDs directly providing
WIC varies by the degree of jurisdiction
urbanization. Specically, LHDs in rural
areas are more likely to provide this service
than those in urban areas.
Fewer LHDs provide other direct clinical
services to mothers and children, such as
EPSDT, well child clinics, and prenatal care.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Women, Infants, and Children (WIC) 68% 64% 71% 82% 59% 76%
Early and periodic screening,
diagnosis, and treatment (EPSDT)
38% 41% 37% 27% 29% 48%
Well child clinic 30% 30% 29% 31% 26% 34%
Prenatal care 30% 28% 32% 31% 25% 35%
NACCHO | 2019 National Prole of Local Health Departments
80
CHAPTER
7 Programs and Services
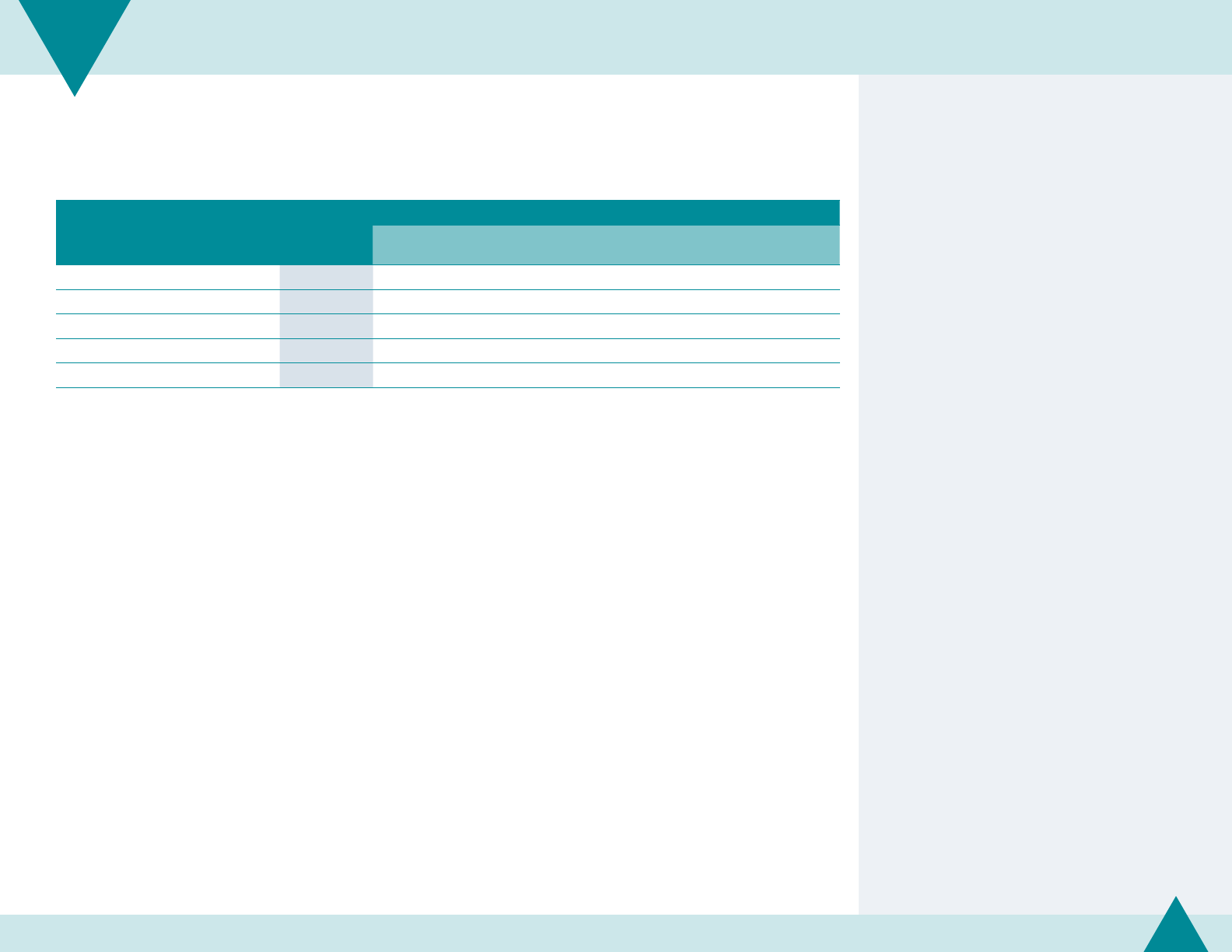
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 7.6 | Other clinical services provided directly by LHDs in the past year, by size of population served and degree
of urbanization
Few LHDs provide other clinical services,
such as home health care, substance
abuse services, behavioral/mental health
services, or comprehensive primary care.
With the exception of home health care,
large LHDs are more likely to provide these
services than small or medium LHDs.
n=1,434–1,453
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Oral health 30% 26% 36% 49% 30% 31%
Home health care 15% 18% 11% 11% 11% 19%
Substance abuse 15% 13% 18% 24% 16% 14%
Behavioral/mental health 12% 9% 16% 22% 10% 13%
Comprehensive primary care 11% 8% 14% 15% 11% 10%
NACCHO | 2019 National Prole of Local Health Departments
81
CHAPTER
7 Programs and Services

Figure 7.7 | Epidemiology and surveillance services provided directly by LHDs in the past year, by size of population
served and degree of urbanization
Almost all LHDs provide communicable/
infectious disease surveillance; most
provide environmental health surveillance,
maternal child health surveillance,
syndromic surveillance, and chronic
disease surveillance.
Large LHDs are more likely to provide
these services than small or medium LHDs.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
n= 1,246–1,466
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Communicable/infectious disease 90% 88% 94% 98% 88% 93%
Environmental health 84% 81% 90% 86% 86% 82%
Maternal and child health 70% 65% 77% 86% 65% 76%
Syndromic surveillance 65% 58% 76% 84% 67% 64%
Chronic disease 51% 45% 56% 82% 51% 50%
Behavioral risk factors 47% 41% 52% 74% 47% 47%
Injury 37% 31% 43% 64% 37% 37%
NACCHO | 2019 National Prole of Local Health Departments
82
CHAPTER
7 Programs and Services

Figure 7.8 | Population-based primary prevention services provided directly by LHDs in the past year,
by size of population served and degree of urbanization
Most LHDs provide population-based
primary prevention services focused on
tobacco use, nutrition, chronic diseases,
and physical activity.
Large LHDs are more likely to provide
these services than small or medium LHDs.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
n= 1,343–1,449
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Tobacco 78% 75% 82% 90% 76% 81%
Nutrition 75% 68% 83% 94% 71% 78%
Chronic disease programs 60% 54% 69% 82% 61% 60%
Physical activity 59% 53% 66% 72% 58% 59%
Opioids 45% 37% 55% 67% 48% 42%
Injury 40% 34% 48% 59% 40% 40%
Substance abuse (other than opioids) 37% 34% 40% 46% 37% 37%
Mental illness 18% 15% 21% 33% 20% 15%
NACCHO | 2019 National Prole of Local Health Departments
83
CHAPTER
7 Programs and Services

Figure 7.9 | Regulation, inspection, or licensing services provided directly by LHDs in the past year,
by size of population served and degree of urbanization
LHDs are most likely to provide regulation,
inspection, or licensing services of food
service establishments, schools/daycares,
septic systems, and recreational water.
With the exception of public drinking
water, LHDs serving urban jurisdictions
are more likely to provide regulation,
inspection, and/or licensing than LHDs
serving rural jurisdictions.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
n= 1,234–1,463
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Food service establishments 78% 73% 87% 83% 86% 71%
Schools/daycare 72% 66% 79% 81% 76% 67%
Septic systems 68% 65% 73% 77% 74% 63%
Recreational water (e.g., pools,
lakes,beaches)
66% 61% 75% 76% 74% 59%
Body art (e.g., tattoos, piercings) 58% 52% 68% 62% 63% 52%
Private drinking water 56% 54% 61% 55% 59% 54%
Children’s camps 55% 49% 65% 64% 64% 46%
Hotels/motels 55% 52% 60% 50% 56% 53%
Lead inspection 52% 46% 61% 64% 59% 45%
Campgrounds & RVs 49% 42% 61% 56% 51% 48%
Health-related facilities 42% 39% 45% 47% 44% 39%
Tobacco retailers 41% 39% 43% 44% 47% 34%
Food processing 41% 40% 43% 35% 42% 39%
Public drinking water 37% 33% 43% 41% 37% 37%
Housing (inspections) 33% 32% 34% 33% 42% 23%
Milk processing 11% 10% 12% 17% 12% 10%
NACCHO | 2019 National Prole of Local Health Departments
84
CHAPTER
7 Programs and Services

Figure 7.10 | Environmental health services provided directly by LHDs in the past year, by size of population served
and degree of urbanization
Approximately three-quarters of LHDs
provide food safety education and public
health nuisance abatement. Few provide
noise pollution control or radiation control.
LHDs serving urban jurisdictions are more
likely to provide these environmental
health services than LHDs serving
ruraljurisdictions.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
n=1,136–1,430
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
Food safety education 78% 74% 84% 83% 81% 75%
Public health nuisance abatement 72% 68% 77% 72% 79% 64%
Vector control 55% 49% 63% 69% 63% 46%
Indoor air quality 32% 29% 34% 46% 38% 25%
Hazmat response 23% 19% 27% 40% 27% 18%
Land use planning 19% 15% 25% 33% 25% 13%
Air pollution 19% 17% 21% 35% 26% 11%
Radiation control 16% 14% 18% 24% 18% 14%
Noise pollution 16% 14% 16% 20% 26% 4%
NACCHO | 2019 National Prole of Local Health Departments
85
CHAPTER
7 Programs and Services

Figure 7.11 | Other population-based services provided directly by LHDs in the past year, by size of population served
and degree of urbanization
More than one-third of LHDs provide
school health services. Meanwhile, only
4% of LHDs provide emergency medical
services, and almost one in ve LHDs
provide animal control services.
With the exception of school-based
clinics, large LHDs are slightly more likely
to provide these services than small or
medium LHDs.
Technical notes
School health programs may include both clinical services
and populated-based prevention programs.
LHD laboratories may test clinical or environmental
specimens; the Prole questionnaire includes a single item
intended to include both types.
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
n=1,419–1,461
Size of population served Degree of urbanization
Program/service All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+) Urban Rural
School health 37% 36% 37% 48% 34% 41%
Laboratory services 33% 27% 36% 68% 31% 34%
School-based clinics 29% 31% 27% 18% 23% 35%
Animal control 17% 17% 18% 20% 21% 13%
Emergency medical services 4% 2% 6% 10% 6% 1%
NACCHO | 2019 National Prole of Local Health Departments
86
CHAPTER
7 Programs and Services

52%
58%
46%
24%
15%
16%
16%
12%
18%
14%
25%
30%
14%
12%
13%
34%
All LHDs
Size of population served
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
More than
5 services
No services
1 service 2 to 5 services
Percent of LHDs
n=1,486
Figure 7.12 | Number of services contracted out by LHDs, by size of population served
More than half of all LHDs (and one-fourth
of large LHDs) contract out for
service (i.e., pay another organization to
perform this service on behalf of the LHD).
Only 1 % of all LHDs and 3 % of large
LHDs contract out for more than
veservices.
NACCHO | 2019 National Prole of Local Health Departments
87
CHAPTER
7 Programs and Services
4
4
s
any
do not

Technical note
LHD laboratories may test clinical or environmental
specimens; the Prole questionnaire includes a single item
intended to include both types.
n=1,383–1,453
Figure 7.13 | Programs and services provided most frequently via contracts
LHDs are most likely to contract out their
HIV/AIDS treatment or laboratory services.
Six of these services (laboratory services,
HIV/AIDS treatment, STD screening,
population-based tobacco prevention
services, STD treatment, and cancer
screening) have been among the top 10
services most likely to be contracted out
since 2005 (not shown).
Program/service
Percent of LHDs
contracting service
HIV/AIDS treatment 10%
Laboratory services 10%
HIV/AIDS screening 8%
Tuberculosis treatment 7%
Cancer screening 7%
Lead inspection 7%
Oral health 7%
STD screening 6%
STD treatment 6%
Population-based tobacco prevention services 6%
Behavioral/mental health services 6%
Tuberculosis screening 6%
Population-based primary substance use prevention 6%
Behavioral risk factor surveillance 6%
NACCHO | 2019 National Prole of Local Health Departments
88
CHAPTER
7 Programs and Services

n(2013)=1,910–1,959
n(2019)=1,343–1,449
52%
59%
66%
65%
60%
79%
84%
70%
75%
79%
81%
82%
90%
92%
Injury
Chronic disease
Nutrition
Physical activity
Tobacco
Substance abuse
Mental illness
2013 2019
Percent of LHDs reporting service provided by other organizations
Figure 7.14 | Provision of population-based primary prevention services by other organizations independent
ofLHDfunding
Since 2013, the proportion of LHDs
reporting that primary prevention
services are provided by other
organizations independent of LHD
funding increased for every activity, from
a low of an 8 percentage point increase
for mental illness prevention to a high
of a 22 percentage point increase for
injuryprevention.
NACCHO | 2019 National Prole of Local Health Departments
89
CHAPTER
7 Programs and Services

n=1,226–1,461
Urban Rural
Percent of LHDs providing service directly
81%
80%
77%
65%
59%
65%
65%
63%
59%
51%
45%
41%
29%
34%
25%
26%
11%
96%
93%
90%
76%
76%
74%
71%
61%
58%
51%
48%
41%
35%
34%
19%
Childhood immunizations
Adult immunizations
Tuberculosis treatment
Maternal and child
health surveillance
Women, Infants,
and Children (WIC)
Other STDs screening
Other STDs treatment
HIV/AIDS screening
High blood
pressure screening
Body Mass Index
(BMI) screening
HIV/AIDS treatment
Early and periodic screening,
diagnosis, and treatment
School health
Prenatal Care
Well-child clinic
Home health care
Figure 7.15 | Programs and services more likely to be provided in rural jurisdictions
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
This gure includes 17 services that rural
LHDs are more likely to provide than
urban LHDs (i.e., with dierences of at least
5percentage points and p<0.05 using
chi-square test).
Overall, LHDs serving rural jurisdictions
are more likely to provide certain clinical
services, including childhood and adult
immunizations, maternal and child health
services, and screening/treatment for
various conditions.
NACCHO | 2019 National Prole of Local Health Departments
90
CHAPTER
7 Programs and Services

81% 91%
Tuberculosis screening
71% 86%
Regulation of food
service establishments
75% 81%
Food safety education
64% 79%
Public health nuisance abatement
63% 74%
Regulation of septic systems
46% 63%
Vector control
52% 63%
Regulation of body art
(tattoos, piercings)
45% 59%
Lead inspection
59% Regulation of private drinking water 54%
42% 48%
Opioids prevention
39% 44% Regulation of health-related facilities
23% 42% Regulation of housing
25% 38%
Indoor air quality
27%
Hazmat response
18%
11% 26%
Air pollution
4% 26%
Noise pollution
25%
Land use planning
13%
13% 21%
Animal control
20%
Mental illness
15%
1% 6%
Emergency medical services
UrbanRuralPercent of LHDs providing service directly
Regulation includes inspections and/or licensing.
n=1,136–1,463
Figure 7.16 | Programs and services more likely to be provided in urban jurisdictions
This gure includes 20 services that urban
LHDs are more likely to provide than rural
LHDs (i.e., with dierences of at least 5
percentage points and p<0.05 using chi-
square test).
Overall, LHDs serving urban jurisdictions
are more likely to provide regulation,
inspection, and licensing services, as well
as environmental health services.
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
NACCHO | 2019 National Prole of Local Health Departments
91
CHAPTER
7 Programs and Services

2008 2019
n=2,251–2,292 n=1,411–1,447
72%
83%
68%
56%
60%
70%
57%
67%
42%
31%
41%
30%
35%
25% 25%
15%
20%
46%
Tuberculosis treatment
High blood pressure screening
Other STDs screening
Other STDs treatment
Cancer screening
Well child clinic
Cardiovascular disease screening
Home healthcare
HIV/AIDS treatment
Percent of LHDs providing service directly
Figure 7.17 | Change in percent of LHDs providing clinical programs and services since 2008
This gure shows the nine clinical services
for which the percentage of LHDs
providing that service directly changed by
at least 10 percentage points since 2008.
The percentage of LHDs providing four of
these nine services increased. In particular,
20% of LHDs directly provided HIV/AIDS
treatment in 2008. This has increased by
26 percentage points, to 46% of LHDs
providing this service directly in 2019.
Conversely, the percentage of LHDs
providing ve of the services decreased.
The provision of high blood pressure
screenings decreased the most, with the
percentage of LHDs providing this service
directly dropping 12 percentage points.
Technical note
The Prole questionnaire includes two sections on LHD
programs and services. One section asks LHDs to indicate
whether or not they provide that service (regardless of
scope) and a second asks LHDs to indicate how 11 service
areas have changed since the previous scal year (i.e.,
increased, reduced, did not change). Figures 7.17 and 7.18
show the change in the overall percentage of LHDs that
indicated they provided that service (regardless of scale or
scope) over time by comparing results from the 2019 Prole
to previous Proles. Figures 7.19, 7.20, and 7.21 show the
percentage of LHDs that reported how service areas have
changed in scale or scope since the previous scal year.
NACCHO | 2019 National Prole of Local Health Departments
92
CHAPTER
7 Programs and Services
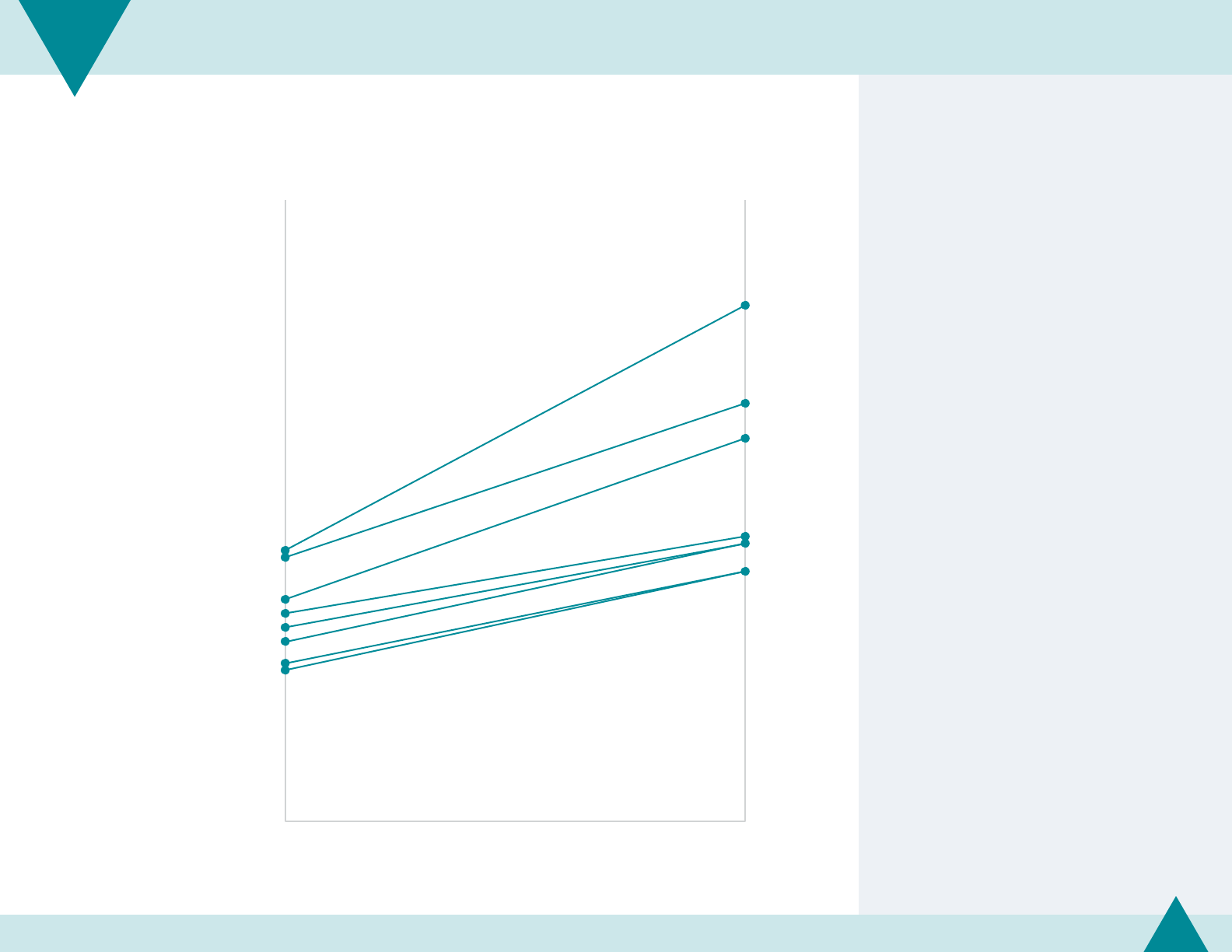
Regulation includes inspections and/or licensing.
2008 2019
n=2,256–2,285 n=1,246–1,429
Syndromic surveillance 40%
47%
Chronic disease surveillance 39%
65%
Behavioral risk factors surveillance 33%
51%
Regulation of health-related facilities 31%
41%
Regulation of food processing 29%
37%
Regulation of tobacco retailers 27%
Substance abuse prevention 24%
Injury surveillance 23%
42%
Percent of LHDs providing service directly
Figure 7.18 | Change in percent of LHDs providing population-based programs and services since 2008
This gure shows the eight population-
based services for which the percentage
of LHDs providing that service directly
changed by at least 10 percentage points
since 2008.
For all of these programs and services,
the percentage of LHDs providing them
directly increased. In particular, syndromic
surveillance provision increased by 25
percentage points, with 40% of LHDs
providing this service directly in 2008,
compared to 65% in 2019.
Technical note
The Prole questionnaire includes two sections on LHD
programs and services. One section asks LHDs to indicate
whether or not they provide that service (regardless of
scope) and a second asks LHDs to indicate how 11 service
areas have changed since the previous scal year (i.e.,
increased, reduced, did not change). Figures 7.17 and 7.18
show the change in the overall percentage of LHDs that
indicated they provided that service (regardless of scale or
scope) over time by comparing results from the 2019 Prole
to previous Proles. Figures 7.19, 7.20, and 7.21 show the
percentage of LHDs that reported how service areas have
changed in scale or scope since the previous scal year.
NACCHO | 2019 National Prole of Local Health Departments
93
CHAPTER
7 Programs and Services

Percent of LHDs that reduced services
Clinical services
9%
9%
21% Immunization
11% 18% Maternal and child health services
7% 14% High blood pressure screening
21% Diabetes screening
6% 15% Blood lead screening
4% 19% Communicable disease screening or treatment
Population-based services
5% 39%
Tobacco, alcohol, or other drug prevention
8% 16%
Obesity prevention
5% 15%
Emergency preparedness
3% 20%
Environmental health, including food safety
2% 16%
Epidemiology and surveillance
Percent of LHDs that expanded services
n=602–1,407
Figure 7.19 | Changes in provision of services in the past year
A larger proportion of LHDs expanded,
rather than reduced, both clinical and
population-based services in the past year
compared to the previous year. Expansion
was more common than reduction in all
categories, and the dierence was greater
for clinical services than for preventive
services (except tobacco, alcohol or other
drug prevention).
Notably, 39% expanded their tobacco,
alcohol, and other drug prevention
services, compared to only 5% of LHDs
that reduced these services.
Technical note
The Prole questionnaire includes two sections on LHD
programs and services. One section asks LHDs to indicate
whether or not they provide that service (regardless of
scope) and a second asks LHDs to indicate how 11 service
areas have changed since the previous scal year (i.e.,
increased, reduced, did not change). Figures 7.17 and 7.18
show the change in the overall percentage of LHDs that
indicated they provided that service (regardless of scale or
scope) over time by comparing results from the 2019 Prole
to previous Proles. Figures 7.19, 7.20, and 7.21 show the
percentage of LHDs that reported how service areas have
changed in scale or scope since the previous scal year.
NACCHO | 2019 National Prole of Local Health Departments
94
CHAPTER
7 Programs and Services

n=602–1,407
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
2%0% 4% 6% 8% 10%
14%12%
Percent of LHDs reducing service
Percent of LHDs expanding service
Immunization
Obesity prevention
Tobacco, alcohol,
other drugs
Diabetes screening
Maternal and child
health services
High blood
pressure screening
Blood lead
screening
Environmental
health
Epidemiology
and surveillance
Communicable
disease screening
or treatment
Emergency
preparedness
Average percent reduced (6%)
Average percent expanded (19%)
Clinical service Population-based service
Growing
services
Mixed
trend
Stable
services
Shrinking
services
Figure 7.20 | Growing, stable, and shrinking services in the past year
This diagram illustrates how LHDs are changing their levels
of service provision in 11 programmatic areas. The horizontal
and vertical lines represent the average percentages of LHDs
expanding and reducing services across these 11 programmatic
areas. The direction and distance from the average lines illustrate
whether programs are being expanded and reduced more or less
than average.
Programs in the lower left quadrant are stable services—those
that few LHDs are expanding or reducing. These include
epidemiology and surveillance, communicable disease
screening and treatment, and emergency preparedness.
Programs in the upper left quadrant are growing services—
those that relatively few LHDs are reducing and more are
expanding. These include tobacco, alcohol, and other drug
abuse and environmental health programs.
Programs in the lower right quadrant are shrinking services—
those that relatively more LHDs are reducing and few are
expanding. These include blood lead screening, maternal
and child health services, obesity prevention, and blood
pressurescreening.
Programs in the upper right quadrant are services where the
trends are mixed—those that relatively high percentages
of LHDs are expanding and reducing. These include
immunization and diabetesscreening.
Though most quadrants include both clinical and population-
based services, population-based services are more likely to
be stable or growing than clinicalservices.
Technical note
The Prole questionnaire includes two sections on LHD programs and
services. One section asks LHDs to indicate whether or not they provide
that service (regardless of scope) and a second asks LHDs to indicate how
11 service areas have changed since the previous scal year (i.e., increased,
reduced, did not change). Figures 7.17 and 7.18 show the change in the
overall percentage of LHDs that indicated they provided that service
(regardless of scale or scope) over time by comparing results from the 2019
Prole to previous Proles. Figures 7.19, 7.20, and 7.21 show the percentage
ofLHDs that reported how service areas have changed in scale or scope since
the previous scal year.
NACCHO | 2019 National Prole of Local Health Departments
95
CHAPTER
7 Programs and Services

n=1,041–1,296
14%
6%
10%
23%
6%
4%
16%
8%
9%
Lower budget
Same budget
Higher budget
Percent of LHDs reducing service
21%
21%
24%
19%
16%
25%
38%
32%
52%
Lower budget
Same budget
Higher budget
Percent of LHDs expanding service
Immunization
Diabetes screening
Maternal and child health services
Tobacco, alcohol, and other drug prevention
Figure 7.21 | Changes in provision of services, by changes in budgets in the past year
In general, the services that LHDs are most
likely to expand or reduce are the same
in LHDs with varying budget situations.
However, the degree to which LHDs are
expanding or reducing the programs varies
bybudgetsituation.
LHDs with lower budgets than the previous
scal year are more likely to reduce services
than LHDs with higher or unchanging budgets.
LHDs with higher budgets compared to the
previous scal year are slightly more likely to
expand and less likely to reduce services than
LHDs with lower or unchanging budgets.
In particular, LHDs are likely to expand
services related to tobacco, alcohol, and other
drug prevention regardless of changes in
theirbudgets.
Technical notes
This gure shows the three programmatic areas LHDs
were most likely to report reducing and expanding. Note
that immunization and diabetes screening appear in
bothcategories.
The Prole questionnaire includes two sections on LHD
programs and services. One section asks LHDs to indicate
whether or not they provide that service (regardless of
scope) and a second asks LHDs to indicate how 11 service
areas have changed since the previous scal year (i.e.,
increased, reduced, did not change). Figures 7.17 and 7.18
show the change in the overall percentage of LHDs that
indicated they provided that service (regardless of scale or
scope) over time by comparing results from the 2019 Prole
to previous Proles. Figures 7.19, 7.20, and 7.21 show the
percentage of LHDs that reported how service areas have
changed in scale or scope since the previous scal year.
NACCHO | 2019 National Prole of Local Health Departments
96
CHAPTER
7 Programs and Services

This chapter includes the following:
Local health department (LHD) budget
changes and sources for emergency
preparednessactivities.
Response to all-hazards events.
Source and use of volunteers in emergency
preparedness activities and emergencies.
Emergency Preparedness
andResponse
CHAPTER 8

19%
18%
20%
20%
19%
26%
10%
23%
62%
55%
71%
71%
56%
64%
61%
61%
7%
7%
5%
7%
3%
9%
4%
10%
13%
19%
4%
2%
22%
1%
25%
5%
All LHDs
Size of population served
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
Census region
Northeast
Midwest
South
West
Lower budget Approximately the same budget
Higher
budget Don't know
Percent of LHDs
n=371
Figure 8.1 | Changes in LHD budgets for emergency preparedness activities, by size of population served
and census region
Approximately one-fth of LHDs report a
lower budget for emergency preparedness
in the current scal year compared to
the previous scal year, while 7% report
ahigher budget.
The proportion of LHDs reporting a
change in emergency preparedness
budgets was similar among LHDs serving
populations of dierent sizes.
LHDs in the West and Midwest were
more likely than LHDs in South and
Northeast to report a lower budget for
emergencypreparedness.
NACCHO | 2019 National Prole of Local Health Departments
98
CHAPTER
8 Emergency Preparedness and Response

n=370
71%
24%
23%
3%
2%
10%
Federal sources passed through by state
Local sources
State sources (excluding federal pass-through)
Direct federal sources
Private foundations/grants
Do not know
Percent of LHDs
Figure 8.2 | Funding sources for emergency preparedness activities
The majority of LHDs received funding
from federal sources passed through
the state for emergency preparedness
activities.
Few LHDs received funding directly from
the federal government or through private
foundations/grants.
NACCHO | 2019 National Prole of Local Health Departments
99
CHAPTER
8 Emergency Preparedness and Response

n(2013)=484–495
n(2019)=353
2013 2019
Percent of LHDs
27%
41%
25%
30%
14%
1%
45%
41%
35%
32%
24%
10%
9%
5% 6%
1%
32%
Infectious disease outbreak other than inuenza
Natural disaster
Food-borne outbreak
Inuenza outbreak
Opioid-related event
Chemical spills or releases
Exposure to potential biological agent
Radiological release event
None
Figure 8.3 | Response to specic all-hazards events in the past year, over time
More than two-thirds of LHDs reported
responding to an all-hazards event in the
past year. This proportion has increased by
13 percentage points compared to 2013.
In 2019, LHDs most commonly responded
to outbreaks of infectious disease (other
than inuenza).
LHDs were less likely to have responded
to a natural disaster, inuenza outbreak,
chemical spills or releases, and exposure to
a potential biological agent in 2019 than
in 2013.
NACCHO | 2019 National Prole of Local Health Departments
100
CHAPTER
8 Emergency Preparedness and Response

n=353
Figure 8.4 | Response to specic all-hazards events in the past year, by size of population served
Large LHDs were almost twice as likely
as small LHDs to have responded to
an all-hazards event in the past year. In
particular, 77% of large LHDs responded
to an infectious disease outbreak (other
than inuenza), compared to 28% of
smallLHDs.
Size of population served
All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+)
Infectious disease outbreak other than inuenza 41% 28% 58% 77%
Natural disaster 35% 28% 40% 70%
Food-borne outbreak 32% 18% 50% 72%
Inuenza outbreak 24% 14% 36% 54%
Opioid-related event 10% 7% 15% 8%
Chemical spills or releases 9% 6% 10% 29%
Exposure to potential biological agent 5% 1% 10% 19%
Radiological release event 1% 1% 0% 2%
None 32% 45% 14% 2%
NACCHO | 2019 National Prole of Local Health Departments
101
CHAPTER
8 Emergency Preparedness and Response

n=353
Figure 8.5 | Response to specic all-hazards events in the past year, by census region
LHDs in the South are slightly more likely
to have responded to an all-hazards event
in the past year, compared to LHDs in
other regions. In particular, these LHDs are
approximately twice as likely to respond to
an opioid-related event.
A greater proportion of LHDs in the West
reported responding to chemical spills
or releases and exposure to a potential
biological agent.
Census region
All LHDs Northeast Midwest South West
Infectious disease outbreak other than inuenza 41% 36% 41% 41% 44%
Natural disaster 35% 28% 32% 39% 38%
Food-borne outbreak 32% 38% 34% 28% 31%
Inuenza outbreak 24% 27% 22% 23% 28%
Opioid-related event 10% 7% 9% 14% 3%
Chemical spills or releases 9% 16% 9% 4% 14%
Exposure to potential biological agent 5% 6% 4% 4% 10%
Radiological release event 1% 2% 1% 0% 0%
None 32% 31% 35% 28% 36%
NACCHO | 2019 National Prole of Local Health Departments
102
CHAPTER
8 Emergency Preparedness and Response

n=349–353
Figure 8.6 | Number of LHD responses to specic all-hazards events in the past year
For all event types, most LHDs reported
not responding.
Among LHDs that did respond to the
event type, most LHDs reported one event
in the past year. A total of 12% of LHDs
responded to four or more outbreaks of
infectious disease (other than inuenza),
and 11% responded to two natural
disasterevents.
No events 1 event 2 events 3 events
4 or more
events
Infectious disease outbreak other than inuenza 59% 21% 5% 4% 12%
Natural disaster 65% 22% 11% 2% 1%
Food-borne outbreak 68% 14% 6% 4% 7%
Inuenza outbreak 77% 11% 3% 2% 8%
Opioid-related event 91% 5% 2% 0% 2%
Chemical spills or releases 91% 5% 1% 1% 2%
Exposure to potential biological agent 95% 5% 0% 0% 0%
Radiological release event 99% 1% 0% 0% 0%
NACCHO | 2019 National Prole of Local Health Departments
103
CHAPTER
8 Emergency Preparedness and Response

n=370
55%
35%
32%
25%
12%
16%
Medical Reserve Corps (MRC)
Community Emergency Response Team (CERT)
Independent individuals
American Red Cross
Other groups
Do not engage volunteers
Percent of LHDs
Figure 8.7 | Use of select volunteer groups in emergency preparedness activities
LHDs are most likely to engage volunteers
from the Medical Reserve Corps (MRC) for
emergency preparedness activities.
A similar proportion of LHDs engage
volunteers from the Community
Emergency Response Team and
independent individuals.
Sixteen percent of LHDs do not
engage volunteers in emergency
preparednessactivities.
NACCHO | 2019 National Prole of Local Health Departments
104
CHAPTER
8 Emergency Preparedness and Response

7%
16% 15%
16%
34%
26%
47%
35%
Community Emergency
Response Team (CERT)
Do not engage volunteers
33%
29%
48%
25%
7%
16%
15%
16%
American Red Cross
Do not engage volunteers
7%
16%
15%
16%
49%
27%
65%
55%
2010
n=516
2013
n=496
2016
n=426
2019
n=370
2010
n=516
2013
n=496
2016
n=426
2019
n=370
2010
n=516
2013
n=496
2016
n=426
2019
n=370
Medical Reserve Corps (MRC)
Do not engage volunteers
Figure 8.8 | Use of select volunteer groups in emergency preparedness activities, over time
Compared to 2016, LHDs were less likely
to engage volunteers from MRC, CERT, or
American Red Cross in 2019.
However, the proportion of LHDs that
engaged volunteers from the MRC
increased overall from 49% in 2010 to 55%
in 2019. Conversely, 33% of LHDs engaged
volunteers from the American Red Cross
in 2013, compared to 25% in 2019—a
decrease of 8 percentage points.
NACCHO | 2019 National Prole of Local Health Departments
105
CHAPTER
8 Emergency Preparedness and Response

This chapter includes the following:
Local health department (LHD) participation
in a community health assessment (CHA),
community health improvement plan (CHIP),
and/or strategic plan (SP).
Data included in and elements of most
recentCHA.
Actions taken to implement or sustain a CHIP.
Level and types of collaboration with
non-prot hospitals on a community health
needsassessment.
Level of engagement with Public Health
Accreditation Board (PHAB) accreditation.
Assessment, Planning,
andAccreditation
CHAPTER 9

Technical note
In 2010, the strategic planning question was included in a
module, resulting in a lower number of respondents.
60%
70%
78%
78%
51%
55%
67%
71%
31%
43%
53%
64%
20%
30%
44%
51%
2010
n=519–2,091* n=1,939–1,964 n=1,853–1,885 n=1,477–1,482
2013 2016 2019
CHA
CHIP
SP
All three
(CHA, CHIP, & SP)
Percent of LHDs participating in CHAs, CHIPs, or SPs
Figure 9.1 | Participation over time in a community health assessment (CHA), community health improvement plan
(CHIP), and/or strategic plan (SP) within ve years
Participation in a CHA, CHIP, and SP within
the past ve years has increased among
all LHDs, compared to 2010. In particular,
LHDs were twice as likely to develop a
comprehensive, agency-wide strategic
plan in 2019. The proportion of LHDs
completing a CHA has remained steady
since 2016.
In 2019, just over half of LHDs completed
all three processes, a requirement for
PHABaccreditation.
NACCHO | 2019 National Prole of Local Health Departments
107
CHAPTER
9 Assessment, Planning, and Accreditation

n=1,477–1,482
51%
78%
71%
64%
41%
72%
64%
55%
65%
88%
79%
75%
83%
92%
92%
89%
All three (CHA, CHIP, SP)
CHA
CHIP
SP
All LHDs
Small
(<50,000)
Medium
(50,000–499,999)
Large
(500,000+)
Percent of LHD participation
Figure 9.2 | Participation in a community health assessment (CHA), community health improvement plan (CHIP),
and/or strategic plan (SP) within ve years, by size of population served
Large LHDs were the most likely to
complete a CHA, CHIP, and SP, while small
LHDs were the least likely.
NACCHO | 2019 National Prole of Local Health Departments
108
CHAPTER
9 Assessment, Planning, and Accreditation
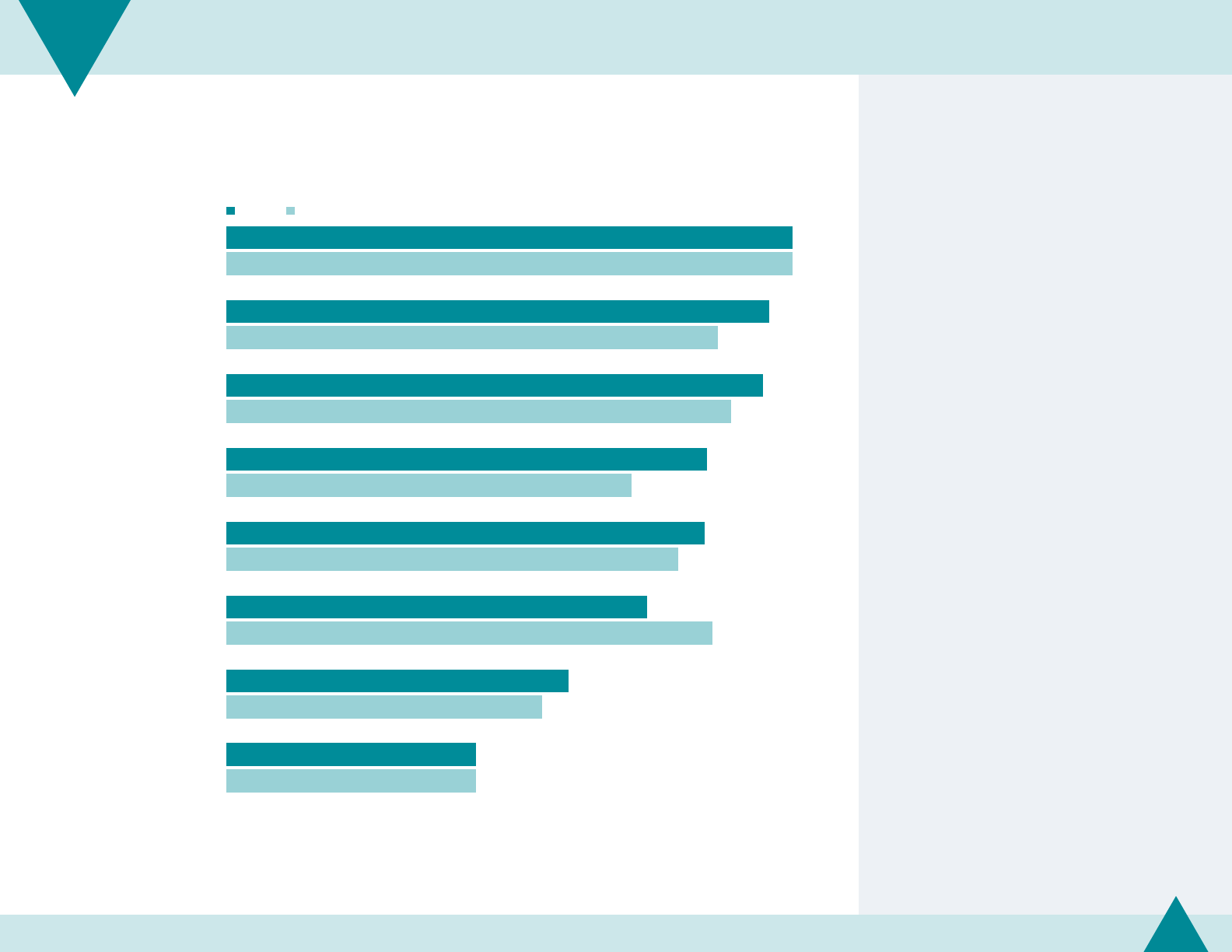
n(2016)=392
n(2019)=334
93%
89%
88%
79%
79%
69%
56%
41%
93%
81%
83%
67%
74%
80%
52%
41%
Socioeconomic characteristics
Community perceptions
of health
Social and mental health
Community attitudes
about health promotion/
improvement
Quality of life indicators
Environmental
health indicators
Built environment factors
that impact health
Policies that impact health
Percent of LHDs among those that completed a CHA
2019
2016
Figure 9.3 | Data included in most recent community health assessment (CHA), over time
LHDs use a variety of data sources in their
CHAs, including data on socioeconomic
characteristics, community perceptions
of health, and social and mental health.
LHDs are less likely to use data on the built
environment factors that impact health or
data on policies that impact health.
Compared to 2016, a greater proportion
of LHDs are using data on community
perceptions of health, social and mental
health, and community attitudes about
health promotion/improvement.
Conversely, the proportion of LHDs using
environmental health indicators in their
CHAs decreased by 11 percentage points
from 2016 to 2019.
NACCHO | 2019 National Prole of Local Health Departments
109
CHAPTER
9 Assessment, Planning, and Accreditation

87%
62%
39%
37%
29%
Healthy People 2020
Mobilizing for Action through
Planning and Partnerships (MAPP)
National Public Health Performance
Standards Program (NPHPSP)
State-specic tool
Other planning tool
Percent of LHDs among those that completed a CHIP within ve years
n=650–1,023
Figure 9.4 | Use of tools for most recent community health improvement plan (CHIP)
The most commonly selected tool LHDs
used for their most recent CHIP was
HP2020.
More than half of LHDs with a CHIP used
MAPP, while fewer LHDs used NPHPSP
orother planning tools.
LHDs were most likely to use HP2020 as
areference tool (not shown).
Large LHDs were more likely to implement
tools (rather than as a reference) than small
or medium LHDs (not shown).
NACCHO | 2019 National Prole of Local Health Departments
110
CHAPTER
9 Assessment, Planning, and Accreditation

Technical note
Missing data is due to items not being included on the 2008
Prole questionnaire.
94% 80%
Developed or strengthened
relationships with
community partners
88% 73%
Participated in a coalition(s) to
address one or more priorities
73% 61%
Established or rearmed
priorities for LHD
72% 58%
Advocated for other community
partners to establish or increase
activities to support priorities
64% 45%
Set or revisited goals for
community health outcomes
63% 45%
Set or revisited goals
for LHD performance
62%
Reported on progress toward
implementation of the plan
61%
Worked with community
partners to advance policy
changes related to priorities
56%
Developed performance measures to
monitor implementation of the plan
33% 21%
Increased LHD funding for
one or more priorities
29% 28%
Measured progress to
Healthy People 2020 goals
20192008
Percent of LHDs among those that completed a CHIP
n(2008)=315–335
n(2019)=301
Figure 9.5 | Actions taken in the past three years to implement or sustain a community health improvement
plan (CHIP), over time
LHDs take a variety of actions to
implement or sustain their CHIPs, including
developing or strengthening relationships
with community partners, participating
in a coalition to address one or more
priorities, and establishing or rearming
priorities for LHDs.
Compared to 2008, larger proportions of
LHDs have taken these actions. Notably,
nearly two-thirds of LHDs set or revisited
goals for community health outcomes and
LHD performance in 2019, compared to
less than half in 2008.
NACCHO | 2019 National Prole of Local Health Departments
111
CHAPTER
9 Assessment, Planning, and Accreditation

Technical note
The Patient Protection and Aordable Care Act (ACA)
includes a requirement that non-prot hospitals must
conduct a community health needs assessment (CHNA)
at least once every three years. The CHNA must take
into account input from persons who represent the
broad interests of the community served by the hospital,
including those with special knowledge of or expertise
inpublichealth.
63%
4%
7%
26%
Has collaborated or
is currently collaborating
Discussing future
collaboration
Not engaged in discussion
or collaboration
No non-prot hospitals
serving jurisdiction
n=1,367
Figure 9.6 | Level of collaboration with non-prot hospitals on most recent community health needs
assessment(CHNA)
Just under two-thirds of LHDs collaborated
or are currently collaborating with a
non-prot hospital on a CHNA; 4% are
discussing future collaboration; 7% are
neither collaborating nor discussing
collaboration.
One in four LHDs reported no non-prot
hospital serves their jurisdiction. One-
third of small LHDs, 14% of medium
LHDs, and 5% of large LHDs reported this
(notshown).
NACCHO | 2019 National Prole of Local Health Departments
112
CHAPTER
9 Assessment, Planning, and Accreditation

Figure 9.7 | Types of collaboration with non-prot hospitals on most recent community health needs
assessment(CHNA)
Among LHDs that are collaborating with
a non-prot hospital on a CHNA, more
than half assist in engaging community
organizations and residents in the CHNA
process, share local data resources on
health status and/or social determinants
of health, jointly conduct an assessment
that serves as both the LHD’s CHA and
hospital’s CHNA, and provide input on
strategies to improve community health.
Approximately one-third of all LHDs
collaborate with non-prot hospitals in
each of these ways.
Among all LHDs
Among LHDs
collaborating
on a CHNA
LHD provided input on strategies to improve community health 38% 63%
LHD and non-prot hospital jointly conducted an assessment that serves as both the LHD’s
Community Health Assessment and the hospital’s CHNA
36% 60%
LHD shared local data resources on health status and/or social determinants of health 35% 58%
LHD assisted in engaging community organizations and residents in CHNA process 32% 53%
LHD provided technical assistance on data collection, analysis, synthesis, or interpretation 17% 26%
LHD coordinated joint eorts by multiple hospitals to pool resources and information for a CHNA 14% 20%
LHD provided technical assistance to hospital on how to design and implement a CHNA 12% 18%
LHD served as an impartial facilitator to ensure a collaborative CHNA process 10% 16%
Not sure 2% 4%
None of the above 1% 1%
n=392 n=256
NACCHO | 2019 National Prole of Local Health Departments
113
CHAPTER
9 Assessment, Planning, and Accreditation

Technical note
The level of engagement is based on the LHD’s perception
as of July 2019 and does not reect PHAB’s most recently
accredited health departments.
n=1,426
16%
5%
2%
8%
26%
32%
11%
Accredited by PHAB
Submitted application
Registered in e-PHAB
Plans to apply, but not yet registered in e-PHAB
Undecided
Decided not to apply
Do not know
Percent of LHDs
Figure 9.8 | Level of engagement with Public Health Accreditation Board (PHAB) accreditation in 2019
In 2019, 16% of LHDs were accredited by
PHAB, which is an increase of 9 percentage
points since 2016 (not shown).
Another 7% of LHDs were engaged in
PHAB accreditation (i.e., either submitted
an application or registered in e-PHAB).
Twenty-six percent of LHDs are undecided
about PHAB accreditation, and 32%
decided not to apply. This is a shift from
LHD engagement in 2016, when 31% were
undecided and 20% decided not to apply
(not shown).
NACCHO | 2019 National Prole of Local Health Departments
114
CHAPTER
9 Assessment, Planning, and Accreditation

56%
53%
42%
34%
6%
13%
21%
26%
2013
n=448–449
2014
n=609
2016
n=1,710
2019
n=1,282
Percent of LHDs favorably
inclined towards accreditation
Percent of LHDs formally
engaged in PHAB accreditation
Figure 9.9 | Level of engagement with Public Health Accreditation Board (PHAB) accreditation, over time
The percentage of LHDs favorably inclined
towards PHAB accreditation has decreased
from 56% in 2013 to 34% in 2019.
However, the percentage of LHDs formally
engaged in PHAB accreditation has
increased from 6% in 2013 to 26% in 2019.
Level of engagement in PHAB accreditation
Formally engaged in PHAB accreditation: LHDs that are
accredited, have submitted an application or registered
ine-PHAB.
Favorably inclined towards PHAB accreditation: LHDs that
are formally engaged in PHAB accreditation or plan to apply
(all LHDs except those that are undecided or decided not
toapply for PHAB).
Technical note
This analysis excludes a number of do not know responses.
NACCHO | 2019 National Prole of Local Health Departments
115
CHAPTER
9 Assessment, Planning, and Accreditation

n=1,282
26%
13%
39%
73%
21%
12%
33%
58%
All LHDs
Size of population served
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
Percent of LHDs
2019
2016
Figure 9.10 | Formal engagement in Public Health Accreditation Board (PHAB) accreditation, over time and by size
ofpopulation served
Large LHDs are more likely to be formally
engaged in PHAB accreditation than small
and medium LHDs.
The proportion of large LHDs formally
engaged has increased by 15 percentage
points from 2016 to 2019, compared
to very small increases for small and
mediumLHDs.
Level of engagement in PHAB accreditation
Formally engaged in PHAB accreditation: LHDs that are
accredited, have submitted an application or registered
ine-PHAB.
Technical note
This analysis excludes a number of do not know responses.
NACCHO | 2019 National Prole of Local Health Departments
116
CHAPTER
9 Assessment, Planning, and Accreditation

55%
40%
36%
16%
14%
11%
18%
Fees are too high
Application requires too much time and eort
Standards exceed the capacity of my LHD
Governing body has directed LHD
not to pursue PHAB accreditation
Standards are not appropriate for LHD
Already accredited/pursuing accreditation
by another agency besides PHAB
Other reasons
Percent of LHDs among those that decided not to apply for accreditation
n=437
Figure 9.11 | Reasons for not pursuing Public Health Accreditation Board (PHAB) accreditation
In 2019, LHDs most commonly reported
that the fees are too high as the reason
they did not pursue PHAB accreditation.
LHDs were less likely to report each
reason as a factor in not pursuing PHAB
accreditation in 2019 than in 2016
(not shown). In particular, 40% of LHDs
reported that the application requires too
much time/eort in 2019 compared to
66% in 2016.
NACCHO | 2019 National Prole of Local Health Departments
117
CHAPTER
9 Assessment, Planning, and Accreditation

CHAPTER 10
This chapter includes the following:
Level of quality improvement implementation
at local health departments (LHDs).
Number of quality improvement projects.
Elements used in quality improvement eorts.
Use of core competencies for public
healthworkers.
Quality Improvement
andWorkforce Development

n=519 n=477 n=483 n=396
15%
23%
27%
36%
30%
33%
27%
25%
39%
32%
35%
29%
16%
13%
11%
9%
2010 2013 2016 2019
Formal agency-wide QI
Formal QI in specic
programmatic areas
Informal or ad hoc QI
No QI
Figure 10.1 | Level of quality improvement (QI) implementation, over time
Since 2010, the proportion of LHDs
reporting informal or no QI has decreased.
Between 2016 and 2019, the proportion
of LHDs engaged in formal QI increased
by 7 percentage points, with LHDs being
more likely to report formal agency-wide
QI programs.
NACCHO | 2019 National Prole of Local Health Departments
119
CHAPTER
10 Quality Improvement and Workforce Development

n=396
27%
45%
72%
23%
30%
24%
36%
21%
2%
2%
13%
4%
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
Percent of LHDs
Formal agency-wide QI
Formal QI in specic
programmatic areas Informal or ad hoc QI No QI
Figure 10.2 | Level of quality improvement (QI) implementation, by size of population served
Large LHDs are more likely to be involved
in formal QI programs than small or
medium LHDs.
Thirteen percent of small LHDs are not
involved in any QI at their agency, either
formal or informal.
NACCHO | 2019 National Prole of Local Health Departments
120
CHAPTER
10 Quality Improvement and Workforce Development

QI project
A systematic quality improvement initiative that includes
an aim statement; a work plan with tasks, responsibilities
and timelines; intervention strategy (ies); and measures for
tracking change
22%
58%
20%
4 or more projects 1 to 3 projects No projects
Percent of LHDs, excluding those not involved in QI activities
n=366
Figure 10.3 | Number of quality improvement (QI) projects implemented in the past year
Among LHDs involved in QI, most reported
having implemented one to three formal
QI processes in the past year.
The proportion of LHDs reporting more
than three formal QI projects in the past
year increased from 14% in 2013 (not
shown) to 22% in 2019.
NACCHO | 2019 National Prole of Local Health Departments
121
CHAPTER
10 Quality Improvement and Workforce Development

n=363
29%
7%
63%
50%
9%
42%
Formal QI
Informal QI
Percent of LHDs, excluding those not involved in QI activities
1–3 projects More than 3 projects
No projects
Figure 10.4 | Number of quality improvement (QI) projects implemented in the past year,
by level of QI implementation
LHDs with formal QI programs were more
likely to have implemented at least one
formal QI project—and four times as likely
to have implemented more than three
formal QI projects—as LHDs with only
informal QI programs.
QI project
A systematic quality improvement initiative that includes
an aim statement; a work plan with tasks, responsibilities
and timelines; intervention strategy (ies); and measures for
tracking change
NACCHO | 2019 National Prole of Local Health Departments
122
CHAPTER
10 Quality Improvement and Workforce Development

n(2013)=426
n(2019)=365
51%
51%
46%
43%
42%
40%
30%
28%
13%
40%
41%
36%
24%
31%
29%
24%
30%
20%
QI resources and training
oered on ongoing basis
Leadership dedicates resources for QI
Use performance data to
drive improvement eorts
Agency-wide QI plan
Sta member with dedicated time
QI Council
QI incorporated into job descriptions
QI incorporated into
performance appraisals
None of the above
Percent of LHDs, excluding those not involved in QI activities
2019
2013
Figure 10.5 | Elements of an agency-wide quality improvement (QI) program currently in place at LHD, over time
More than half of LHDs have QI resources
and trainings oered on an ongoing basis
at their agency and have leadership that
dedicates resources for QI. Fewer LHDs
have QI incorporated into job descriptions
or performance appraisals.
With the exception of having QI
incorporated into performance
appraisals, the proportion of LHDs with
these elements in place has increased
since2013.
QI project
A systematic quality improvement initiative that includes
an aim statement; a work plan with tasks, responsibilities
and timelines; intervention strategy (ies); and measures for
tracking change
NACCHO | 2019 National Prole of Local Health Departments
123
CHAPTER
10 Quality Improvement and Workforce Development

Technical note
The Core Competencies for Public Health Professionals
(developed by the Council on Linkages between Academia
and Public Health Practice) are a consensus set of skills for
the broad practice of public health. The Core Competencies
can provide a framework for workforce development
planning and action. More information is available at
www.phf.org/link/corecompetencies.htm
n=395
46%
31%
10%
7%
7%
41%
Core Competencies for
Public Health Professionals
Public Health Preparedness and
Response Core Competencies
Public Health Epidemiology Competency Set
Quad Council Competencies
for Public Health Nurses
Competencies for Public Health Informaticians
None
Percent of LHDs
Figure 10.6 | Use of any competency sets for workforce development, planning, and action
The most commonly used competency
set for workforce development, planning,
and action is the Core Competencies for
Public Health Professionals, with almost
half of LHDs using it. Few LHDs use
occupation-specic competency sets (e.g.,
Quad Council Competencies for Public
Health Nurses, Competencies for Public
HealthInformaticians).
Notably, 41% of LHDs do not use
any competency set for workforce
development.
Medium and large LHDs were more likely
to have used these core competency sets
than small LHDs (not shown).
NACCHO | 2019 National Prole of Local Health Departments
124
CHAPTER
10 Quality Improvement and Workforce Development

Technical note
The Core Competencies for Public Health Professionals
(developed by the Council on Linkages between Academia
and Public Health Practice) are a consensus set of skills for
the broad practice of public health. The Core Competencies
can provide a framework for workforce development
planning and action. More information is available at
www.phf.org/link/corecompetencies.htm
n=389
45%
39%
33%
22%
19%
19%
Any activity
Assessing sta training needs
Developing sta training plans
Writing position descriptions
Creating custom set of foundational
skills/core competencies for sta
Conducting sta performance evaluations
Percent of LHDs
Figure 10.7 | Use of the Core Competencies for Public Health Professionals
Almost half of LHDs have used
the Core Competencies for Public
Health Professionals for their public
healthworkers.
Most commonly, the core competencies
were used by LHDs for sta training
purposes, i.e., assessing training needs
anddeveloping training plans.
NACCHO | 2019 National Prole of Local Health Departments
125
CHAPTER
10 Quality Improvement and Workforce Development

n(2013)=470
n(2016)=462
n(2019)=389
45%
39%
33%
22%
19%
19%
34%
28%
26%
23%
26%
18%
14%
13%
14%
Any activity
Assessing sta training needs
Developing sta training plans
Writing position descriptions
Creating custom set of foundational
skills/core competencies for sta
Conducting sta performance evaluations
201920162013
Percent of LHDs
Figure 10.8 | Use of the Core Competencies for Public Health Professionals, over time
After an increase in 2013, the proportion
of LHDs using the Core Competencies for
Public Health Professionals for their public
health workers has remained the same.
In 2019, LHDs were more likely to use the
competency set to assess sta training
needs and develop sta training plans.
Conversely, a lower proportion of LHDs
used the competency set to write
position descriptions and conduct
sta performance evaluations in 2019
compared to 2016.
Technical note
The Core Competencies for Public Health Professionals
(developed by the Council on Linkages between Academia
and Public Health Practice) are a consensus set of skills for
the broad practice of public health. The Core Competencies
can provide a framework for workforce development
planning and action. More information is available at
www.phf.org/link/corecompetencies.htm
NACCHO | 2019 National Prole of Local Health Departments
126
CHAPTER
10 Quality Improvement and Workforce Development

This chapter includes the following:
Local health department (LHD) policy
development, including tobacco, alcohol,
opioids, or other drugs.
Public health ordinances and regulations.
Access to healthcare services.
Public Health Policy
CHAPTER 11

n=1,476
Figure 11.1 | Involvement in policy areas in the past two years, by size of population served
LHDs were involved in a variety of policy
areas in the past two years. LHDs were
more likely to be involved in traditional
public health policy areas (e.g., tobacco,
alcohol, opioids, or other drugs;
emergency preparedness and response;
infectious disease) than policy areas
related to social determinants of health
(e.g., safe and healthy housing, funding for
access to healthcare, land use planning).
Large LHDs were more likely to be
involved in all policy areas than small
LHDs. This dierence is greater for areas
related to the social determinants of
health than for other health-related areas.
For example, large LHDs were three times
as likely as small LHDs to be involved in
policy activities related to access to health
care and safe and healthy housing.
LHDs governed by state authorities are
less likely to be involved in policy areas
than LHDs governed by local authorities or
LHDs with shared governance (notshown).
Size of population served
All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+)
Tobacco, alcohol, opioids, or other drugs 74% 70% 79% 82%
Emergency preparedness and response 62% 62% 61% 65%
Infectious disease (e.g., vaccination) 60% 57% 60% 85%
Funding for local public health 59% 52% 68% 77%
Food safety 48% 43% 54% 62%
Obesity/physical activity 45% 41% 48% 78%
Waste, water, or sanitation 39% 38% 39% 47%
Mental health 32% 28% 37% 48%
Oral health 27% 24% 30% 44%
Injury and violence prevention 27% 21% 31% 55%
Safe and healthy housing 25% 19% 31% 54%
Funding for access to healthcare 22% 16% 30% 50%
Land use planning 14% 9% 20% 37%
Climate change 7% 4% 10% 24%
Occupational health and safety 6% 7% 5% 10%
None 9% 11% 7% 3%
NACCHO | 2019 National Prole of Local Health Departments
128
CHAPTER
11 Public Health Policy

15%
23%
25%
2013 2016 2019
n=1,936 n=1,872 n=1,476 n=1,936 n=1,872 n=1,476
n=1,936 n=1,872 n=1,476 n=1,936 n=1,872 n=1,476
Safe and healthy housing
17%
27%
32%
2013 2016 2019
Mental health
65%
74%
74%
2013 2016 2019
Tobacco, alcohol, or other drugs
28%
27%
22%
2013 2016 2019
Funding for access to healthcare
Figure 11.2 | Involvement in select policy areas, over time
Since 2013, a larger proportion of LHDs
have been involved in many policy areas.
For example, LHDs were nearly twice as
likely to be involved in mental health
policy activities.
However, LHD involvement in some policy
areas has experienced little change more
recently. The proportion of LHDs involved
in policy activities related to tobacco,
alcohol, or other drugs has increased
overall since 2013 but has remained stable
since 2016. In 2019, 25% of LHDs were
involved in safe and healthy housing
policy activities compared to 23% in 2016.
Notably, LHD involvement in policy
activities related to funding for access to
healthcare decreased by 6 percentage
points since 2013.
NACCHO | 2019 National Prole of Local Health Departments
129
CHAPTER
11 Public Health Policy

n=1,437
Figure 11.3 | Involvement in policy areas related to tobacco, alcohol, opioids, or other drugs in the past two years,
bysize of population served
In the past two years, nearly half of all
LHDs were involved in policies to reduce
the sale of tobacco to minors, while few
LHDs were involved in raising taxes on
cigarettes or alcohol.
Forty-three percent of all LHDs and more
than half of large LHDs were involved in
policies related to e-cigarette use in the
past two years.
Large LHDs were more likely to be
involved in these policy areas than small
LHDs, especially areas related to drug
abuse. For example, large LHDs were
almost three times as likely as small LHDs
to be involved in policy activities related
to increasing access to clean syringes
and diverting certain drug oenders into
treatment rather than incarceration.
LHD involvement in some policy areas
changed since 2016 (not shown). For
example, LHDs were less likely to be
involved in smoke-free indoor air policies
in 2019 (46%) compared to 2016 (57%).
The proportion of LHDs involved in
policies to increase use of medications to
prevent drug overdose increased by 22
percentage points since 2016.
Size of population served
All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+)
Reducing sale of tobacco to minors 46% 41% 51% 64%
Smoke-free indoor air (e.g., workplace, multi-unit residential) 46% 42% 48% 66%
Regulating e-cigarettes or other electronic smoking devices 43% 40% 47% 59%
Increasing use of medications to prevent drug overdose
(e.g.,Naloxone, Buprenorphine)
42% 32% 55% 66%
Smoke-free outdoor air (e.g., parks, beaches, playgrounds,
sporting events)
41% 39% 43% 51%
Reducing exposure to alcohol or tobacco advertising 23% 23% 24% 27%
Increasing access to clean syringes 18% 11% 25% 38%
Reducing alcohol or drug impaired driving 14% 15% 13% 15%
Diverting certain drug oenders into treatment rather
thanincarceration
14% 8% 22% 31%
Raising cigarette taxes 13% 12% 13% 21%
Raising alcohol taxes 2% 2% 1% 3%
NACCHO | 2019 National Prole of Local Health Departments
130
CHAPTER
11 Public Health Policy

n=1,437
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 11.4 | Involvement in policy areas related to tobacco, alcohol, opioids, or other drugs in the past two years,
bydegree of urbanization
LHDs in urban areas were more likely to
be involved in these policy areas than
LHDs in rural areas. In particular, a much
greater proportion of LHDs in urban areas
were involved in policies to divert certain
drug oenders into treatment rather than
incarceration.
Conversely, LHDs in rural areas were
more likely to reduce exposure to
alcohol or tobacco advertising and raise
cigarettetaxes.
Regardless of jurisdiction’s degree of
urbanization, approximately the same
proportion of LHDs were involved in policy
activities related to smoke-free air (indoor
and outdoor).
Degree of urbanization
All LHDs Urban Rural
Reducing sale of tobacco to minors 46% 54% 37%
Smoke-free indoor air (e.g., workplace, multi-unit residential) 46% 46% 45%
Regulating e-cigarettes or other electronic smoking devices 43% 51% 35%
Increasing use of medications to prevent drug overdose (e.g., Naloxone, Buprenorphine) 42% 47% 37%
Smoke-free outdoor air (e.g., parks, beaches, playgrounds, sporting events) 41% 42% 41%
Reducing exposure to alcohol or tobacco advertising 23% 22% 24%
Increasing access to clean syringes 18% 21% 14%
Reducing alcohol or drug impaired driving 14% 14% 15%
Diverting certain drug oenders into treatment rather than incarceration 14% 19% 10%
Raising cigarette taxes 13% 11% 14%
Raising alcohol taxes 2% 1% 2%
NACCHO | 2019 National Prole of Local Health Departments
131
CHAPTER
11 Public Health Policy

99%
97%
92%
42%
43%
41%
25%
48%
66%
2013 2016 2019
n=1,205 n=1,334 n=1,045
Tobacco
Other drugs
Alcohol
Percent of LHDs
Tobacco includes involvement in “reducing sale of tobacco
to minors,” “smoke-free indoor air,” “regulating e-cigarettes or
other electronic smoking devices,” “smoke-free outdoor air,”
“reducing exposure to alcohol or tobacco advertising,” and
“raising cigarette taxes.”
Alcohol incudes involvement in “reducing alcohol or drug
impaired driving,” “reducing exposure to alcohol or tobacco
advertising,” and “raising alcohol taxes.”
Other drugs includes involvement in “increasing use of
medications to prevent drug overdose,” “increasing access to
clean syringes,” “reducing alcohol or drug impaired driving,”
and “diverting certain drug oenders into treatment rather
than incarceration.”
Figure 11.5 | Involvement in policy areas related to tobacco, alcohol, or other drugs, over time
Since 2013, LHD involvement in policy
activities related to other drug use has
more than doubled. The proportion of
LHDs involved in tobacco use policies has
decreased slightly, while involvement in
alcohol use policies has remained steady.
NACCHO | 2019 National Prole of Local Health Departments
132
CHAPTER
11 Public Health Policy

n=1,479
44%
37%
52%
69%
18%
52%
44%
76%
43%
28%
51%
56%
32%
All LHDs
Size of population served
Small (<50,000)
Medium (50,000–499,999)
Large (500,000+)
Type of governance
State
Local
Shared
Census region
Northeast
Midwest
South
West
Degree of urbanization
Urban
Rural
Percent of LHDs
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 11.6 | Involvement in developing new or revising existing ordinances in the past two years,
byLHDcharacteristics
Forty-four percent of LHDs reported that
a new local public health ordinance or
regulation was adopted or substantially
revised in their jurisdiction during the past
two years.
Large LHDs are more likely to report new
or substantially revised ordinances or
regulations than medium or small LHDs.
LHDs governed by state authorities
are less likely to report new or revised
ordinances or regulations than LHDs
governed by local authorities or LHDs
withsharedgovernance.
LHDs in the Northeast are more likely
to report new or revised ordinances or
regulations than LHDs in other regions.
LHDs in urban areas are more likely to
report new or revised ordinances than
LHDs in rural areas.
NACCHO | 2019 National Prole of Local Health Departments
133
CHAPTER
11 Public Health Policy

n=1,466
27%
12%
9%
3%
3%
3%
2%
2%
2%
1%
1%
1%
1%
1%
0.4%
56%
Tobacco, alcohol, opioids, or other drugs
Food safety
Waste, water, or sanitation
Safe and healthy housing
Infectious disease (e.g., vaccination)
Emergency preparedness and response
Funding for local public health
Obesity/physical activity
Land use planning
Mental health
Funding for access to healthcare
Injury and violence prevention
Oral health
Climate change
Occupational health and safety
None
Percent of LHDs involved in developing new or revising existing ordinances
Figure 11.7 | Topic areas of new or revised ordinances in the past two years
More than one-quarter of LHDs report
new or substantially revised ordinances
or regulations related to tobacco,
alcohol, opioids, or other drugs in the
past two years. Few LHDs report new
or substantially revised ordinances or
regulations related to other topic areas.
NACCHO | 2019 National Prole of Local Health Departments
134
CHAPTER
11 Public Health Policy
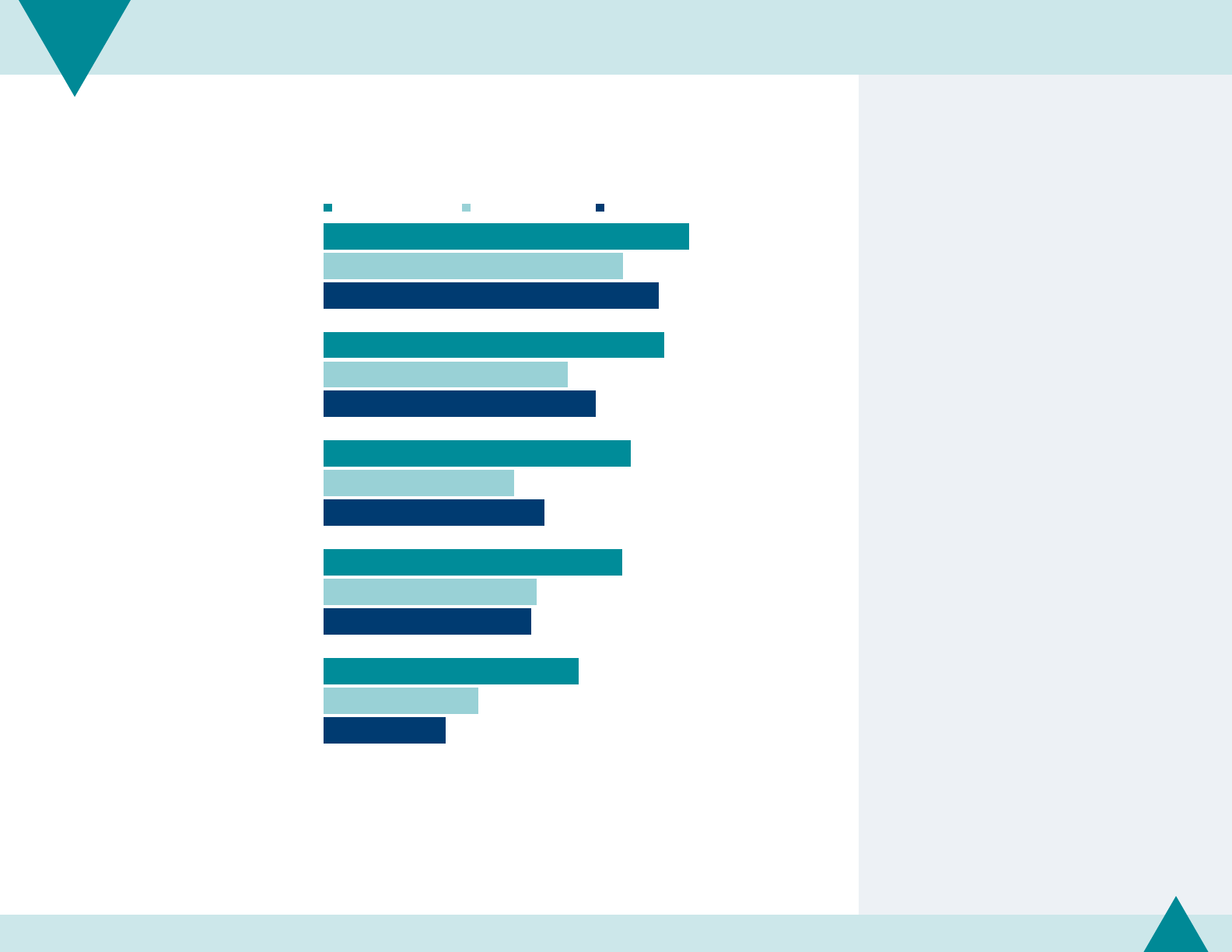
n=363–365
60%
56%
50%
49%
42%
49%
40%
31%
35%
25%
55%
44%
36%
34%
20%
Assessed the gaps in access to services
Implemented strategies to increase accessibility
of existing services (e.g., referrals)
Evaluated strategies to target healthcare
needs of underserved populations
Implemented strategies to target healthcare
needs of underserved populations
Addressed gaps through direct
provision of clinical services
Percent of LHDs
Medical services
Dental services Behavioral services
Figure 11.8 | Engagement in assuring access to healthcare services in the past year
LHDs are more likely to assure access
to medical services than dental and
behavioral services. For example, 50%
of LHDs evaluated strategies to target
medical healthcare needs of underserved
populations, while 31% evaluated
strategies to target dental healthcare
needs and 36% to target behavioral
healthcare needs.
Notably, the proportion of LHDs
implementing strategies to target
medical healthcare needs of underserved
populations decreased by 9 percentage
points since 2016 (not shown).
NACCHO | 2019 National Prole of Local Health Departments
135
CHAPTER
11 Public Health Policy

n=512 n=485 n=468 n=366
71%
73%
77%
76%
55%
51%
57%
59%
40%
47%
56%
62%
2010 2013 2016 2019
Medical
Dental
Behavioral
Percent of LHDs
Figure 11.9 | Engagement in assuring access to healthcare services, over time
The proportion of LHDs engaged in
assuring access to behavioral healthcare
services increased from 40% in 2010 to
62% in 2019, more than the increase
seen in both medical and dental
healthcareservices.
NACCHO | 2019 National Prole of Local Health Departments
136
CHAPTER
11 Public Health Policy

This chapter includes the following:
Level of implementation in information
technology systems at local health
departments (LHDs).
Use of communication channels for
general announcements or emergency
responsecommunications.
Informatics
CHAPTER 12

89%
73%
59%
53%
21%
1%
2%
8%
4%
11%
Immunization registries
Electronic disease
reporting systems
Electronic health records
Electronic lab reporting
Health information exchanges
Implemented
Implementation
in process
Percent of LHDs
n=400–401
Figure 12.1 | Level of activity in information technology systems
Most LHDs use immunization registries
and electronic disease reporting systems;
LHDs are less likely to use electronic lab
reporting, electronic health records, and
health information exchanges.
In addition, relatively large proportions of
LHDs are in the process of implementing
electronic health records and health
information exchanges.
NACCHO | 2019 National Prole of Local Health Departments
138
CHAPTER
12 Informatics

n=400–401
89%
73%
59%
53%
21%
89%
67%
53%
44%
18%
91%
82%
67%
66%
26%
83%
86%
75%
73%
31%
Immunization registries
Electronic disease reporting systems
Electronic health records
Electronic lab reporting
Health information exchanges
All LHDs
Small
(<50,000)
Medium
(50,000–499,999)
Large
(500,000+)
Percent of LHDs that have implemented technology
Figure 12.2 | Implementation of information technology systems, by size of population served
With the exception of immunization
registries, large LHDs are more likely
to have implemented most of these
technology systems than LHDs serving
smaller populations.
The dierence in implementation between
LHDs serving small and large jurisdictions
are greatest for electronic health records
and electronic lab reporting.
NACCHO | 2019 National Prole of Local Health Departments
139
CHAPTER
12 Informatics

Technical note
Missing trend data is due to items not being included in the
Prole questionnaire for the specied year.
2008 2010 2013 2016 2019
n=460–464 n=518 n=505 n=459 n=400–401
75%
85%
85%
89%
74%
79%
73%
48%
49%
53%
19%
19%
23%
37%
59%
8%
6%
14%
17%
21%
Immunization registries
Electronic disease
reporting systems
Electronic lab reporting
Electronic health records
Health information exchanges
Percent of LHDs that have implemented technology
Figure 12.3 | Implementation of information technology systems, over time
For most information technology systems,
use has increased since 2008. Notably, use
of electronic health records increased by
36 percentage points between 2013 and
2019, while use of immunization registries
and electronic lab reporting have shown
very little change.
Use of electronic disease reporting
systems has decreased since 2016,
returning to 2013 levels.
NACCHO | 2019 National Prole of Local Health Departments
140
CHAPTER
12 Informatics

n=396–397
62%
53%
53%
38%
37%
36%
30%
34%
42%
38%
44%
45%
40%
32%
58%
32%
41%
31%
38%
42%
40%
21%
8%
11%
19%
19%
33%
27%
Data management
IT hardware budget
allocation or acquisition
Software selection
IT maintenance
IT system security
Software support
Software application/
development
LHD
City/county
IT department State health agency Other vendor
Percent of LHDs with organization involved in information management
Figure 12.4 | Organizations involved in information management for LHDs
More than half of LHDs perform their own
data management, IT hardware budget
allocation or acquisition, and software
selection.
Several other organizations can be
involved in information management for
LHDs. For example, the city or county IT
department most commonly performs
functions related to LHD IT maintenance
and system security.
For many LHDs, the state health agency is
also involved in data management.
NACCHO | 2019 National Prole of Local Health Departments
141
CHAPTER
12 Informatics
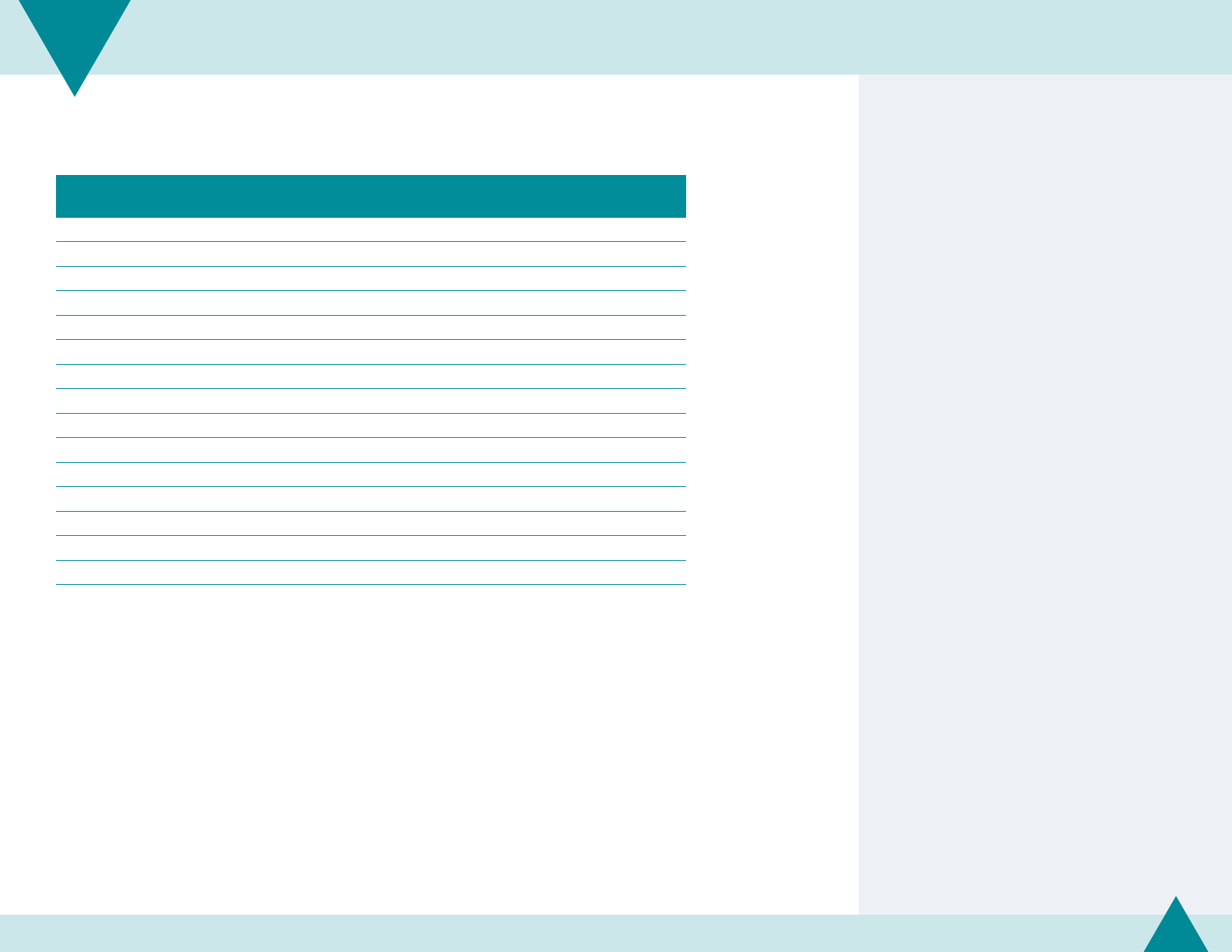
n=401
Figure 12.5 | Use of communication channels for general or emergency response communications
LHDs use a variety of information
technology channels for general
announcements or emergency response
communications. Print media, Facebook,
LHD websites, and e-mail are most
commonly used overall and are more likely
to be used for general announcements
than for emergency response. On the
other hand, LHDs are more likely to use
the Health Alert Network, automated
phone calling, and a hotline or call center
for emergency communications than for
general announcements.
Few LHDs use LinkedIn, a custom
application for phones or tablets, and
blogs for any use.
Any use
Use for general
announcements
Use for emergency
response
Print media 86% 85% 48%
Facebook 83% 80% 56%
LHD website 82% 80% 54%
E-mail 80% 75% 38%
Health Alert Network 62% 28% 53%
Broadcast media 57% 52% 45%
Text messaging 50% 44% 23%
Automated phone calling 40% 19% 29%
Fax broadcast/fax blast 37% 29% 25%
Twitter 28% 26% 19%
Other social media (e.g., YouTube, Instagram, Next Door) 27% 26% 15%
Hotline or call center 18% 8% 15%
LinkedIn 8% 8% 1%
Custom app for phone or tablet 7% 6% 4%
Blogs 6% 6% 2%
NACCHO | 2019 National Prole of Local Health Departments
142
CHAPTER
12 Informatics

n=401
Figure 12.6 | Any use of communication channels, by size of population served
Large LHDs are more likely to use the
communication channels listed than
small LHDs. In particular, a much greater
proportion of large LHDs use Twitter, other
social media channels, and a hotline or call
center to communicate with the public.
Conversely, approximately the same
proportion of LHDs use print media,
Facebook, and automated phone calling,
regardless of the size of the population
they serve.
Size of population served
All LHDs Small (<50,000)
Medium
(50,000–499,999) Large (500,000+)
Print media 86% 85% 87% 96%
Facebook 83% 81% 88% 89%
LHD website 82% 76% 91% 96%
E-mail 80% 77% 84% 98%
Health Alert Network 62% 57% 67% 85%
Broadcast media 57% 48% 69% 79%
Text messaging 50% 49% 48% 60%
Automated phone calling 40% 36% 48% 45%
Fax broadcast/fax blast 37% 33% 42% 43%
Twitter 28% 11% 49% 87%
Other social media (e.g., YouTube, Instagram, Next Door) 27% 13% 44% 71%
Hotline or call center 18% 9% 26% 61%
LinkedIn 8% 3% 13% 34%
Custom app for phone or tablet 7% 6% 7% 13%
Blogs 6% 2% 9% 27%
None 1% 1% 1% 0%
NACCHO | 2019 National Prole of Local Health Departments
143
CHAPTER
12 Informatics

n=401
Figure 12.7 | Any use of communication channels, by type of governance
With the exception of Facebook, state-
governed LHDs are less likely to use all of
the communication channels listed than
LHDs with local or shared governance.
LHDs governed by both state and local
authorities (i.e., shared governance)
are more likely to use the Health Alert
Network, broadcast media, automated
phone calling, Twitter, other social media,
a hotline or call center, and a custom
application for phones or tablets than
LHDs with state or local governance.
Type of governance
All LHDs State Local Shared
Print media 86% 65% 92% 92%
Facebook 83% 70% 90% 66%
LHD website 82% 57% 90% 86%
E-mail 80% 59% 87% 82%
Health Alert Network 62% 45% 66% 70%
Broadcast media 57% 52% 57% 66%
Text messaging 50% 40% 53% 42%
Automated phone calling 40% 30% 42% 51%
Fax broadcast/fax blast 37% 16% 42% 42%
Twitter 28% 8% 32% 42%
Other social media (e.g., YouTube, Instagram, Next Door) 27% 16% 30% 29%
Hotline or call center 18% 15% 19% 21%
LinkedIn 8% 6% 9% 7%
Custom app for phone or tablet 7% 3% 7% 8%
Blogs 6% 3% 6% 13%
None 1% 2% 0% 0%
NACCHO | 2019 National Prole of Local Health Departments
144
CHAPTER
12 Informatics
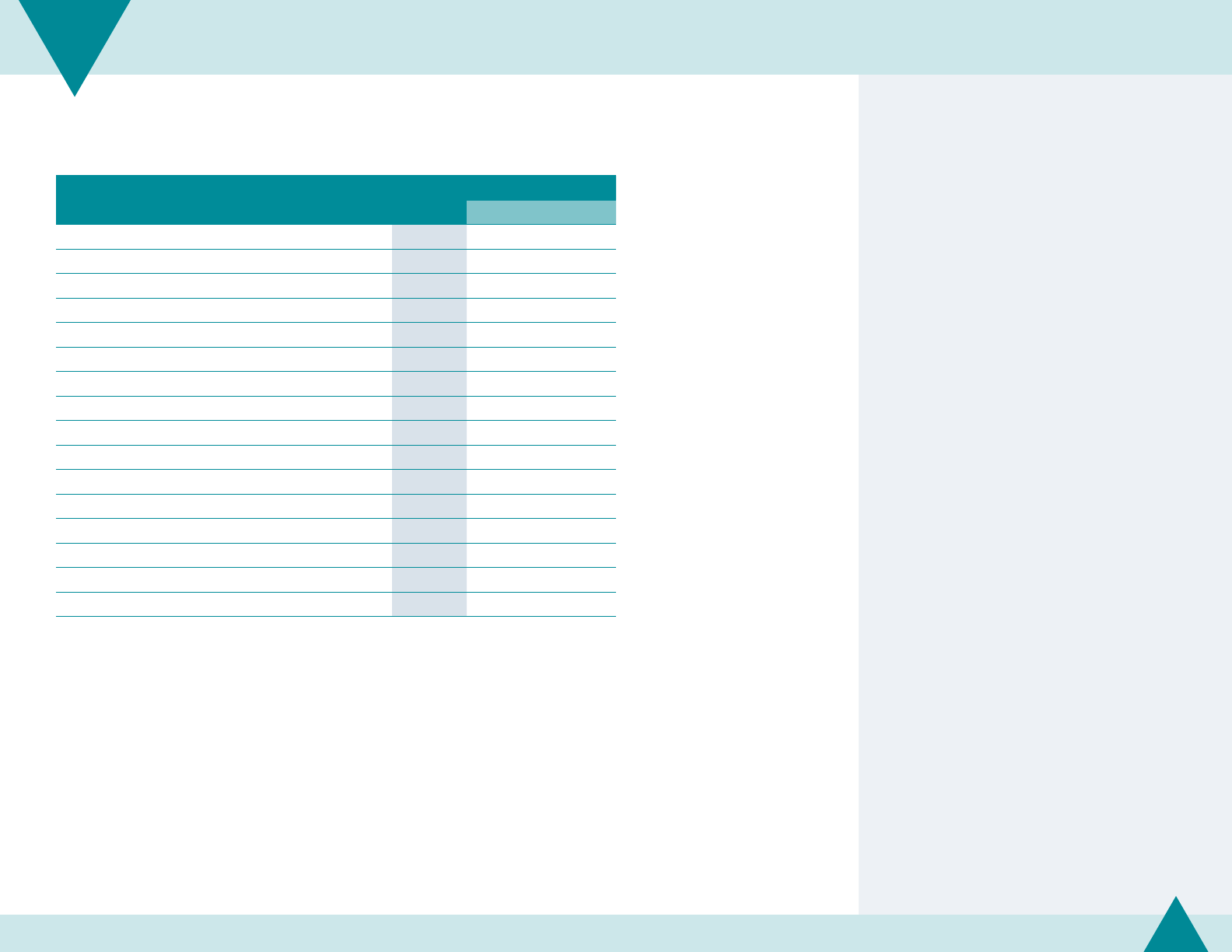
n=401
Technical note
A new schema for categorizing urban and rural LHDs was
used for 2019 estimates. These data may not be comparable
to previous year estimates. Refer to page 18 for more
information on the methodology.
Figure 12.8 | Any use of communication channels, by degree of urbanization
With the exception of Facebook and
text messaging, LHDs in urban areas are
more likely to use the communication
channels listed. In particular, a much
greater proportion of LHDs in urban areas
use Twitter, other social media, a hotline
or call center, and broadcast media to
communicate with the public.
Degree of urbanization
All LHDs Urban Rural
Print media 86% 86% 86%
Facebook 83% 82% 85%
LHD website 82% 90% 76%
E-mail 80% 87% 75%
Health Alert Network 62% 65% 59%
Broadcast media 57% 65% 49%
Text messaging 50% 44% 54%
Automated phone calling 40% 44% 36%
Fax broadcast/fax blast 37% 41% 33%
Twitter 28% 46% 11%
Other social media (e.g., YouTube, Instagram, Next Door) 27% 41% 14%
Hotline or call center 18% 27% 10%
LinkedIn 8% 15% 2%
Custom app for phone or tablet 7% 9% 5%
Blogs 6% 9% 3%
None 1% 1% 0%
NACCHO | 2019 National Prole of Local Health Departments
145
CHAPTER
12 Informatics

26%
42%
50%
35%
64%
80%
28%
43%
65%
83%
13%
17%
28%
28%
2010
n=511 n=475 n=466 n=401
2013 2016 2019
Facebook
Email
Text messaging
Twitter
Percent of LHDs
Figure 12.9 | Any use of communication channels, over time
LHD use of newer technology to
communicate with the public has
increased since 2010. For instance, use of
Facebook increased dramatically from 28%
of LHDs in 2010 to 84% in 2019.
Use of Twitter increased from 13%
in 2010 to 28% in 2016, but has not
increasedsince.
Technical note
Missing trend data is due to items not being included in the
Prole questionnaire for the specied year.
NACCHO | 2019 National Prole of Local Health Departments
146
CHAPTER
12 Informatics

The National Association of County and City Health Ocials (NACCHO) represents the nation’s
nearly 3,000 local health departments. These city, county, metropolitan, district, and tribal
departments work every day to protect and promote health and well-being for all people in their
communities. For more information about NACCHO, please visit www.naccho.org.
1201 I Street, NW, Fourth Floor
Washington, DC 20005
P 202-783-5550
F 202-783-1583
www.naccho.org
prole@naccho.org
© 2020. National Association of County and City Health Ocials.
